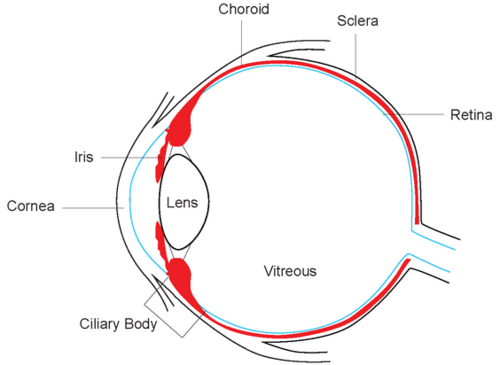
Hey everyone, the first-in-human clinical trial of tebentafusp, the HLA-specific fusion protein targeting gp100, is now online @CCR_AACR! Cool mechanistic proof of concept that you can get CD3+ cells into a poorly infiltrated tumor like #uveal #melanoma.
clincancerres.aacrjournals.org/cgi/content/ab…
clincancerres.aacrjournals.org/cgi/content/ab…
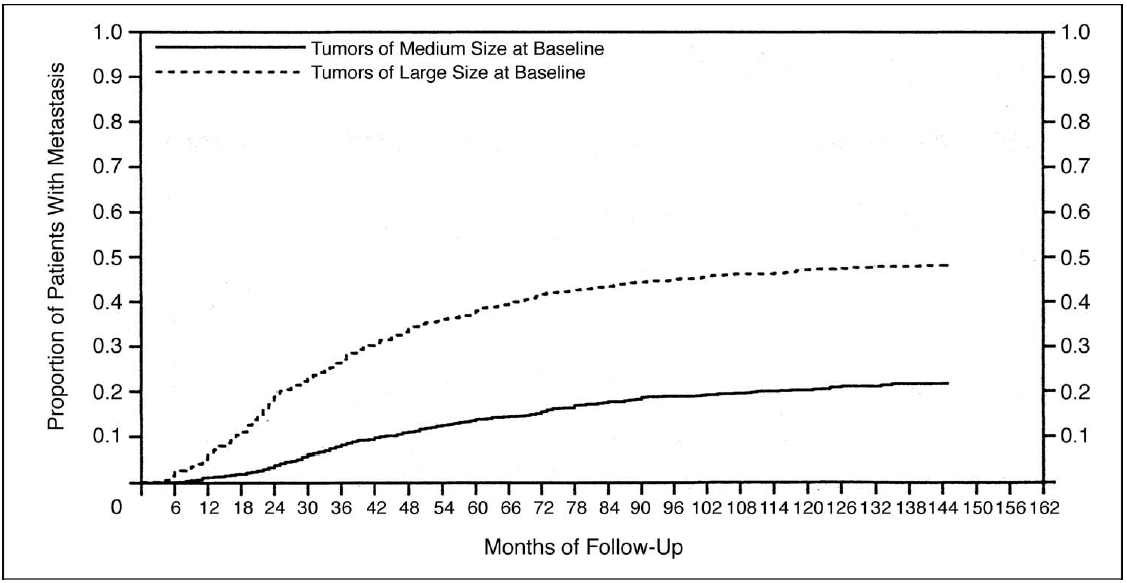
A prelim efficacy signal for uveal melanoma in this trial with a dose (50mcg weekly) that is lower than the 68mcg weekly dose later expanded upon and presented at ASCO last year. Fingers crossed for our patients with this rare disease!
(note: I have fCOI with @Immunocore)
(note: I have fCOI with @Immunocore)

Cytokine Release Syndrome: uncommon but potentially serious side effect. Manageable with everyone's growing experience with adoptive T cell therapy. This trial predated the approval of tocilizumab for severe CRS. Hospitalization mandatory for first 3 doses on study. 

Neat pharmacodynamic markers with this drug...
Spikes of serum markers of Type 1 IFN response like IL-6, IL-10, IFN-gamma, etc are strongest with D1, get more manageable over time.
Some correlation between CXCL-10 spike and CXCR3+CD8+ cells recruited out of plasma. Cool!
Spikes of serum markers of Type 1 IFN response like IL-6, IL-10, IFN-gamma, etc are strongest with D1, get more manageable over time.
Some correlation between CXCL-10 spike and CXCR3+CD8+ cells recruited out of plasma. Cool!

Obligatory 'representative' photomicrographs: 3 patients with subcutaneous mets before and during treatment showing increase in CD3+ infiltration.
(C is uveal...ya love to see it).
I'm only like 183rd author on this so the fact I'm tweeting it tells you how pumped I am!
(C is uveal...ya love to see it).
I'm only like 183rd author on this so the fact I'm tweeting it tells you how pumped I am!

Thanks to lead/senior authors Mark Middleton and Mario Sznol, co-author @OmidHamidMD & Immunocore team. Stay tuned for more with this agent and the entire class of T cell redirectors. Major issue is HLA-A 02:01 restriction: only 40-50% of West Europeans have the allele.
• • •
Missing some Tweet in this thread? You can try to
force a refresh