Obviously a v important topic.
New paper @mlipsitch @mugecevik @EdwardGoldste16. I have serious issues w/ conclusions because it ignores well-known biases, conflates infection & susceptibility, & misuses anecdotes.
Thread.
A huge Q about transmission of SARS-COV-2 is how transmission varies by age. Specifically, is there age-specific variation in either susceptibility or infectiousness?
Many ways to address this Q, but most have major challenges due to biases in how data are collected.
See end of thread for age-specific fatality estimates:
Also paper by @hsalje shows age-specific hospitalization which shows similar huge skew towards older people.
10.1126/science.abc3517
Who did parents try to shield the most? Their youngest children.
-One should not make any claims about relative susceptibility based on infection data; relative contact rates (shielding) equally (more?) likely.
-Claims about relative infection patterns are suspect because of biases due to differential symptoms
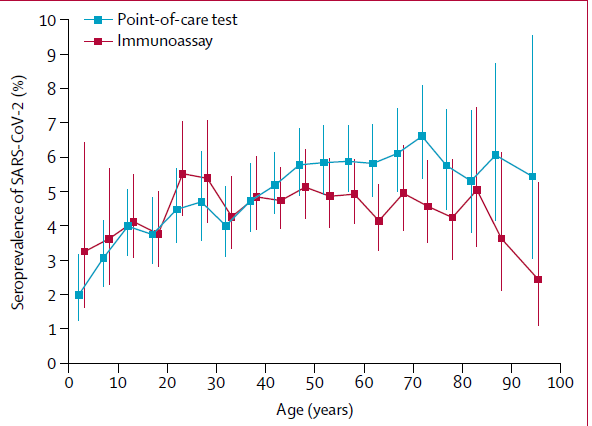
Seroprevalence studies remove one of these issues (but not the other) - differential prob of symptoms
Paper discusses serological data but strangely doesn't make figure or table. Text barely mentions children vs adults.
If lower exposure was due to lower contact rates and not lower susceptibility, then when we re-open schools transmission would be high unless protective measures are taken.
medrxiv.org/content/10.110…
nature.com/articles/s4159…
An ongoing challenge is that contact tracing studies define person w/ earlier symptom onset as index case & later as infectee.
thelancet.com/action/showPdf…
medrxiv.org/content/10.110…
I wrote about it here:
medrxiv.org/content/10.110…


Data do not support strong claim of lower susceptibility in children.
I'd argue we CANNOT make any claims about susceptibility b/c we can't separate susceptibility from contact.
I'd even caution against making claims about infection b/c biases & schools closed.(cont)
medrxiv.org/content/10.110…