1/ 💭 When should I show up? What if I answer a question wrong? Is my presentation too long? Where’s the bathroom? 💭
Sounds like a case of “New Rotation Jitters”
The Cure - Setting Expectations!
Literally, one of my favorite things 🤓
#MedEd #MedTwitter #MedEdTwagTeam
Sounds like a case of “New Rotation Jitters”
The Cure - Setting Expectations!
Literally, one of my favorite things 🤓
#MedEd #MedTwitter #MedEdTwagTeam

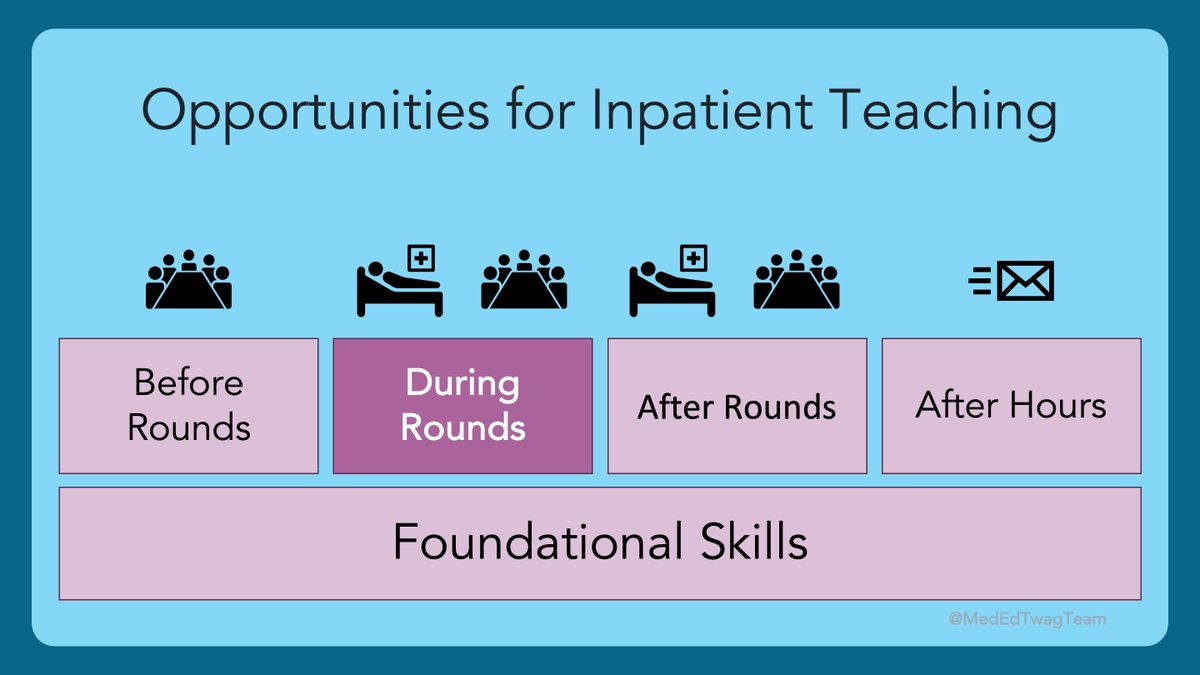
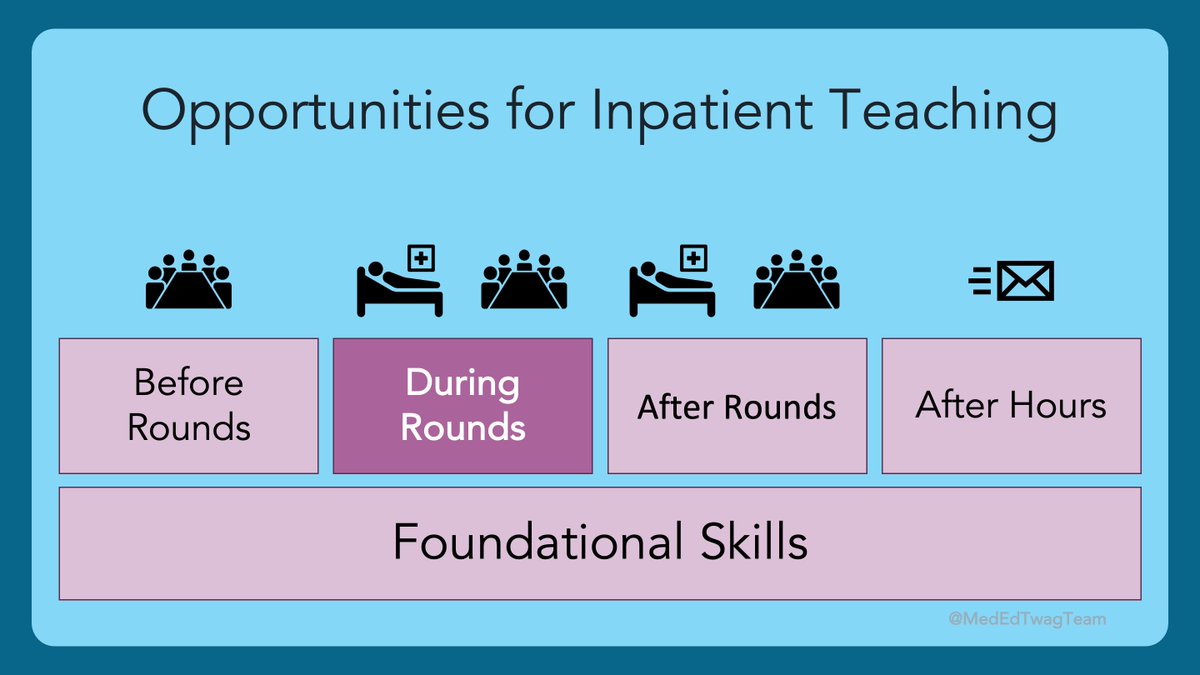
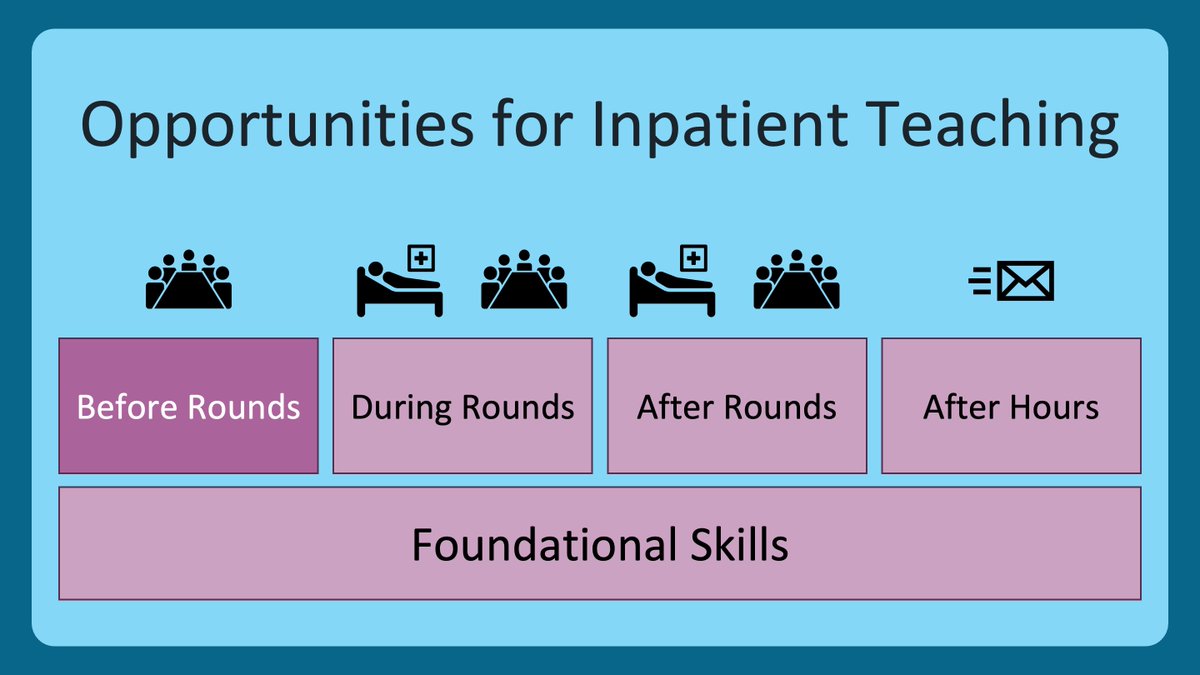
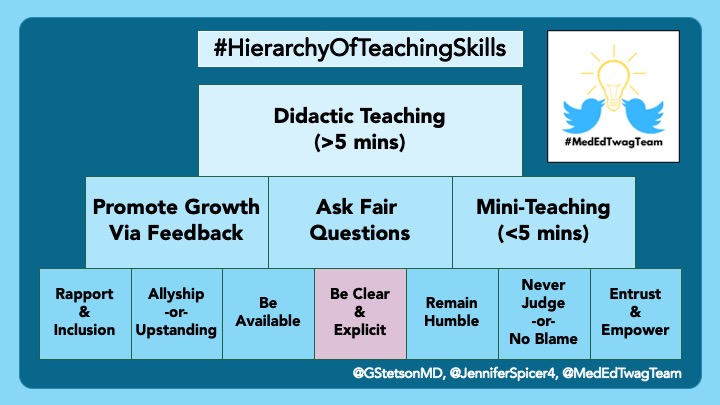
2/ Here is where we are in our journey through the #HierarchyOfTeachingSkills.
Remember that this first level of skills is all about creating #PsychologicalSafety.
If you want to see any of our previous threads, check out the @MedEdTwagTeam account.
Remember that this first level of skills is all about creating #PsychologicalSafety.
If you want to see any of our previous threads, check out the @MedEdTwagTeam account.
3/ Setting clear and explicit expectations is a key teaching skill that will pay numerous dividends.
And like much of teaching, there is an art and a science.
And like much of teaching, there is an art and a science.

4/ First the Science. WHY Expectations?
Anyone out there remember getting first day jitters when starting a new clinical rotation? 🙋
#MedStudentTwitter? You there?
Yeah? Me too!!!
Those jitters and worries are called extraneous load.
Say what?!?
Anyone out there remember getting first day jitters when starting a new clinical rotation? 🙋
#MedStudentTwitter? You there?
Yeah? Me too!!!
Those jitters and worries are called extraneous load.
Say what?!?
5/ Looking at the problem through the lens of cognitive load theory (H/T @MedEdModels & @GIMedEd), clinical learning can involve huge intrinsic and germane loads.
Plain English: learning through patient care is complex and requires a lot of thought.
Plain English: learning through patient care is complex and requires a lot of thought.

6/ Those jitters and worries are distractions and take away processing power from the more pressing tasks of patient care.
In cognitive load theory, those distractions are called extraneous load.
Expectations can reduce this 👆.
In cognitive load theory, those distractions are called extraneous load.
Expectations can reduce this 👆.
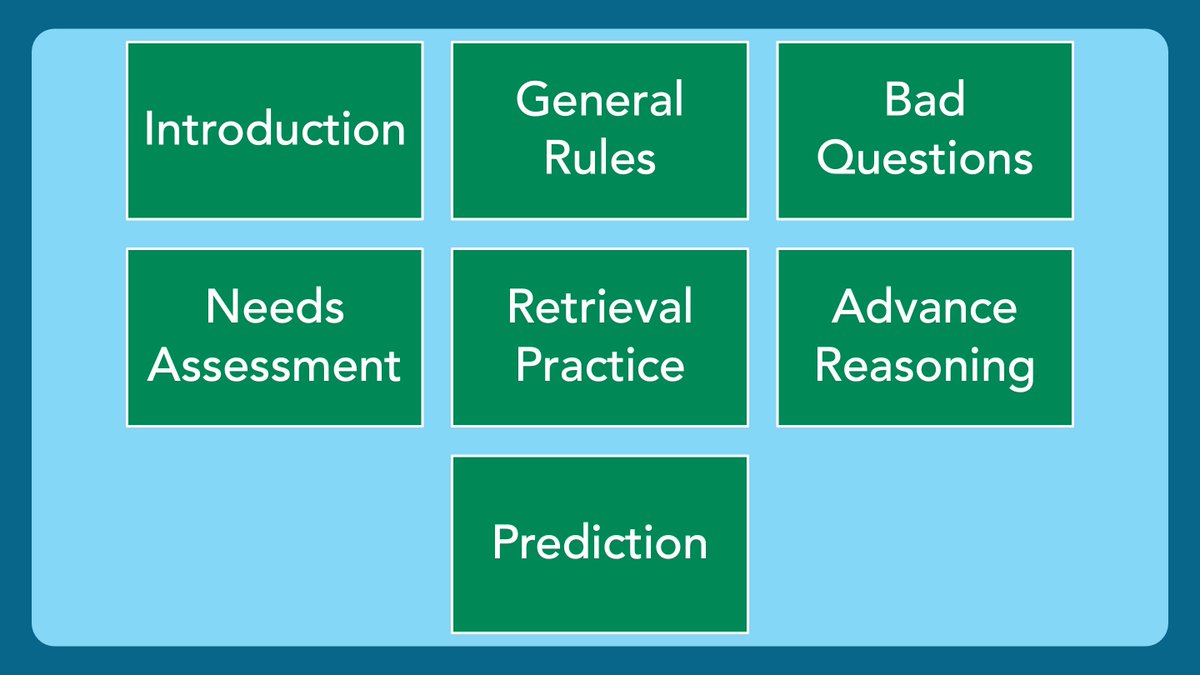
7/ Below is the gist of 'the WHAT' I make clear to my learners every time I am on service.
For context, I am an IM trained hospitalist, working at a VA hospital
*Covered in previous @MedEdTwagTeam threads (check ‘em out)
**Covered in future @MedEdTwagTeam threads (stay tuned)
For context, I am an IM trained hospitalist, working at a VA hospital
*Covered in previous @MedEdTwagTeam threads (check ‘em out)
**Covered in future @MedEdTwagTeam threads (stay tuned)

8/ My approach reflects what I value.
@JenniferSpicer4 & @gradydoctor use the #ACGME competencies as a loose framework.
A senior resident I worked with sent a beautiful e-mail to the team before we started. See what he covered 👇.
What do y'all think is important to cover?
@JenniferSpicer4 & @gradydoctor use the #ACGME competencies as a loose framework.
A senior resident I worked with sent a beautiful e-mail to the team before we started. See what he covered 👇.
What do y'all think is important to cover?

9/ Now for the Art of Expectations. The HOW.
There is a balance to be struck between the importance of set-up, and information overload. (H/T @DrCalvinChou & @Gurpreet2015)
Too MANY expectations can become extraneous load!
There is a balance to be struck between the importance of set-up, and information overload. (H/T @DrCalvinChou & @Gurpreet2015)
Too MANY expectations can become extraneous load!
10/ 🚨 Best Practice Alert 🚨
✅ Document your expectations clearly, and concisely
✅ Set a reasonable limit (1 page? 500 words?)
✅ This is a “living document” - Your expectations will change as you grow as a clinician, supervisor, and educator. So should this document.
✅ Document your expectations clearly, and concisely
✅ Set a reasonable limit (1 page? 500 words?)
✅ This is a “living document” - Your expectations will change as you grow as a clinician, supervisor, and educator. So should this document.
11/ Revisit this document before joining a clinical team.
Does everything still resonate? Have my values or expectations changed?
Mine did.
2-3 years ago I added an expectation about Allyship and Upstanding.
I deleted something else. I have no clue what it was.
Does everything still resonate? Have my values or expectations changed?
Mine did.
2-3 years ago I added an expectation about Allyship and Upstanding.
I deleted something else. I have no clue what it was.

12/ Once you feel good with your document, e-mail it out to the team…or don’t.
🔑 This is another artistic opportunity.
Conveying tone over email is hard. If you send out an email beforehand, this is their first impression of you.
It could work great...or backfire.
🔑 This is another artistic opportunity.
Conveying tone over email is hard. If you send out an email beforehand, this is their first impression of you.
It could work great...or backfire.
13/ Personally, I like to meet the team on Day 1, and lay out 3 key expectations (with a sprinkle of humor & pizzaz):
1⃣ Rounds + Teaching
2⃣ Feedback
3⃣ Allyship & Upstanding
For everything else, see document for details.
1⃣ Rounds + Teaching
2⃣ Feedback
3⃣ Allyship & Upstanding
For everything else, see document for details.
14/ This way, I get to make the first impression, rather than an e-mail.
Also, by sending out the e-mail afterwards, they get all the details, in a form they can later reference.
AND! You’ve saved your team a long-winded spiel. Bonus points!
Also, by sending out the e-mail afterwards, they get all the details, in a form they can later reference.
AND! You’ve saved your team a long-winded spiel. Bonus points!
15/ Lastly, make sure to find time to set expectations with each individual.
Here you can discuss:
1⃣ Role specific expectations
2⃣ Their expectations for themselves
3⃣ Their expectations for YOU – “what can I do to provide you with the best possible learning experience?”
Here you can discuss:
1⃣ Role specific expectations
2⃣ Their expectations for themselves
3⃣ Their expectations for YOU – “what can I do to provide you with the best possible learning experience?”
16/ My #WorkBFF, @JenniferSpicer4, also uses this 1:1 meeting time to suss out if there may be any personal logistics that the team should work around, such as childcare pickup/drop off.
This has not been part of my routine approach…but it is now!!!
#GetYourselfAWorkBFF
This has not been part of my routine approach…but it is now!!!
#GetYourselfAWorkBFF

17/ Last LAST thing…Don’t skip expectations.
Do it on Day 1! ASAP!
It is tempting to dive straight into the clinical work, and sometimes it is necessary.
But, don’t leave on your first day without having set expectations.
Do it on Day 1! ASAP!
It is tempting to dive straight into the clinical work, and sometimes it is necessary.
But, don’t leave on your first day without having set expectations.
18/ Take Aways
⭐️ Expectations reduce extraneous load
⭐️ Your expectations should reflect your values
⭐️ Document your expectations in a concise manner
⭐️ Deliver them in a combo of in-person & e-mail formats
⭐️ Meet 1:1 with each team member on Day 1
⭐️ Expectations reduce extraneous load
⭐️ Your expectations should reflect your values
⭐️ Document your expectations in a concise manner
⭐️ Deliver them in a combo of in-person & e-mail formats
⭐️ Meet 1:1 with each team member on Day 1

19/ Next week, the “better half” of the #MedEdTwagTeam is back to drop some knowledge about the power of humility on the learning climate.
And, as always, you can find all our previous threads @MedEdTwagTeam.
✌️🖖
And, as always, you can find all our previous threads @MedEdTwagTeam.
✌️🖖

• • •
Missing some Tweet in this thread? You can try to
force a refresh