1/
Ever wonder why eosinophils vanish from the blood after exposure to steroids?
I assumed that steroids somehow destroy them and that is why they disappear.
But there's a lot more going on.
#tweetorial #medtwitter
Ever wonder why eosinophils vanish from the blood after exposure to steroids?
I assumed that steroids somehow destroy them and that is why they disappear.
But there's a lot more going on.
#tweetorial #medtwitter
2/
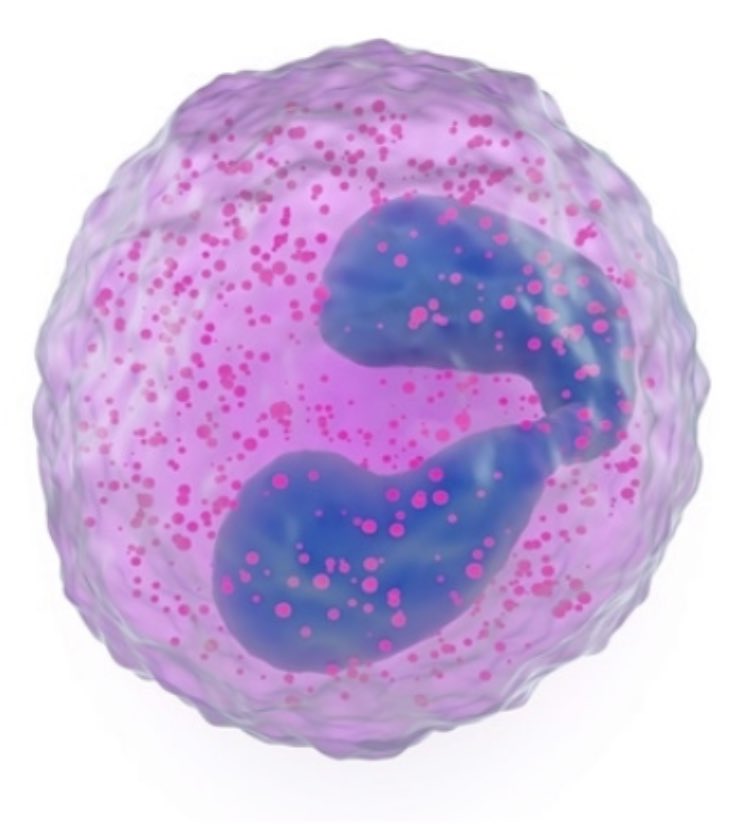
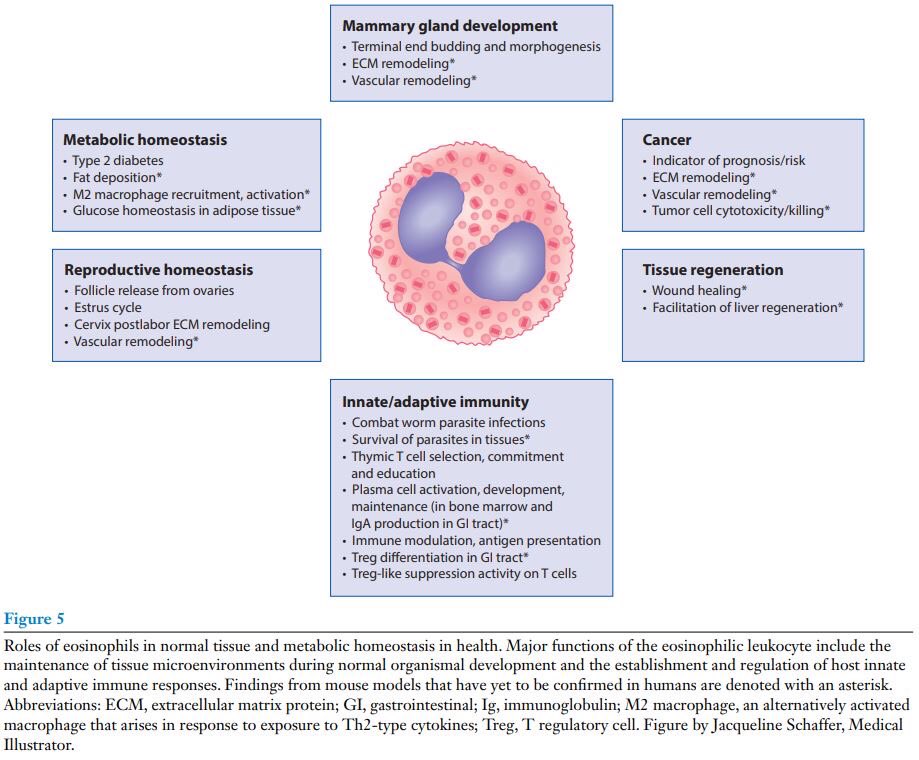
First let's review eosinophil biology.
Eosinophils are granulocytic white blood cells that develop in the bone marrow and reside primarily in tissues.
They have a multitude of physiologic functions, from parasite defense to immuno-regulation.
pubmed.ncbi.nlm.nih.gov/31977298/
First let's review eosinophil biology.
Eosinophils are granulocytic white blood cells that develop in the bone marrow and reside primarily in tissues.
They have a multitude of physiologic functions, from parasite defense to immuno-regulation.
pubmed.ncbi.nlm.nih.gov/31977298/
3/
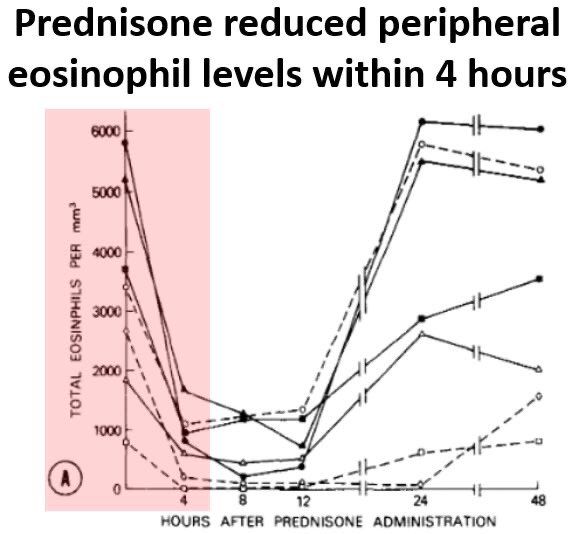
In the 1970s the effects of steroids on blood eosinophil levels were first studied.
🔑 Prednisone led to marked declines in peripheral eosinophil counts within 4 hours.
(bonus: the senior author on this paper was Dr. Anthony Fauci!)
pubmed.ncbi.nlm.nih.gov/313411/
In the 1970s the effects of steroids on blood eosinophil levels were first studied.
🔑 Prednisone led to marked declines in peripheral eosinophil counts within 4 hours.
(bonus: the senior author on this paper was Dr. Anthony Fauci!)
pubmed.ncbi.nlm.nih.gov/313411/
4/
Why do steroids have this effect on eosinophils?
We will focus on 3 potential mechanisms:
🔺Decreased production
🔺Redistribution to other tissue compartments
🔺Cell death
Why do steroids have this effect on eosinophils?
We will focus on 3 potential mechanisms:
🔺Decreased production
🔺Redistribution to other tissue compartments
🔺Cell death
5/
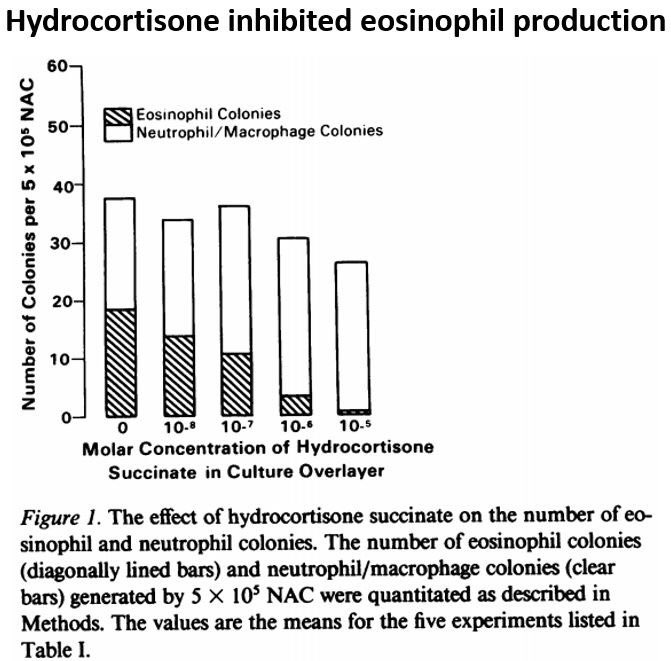
The first possibility is reduced bone marrow production.
This was noted in a 1985 study, where hydrocortisone reduced new eosinophil development, without affecting neutrophils or macrophages.
ncbi.nlm.nih.gov/pmc/articles/P…
The first possibility is reduced bone marrow production.
This was noted in a 1985 study, where hydrocortisone reduced new eosinophil development, without affecting neutrophils or macrophages.
ncbi.nlm.nih.gov/pmc/articles/P…
6/
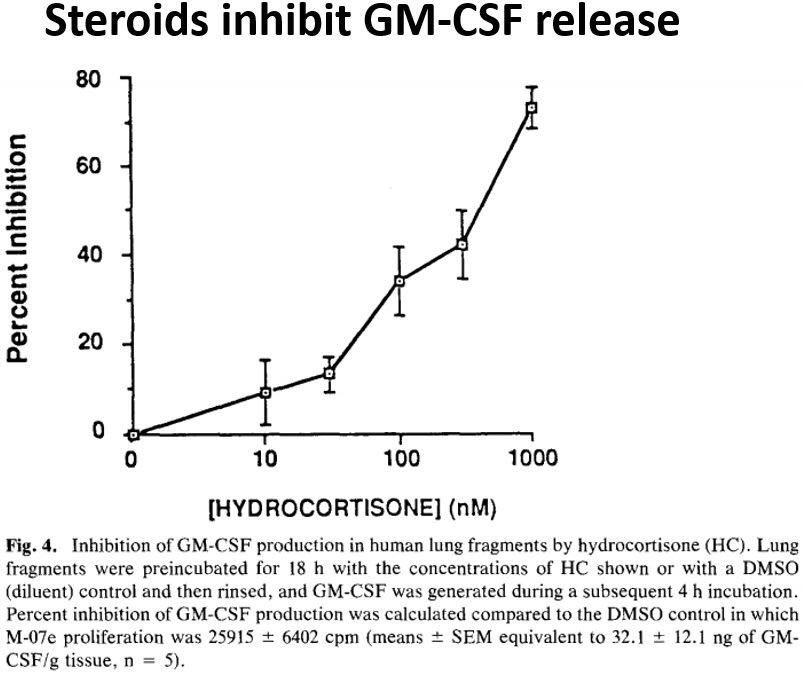
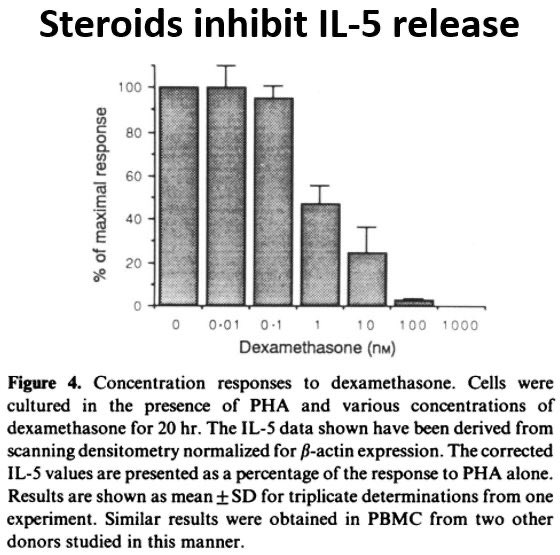
Steroids do ⬇️ production of cytokines that stimulate eosinophil growth in the bone marrow (eg IL-5 and GM-CSF) and also block their cellular effects.
This may explain inhibition of eosinophil production.
pubmed.ncbi.nlm.nih.gov/1493921/ (IL-5)
pubmed.ncbi.nlm.nih.gov/8114512/ (GM-CSF)

Steroids do ⬇️ production of cytokines that stimulate eosinophil growth in the bone marrow (eg IL-5 and GM-CSF) and also block their cellular effects.
This may explain inhibition of eosinophil production.
pubmed.ncbi.nlm.nih.gov/1493921/ (IL-5)
pubmed.ncbi.nlm.nih.gov/8114512/ (GM-CSF)
7/
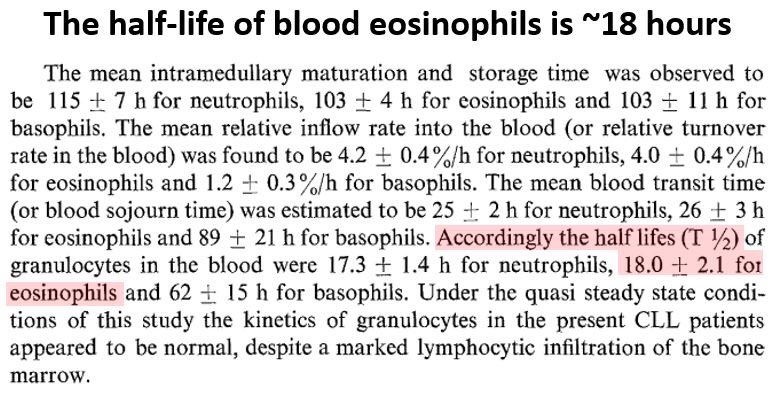
At the same time, eosinophils have a half-life in the blood stream (18 hours) that‘s far longer than the time it takes for counts to drop (as early as 4 hours).
💡 Something else besides decreased production must be going on.
pubmed.ncbi.nlm.nih.gov/223692/
At the same time, eosinophils have a half-life in the blood stream (18 hours) that‘s far longer than the time it takes for counts to drop (as early as 4 hours).
💡 Something else besides decreased production must be going on.
pubmed.ncbi.nlm.nih.gov/223692/
8/
Another possibility is redistribution.
Recall from tweet #2 that most eosinophils reside in tissues, not blood.
Might steroids cause eosinophils to migrate out of the bloodstream?
Another possibility is redistribution.
Recall from tweet #2 that most eosinophils reside in tissues, not blood.
Might steroids cause eosinophils to migrate out of the bloodstream?
9/
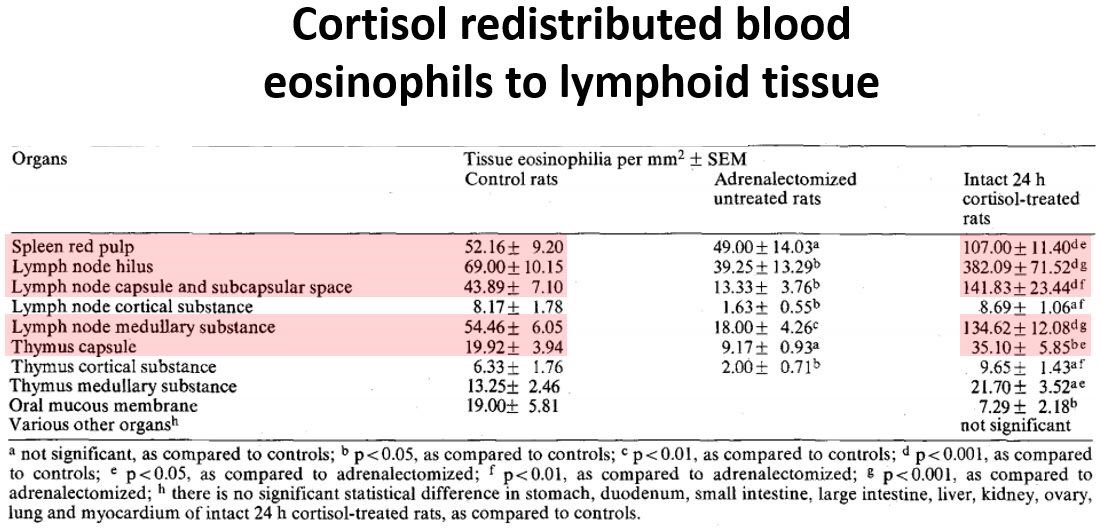
While human data is lacking, experiments in animals suggest steroids do cause eosinophil redistribution.
Giving cortisol to rats caused eosinophils to migrate out of the blood and into lymphoid tissues, such as the spleen and lymph nodes.
pubmed.ncbi.nlm.nih.gov/658264/
While human data is lacking, experiments in animals suggest steroids do cause eosinophil redistribution.
Giving cortisol to rats caused eosinophils to migrate out of the blood and into lymphoid tissues, such as the spleen and lymph nodes.
pubmed.ncbi.nlm.nih.gov/658264/
10/
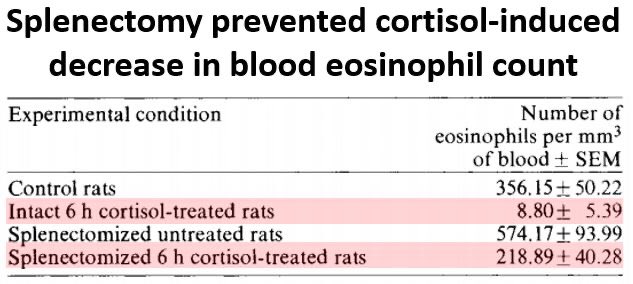
In the same experiment, splenectomy prior to cortisol preserved blood eosinophil counts, compared to rats w/ intact spleens.
🔑 This strongly suggested that steroids redistribute eosinophils to lymphoid organs, though exactly how isn't known.
pubmed.ncbi.nlm.nih.gov/658264/
In the same experiment, splenectomy prior to cortisol preserved blood eosinophil counts, compared to rats w/ intact spleens.
🔑 This strongly suggested that steroids redistribute eosinophils to lymphoid organs, though exactly how isn't known.
pubmed.ncbi.nlm.nih.gov/658264/
11/
We have seen that steroids (1) block new eosinophil development and (2) seem to induce migration out of the blood and into lymphoid tissues.
Before I began preparing this tweetorial, I assumed that steroids destroy eosinophils.
Is that also the case?
We have seen that steroids (1) block new eosinophil development and (2) seem to induce migration out of the blood and into lymphoid tissues.
Before I began preparing this tweetorial, I assumed that steroids destroy eosinophils.
Is that also the case?
12/
Recall from tweet #6 that steroids block the release and cellular effects of cytokines that support eosinophil development in the bone marrow (IL-5 and GM-CSF).
These cytokines also promote eosinophil survival, potentially by inhibiting apoptosis.
pubmed.ncbi.nlm.nih.gov/1864012/
Recall from tweet #6 that steroids block the release and cellular effects of cytokines that support eosinophil development in the bone marrow (IL-5 and GM-CSF).
These cytokines also promote eosinophil survival, potentially by inhibiting apoptosis.
pubmed.ncbi.nlm.nih.gov/1864012/
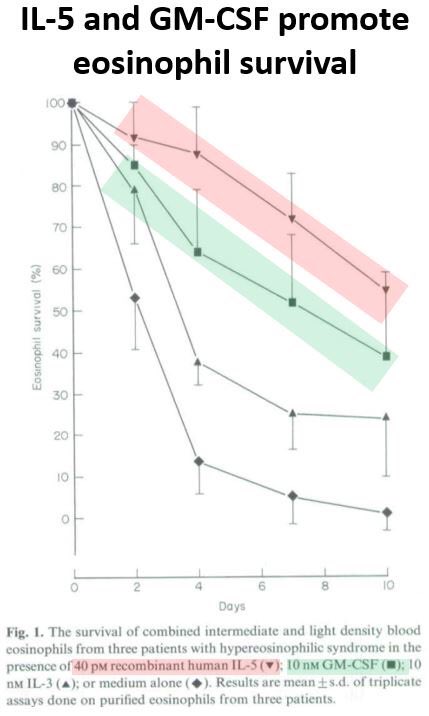
13/
You would expect that since steroids inhibit IL-5 and GM-CSF, they should shorten eosinophil lifespan.
🔑 And accelerated cell death is exactly what happens when eosinophils are exposed to steroids.
pubmed.ncbi.nlm.nih.gov/1551701/
You would expect that since steroids inhibit IL-5 and GM-CSF, they should shorten eosinophil lifespan.
🔑 And accelerated cell death is exactly what happens when eosinophils are exposed to steroids.
pubmed.ncbi.nlm.nih.gov/1551701/

14/
🔑 Blood eosinophil counts drop within hours of exposure to steroids
🔑Steroids inhibit GM-CSF and IL-5 release and cellular effects
🔑This ⬇️ eosinophil production in the bone marrow and ⬆️ cell death
🔑Redistribution to lymphoid organs like the spleen also plays a role
🔑 Blood eosinophil counts drop within hours of exposure to steroids
🔑Steroids inhibit GM-CSF and IL-5 release and cellular effects
🔑This ⬇️ eosinophil production in the bone marrow and ⬆️ cell death
🔑Redistribution to lymphoid organs like the spleen also plays a role
• • •
Missing some Tweet in this thread? You can try to
force a refresh