Should we treat subclinical hypothyroidism during pregnancy?
A tweetorial on physiology, overdiagnosis, risk stratification and treatment harms.
Do you treat subclinical hypothyroidism during pregnancy?❌✅
- Use of the correct reference range is pivotal (grey area of figure).
So, do not use 2.5/3.0 mU/L cut-offs
Note: Any TSH above 10 mU/L = overt hypothyroidism (or lab artefact)
liebertpub.com/doi/full/10.10…

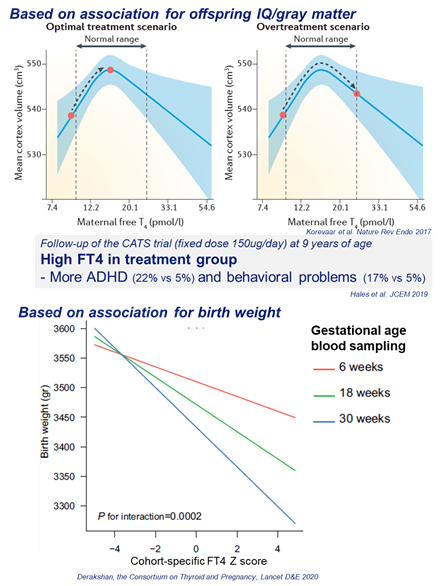
Overdiagnosis ➡️ overtreatment ➡️ increased risk of harm
Note: plenty of data on BMI/ethnicity ref ranges, but no evidence this is clinically meaningful
liebertpub.com/doi/abs/10.108…

Large inter assay differences in FT4 do not allow guidelines to provide any fixed FT4 limits
Best option = adopt a ref range from literature
Why not use the total T4 instead?
- >99% = bound
Thus: biologically unavailable & reflection of TBG/estrogen
- Literature on ref ranges very poor (very poor data for 150% of non-pregnancy ref range)
- Poor reflection of HPT axis (fig)
- No associations with adverse outcomes
pubmed.ncbi.nlm.nih.gov/27187054/

Because it is opposite of normal physiology (fig):
hCG➡️TSH receptor stimulation➡️FT4⬆️& TSH⬇️
Also, hCG➡️pituitary TSH receptor stimulation➡️ultrashort feedback loop➡️TSH suppression
AKA the Brokken-Wiersinga-Prummel Loop pubmed.ncbi.nlm.nih.gov/15588378/

Risk stratification is key!
Below: overview of ATA guidelines (green = no treatment, red = treatment).
We’ll get to gray zone..
liebertpub.com/doi/full/10.10…

1 positive, showing lower risk preterm birth (below)
Note: study started with old ref ranges, LT4 benefit for TSH >4 is another argument for use of current ref ranges
pubmed.ncbi.nlm.nih.gov/27879326/
pubmed.ncbi.nlm.nih.gov/29126290/

- 1 (over)treated (150ug/day), start week 13
- 1 treated with 75ug/day, start week 18
Based on RCTs:
- Still unsure if treatment is beneficial
- If you treat: start early, don’t overtreat
nejm.org/doi/full/10.10…
nejm.org/doi/full/10.10…
Guidelines: consider treatment, individualize
Think about:
- Abnormal physiology: subhypo despite high hCG (twin, 8-11 wks)
- High TSH
- High-normal TPOAb titer (academic.oup.com/jcem/article/1…)
- High pretest probability of subhypo related adverse outcomes

* Reflects an abnormal physiology
* Use correct reference ranges to diagnose
* Risk stratify: TPOAbs, gestational age etc.
* If you treat ➡️ Don’t overtreat
For other very good tweetorials, follow those who inspired me
@tony_breu
@CPSolvers
@ebtapper
@ash_bo21
@AvrahamCooperMD
@MiddeldorpS
@Leo_ReapDO
#thyroidchat
More time to spare?
A hyperthyroidism tweetorial: