Meniscus injury: a complete review.
1/15
@MedTweetorials @RosenelliEM
#MedEd #OrthoTwitter #Tweetorials
1/15
@MedTweetorials @RosenelliEM
#MedEd #OrthoTwitter #Tweetorials

The meniscus function is two-fold. It increases stability by deepening the tibial surface and it aids in force transmission by increasing the contact area to spread force over a larger surface area. The meniscus is responsible for 50% of load transmission across the knee. (1)
2/
2/
The lateral meniscus has a more circular shape than the C-shaped medial meniscus. The lateral meniscus covers a larger portion of the articular surface and is also more mobile than the medial meniscus. The medial meniscus is relatively immobile and is attached to the MCL.
3/15
3/15

Three ligamentous attachments for the meniscus are the intermeniscal ligament (attaching the menisci anteriorly), coronary ligaments (securing the meniscus to the peripheral tibia), and the meniscofemoral ligament (securing the menisci to the PCL).
4/15
4/15

Vascular supply to the menisci originates from the medial and lateral geniculate arteries via the peri-meniscal capillary plexus. Following birth, the menisci become increasing avascular, so by maturity only the peripheral 10% to 25% of the tissue is perfused (1).
5/15
5/15
The peripheral vascularization of the meniscus creates three zones. The peripheral 1/3 is the red zone which is perfused by the geniculate arteries. The inner 2/3 is the white zone which is perfused by the synovial fluid. Between these zones is an intermediate red-white zone.
6/
6/
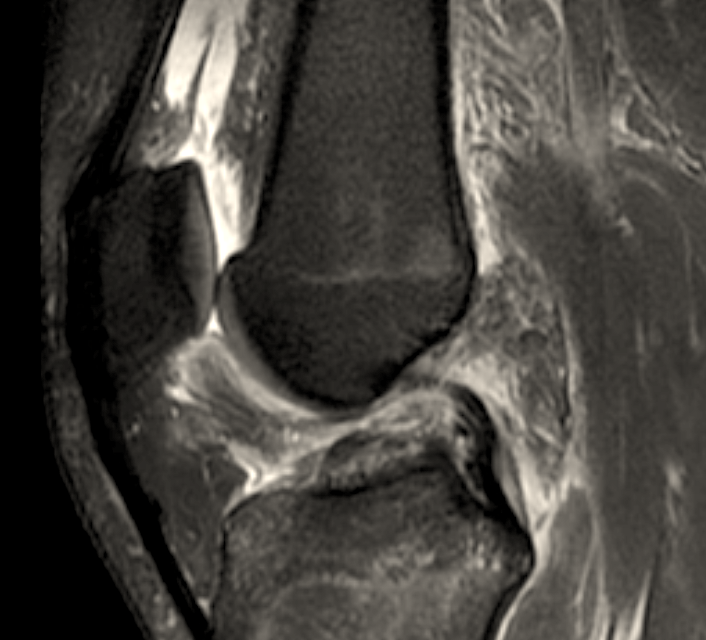
Patients may describe hearing a pop in the knee, swelling, or pain in the knee. Although special provocative signs for meniscal tears (e.g. McMurray) are present, their accuracy, specificity/sensitivity are highly variable and questionable. (2) MRI is the most sensitive test.
7/
7/
The most common meniscal tears in young active patients are longitudinal-vertical, and degenerative tears in the elderly population. The most common locations for tears are the medial menisci and posterior horn. (2)
8/15
8/15

Due to the risk of OA after meniscal resection, it is important to salvage as much menisci as possible. Non-operative treatment (RICE and anti-inflammatories) are the first line of treatment in degenerative tears. If symptoms persist for > 3-6 mo. surgery may be indicated.
9/15
9/15
For simple tears confined to the red zone, pts may undergo 4-6 weeks of conservative treatment and PT to determine if spontaneous healing may occur. If required there are three surgical treatments: partial meniscectomy, meniscal repair, and meniscal reconstruction/transplant
10/
10/
Arthroscopic partial meniscectomy may be utilized in patients with radial tears in the white zone and degenerative tears unresponsive to non-operative therapy. Meniscal repair may be utilized in tears in the red zone or horizontal-vertical tears (extended indications exist)
11/
11/
The gold standard for repair is the inside-out technique, in which the tear is fixed by placement and fixation of a suture from the intra-articular region to an extracapsular area with a posterolateral or posteromedial incision.
12/15
12/15
In a meta-analysis, it was concluded that although meniscal repairs had a higher re-operation rate than meniscectomy, they result in a better long-term functional outcome, better activity level and lower failure rate. (2)
13/15
13/15
Two methods are utilized for reconstruction: meniscal scaffolds and meniscal allograft transplantation. These techniques may be utilized in younger patients. Correct sizing is critical for transplant. Under sizing creates poor congruity and increased loading.
14/15
14/15
Conclusion: Evidence has reliably demonstrated that meniscectomy leads to a significantly increased risk of developing OA in the knee and that the minimum amount of meniscus possible should be removed only. (3)
15/15
15/15
If you enjoyed this review, please RT and follow to help the page grow.
References:
1: ncbi.nlm.nih.gov/pmc/articles/P…
2: ncbi.nlm.nih.gov/pmc/articles/P…
3: ncbi.nlm.nih.gov/pmc/articles/P…
#MedEd #MedTwitter #OrthoTwitter #Ortho #tweetorial
References:
1: ncbi.nlm.nih.gov/pmc/articles/P…
2: ncbi.nlm.nih.gov/pmc/articles/P…
3: ncbi.nlm.nih.gov/pmc/articles/P…
#MedEd #MedTwitter #OrthoTwitter #Ortho #tweetorial
• • •
Missing some Tweet in this thread? You can try to
force a refresh