1/ 💭 Did I check the labs? I know they were fine yesterday. What should I say? 💭
As a supervisor, you need to make clear to your learners (1) the right answer is: “I forgot to check them”
And (2) your reaction will be: “No problem. Let’s check them now.”
#MedEd #MedTwitter
As a supervisor, you need to make clear to your learners (1) the right answer is: “I forgot to check them”
And (2) your reaction will be: “No problem. Let’s check them now.”
#MedEd #MedTwitter

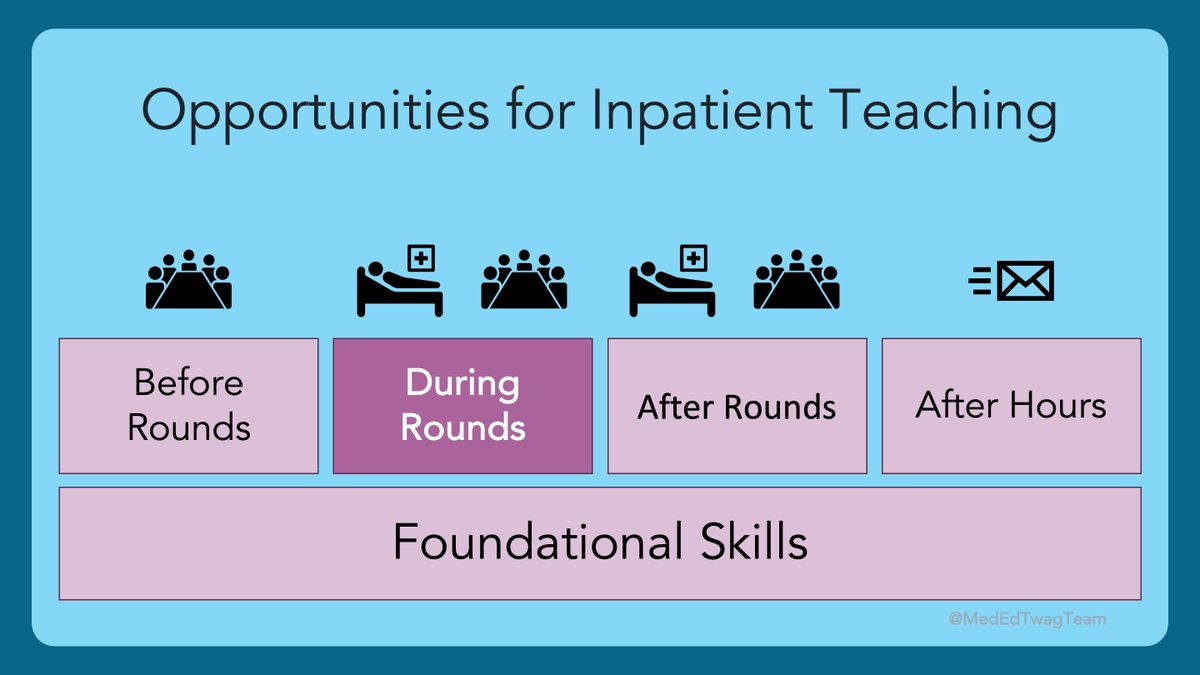
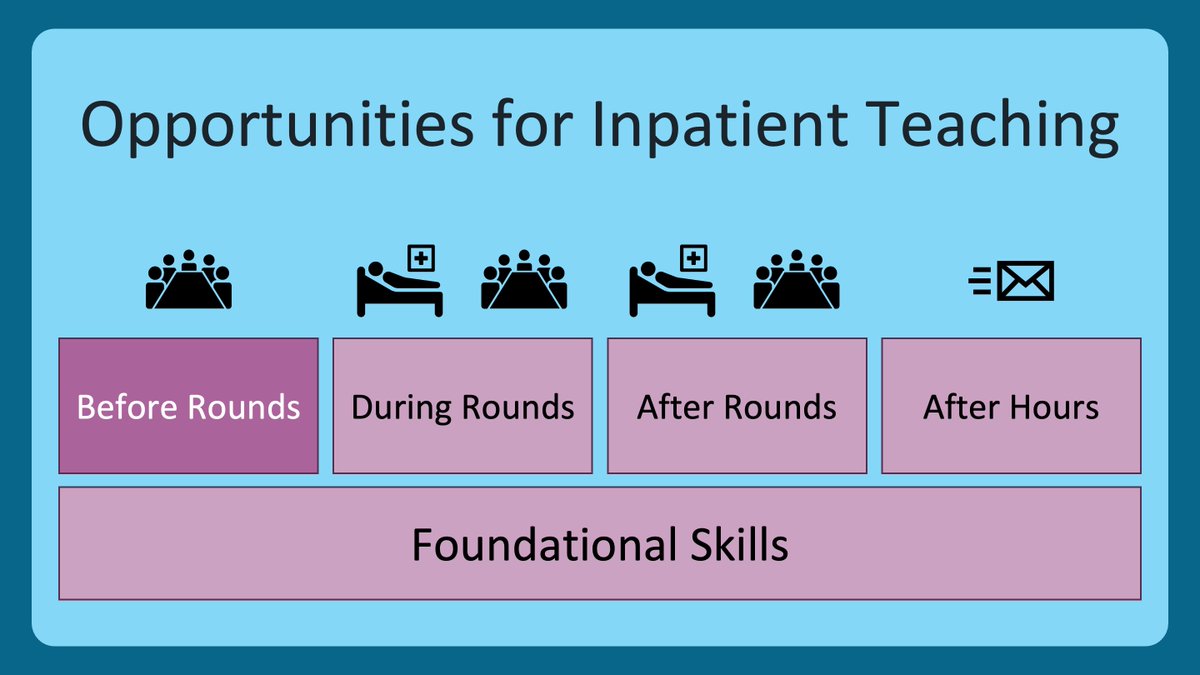
2/ Here is where we are in our journey through the #HierarchyOfTeachingSkills.
Remember that this first level of skills is all about #PsychologicalSafety.
Not judging your learners is key to this.
Find our previous threads @MedEdTwagTeam.
Remember that this first level of skills is all about #PsychologicalSafety.
Not judging your learners is key to this.
Find our previous threads @MedEdTwagTeam.

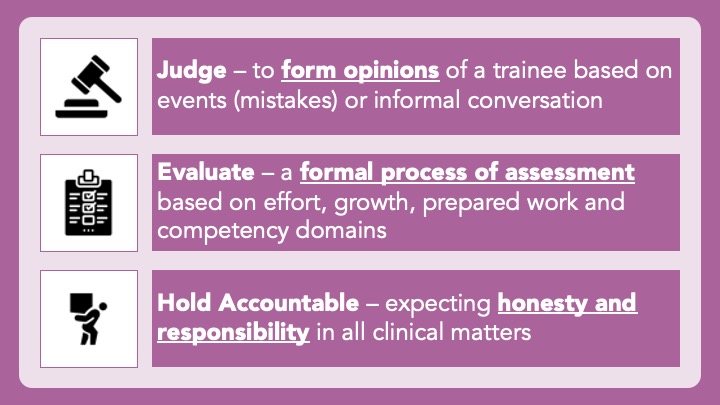
3/ I make sure I never judge my learners. But I DO evaluate them and hold them accountable.
To me, these are three different things.
Here is how I define these concepts 👇
To me, these are three different things.
Here is how I define these concepts 👇
4/ Let’s dive a little deeper.
In the book, Teaching in the Hospital, @kevinjolearymd, @MarianneTschoe & Jeff Wiese describe establishing a “no blame” culture.
They explain this 👇
In the book, Teaching in the Hospital, @kevinjolearymd, @MarianneTschoe & Jeff Wiese describe establishing a “no blame” culture.
They explain this 👇

5/ You can see that a “no-blame culture” should be established for #PatientSafety.
But it also creates #PsychologicalSafety!
When learners make mistakes, if they know that you acknowledge this is a normal part of the learning process, they will disclose & ask for help sooner.
But it also creates #PsychologicalSafety!
When learners make mistakes, if they know that you acknowledge this is a normal part of the learning process, they will disclose & ask for help sooner.
6/ A great way to set this up is to tell them about a time when you made a mistake. We all have our fair share.
Did you fess up right away? Did you conceal it and wish you had done it differently?
Model humility and how to set ego aside for the sake of patients and learning.
Did you fess up right away? Did you conceal it and wish you had done it differently?
Model humility and how to set ego aside for the sake of patients and learning.
7/ When a mistake is revealed, there is work to be done.
This is a golden teaching/learning opportunity!
You need to facilitate a few things:
Diffuse – Don’t judge
Normalize – Alleviate guilt or shame
Explore – Discuss details and root causes
Teach – Distill learning points
This is a golden teaching/learning opportunity!
You need to facilitate a few things:
Diffuse – Don’t judge
Normalize – Alleviate guilt or shame
Explore – Discuss details and root causes
Teach – Distill learning points

9/ This is relatively benign example. Debriefing mistakes or near misses is its own whole skill set.
I know my #WorkBFF has some thoughts on this. Let me just #Twag her in here…#YouAreIt @JenniferSpicer4
Pssst…@gradydoctor…like what I did there? 👆
I know my #WorkBFF has some thoughts on this. Let me just #Twag her in here…#YouAreIt @JenniferSpicer4
Pssst…@gradydoctor…like what I did there? 👆
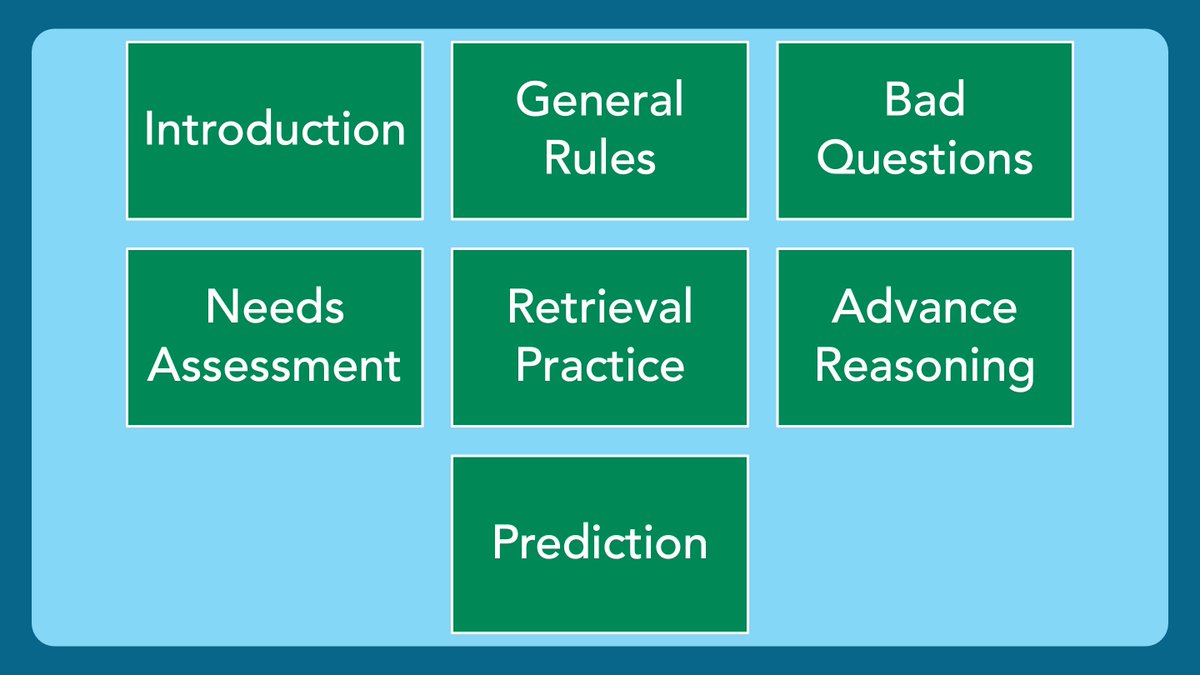
10/ Another form of judgement that can occur is through casual conversation or questions, as explained by @DxRxEdu & @Gurpreet2015 in their @JHospMedicine article: pubmed.ncbi.nlm.nih.gov/32039750/ 

11/ The clinical learning environment needs to be a place where your learners can stretch, i.e.:
-Ask questions when they are curious
-Answer questions even when they are unsure
-Reason through problems on-the-fly
No one ever learned from getting everything right!
-Ask questions when they are curious
-Answer questions even when they are unsure
-Reason through problems on-the-fly
No one ever learned from getting everything right!

12/ Make it clear that:
✅ Casual learning conversations are safe.
✅ Stretching and failing is encouraged.
✅ You will use questions as a teaching tool, but you will not evaluate the answers.
✅ Evaluation WILL take place based on the core competencies and formal patient care.
✅ Casual learning conversations are safe.
✅ Stretching and failing is encouraged.
✅ You will use questions as a teaching tool, but you will not evaluate the answers.
✅ Evaluation WILL take place based on the core competencies and formal patient care.
13/ 🔑 Takeaways:
⭐️ Never judge, but do evaluate and hold accountable
⭐️ When mistakes happen ➡️ diffuse, normalize, explore, teach
⭐️ Ensure learners feel safe in the Stretch Zone
⭐️ Never judge, but do evaluate and hold accountable
⭐️ When mistakes happen ➡️ diffuse, normalize, explore, teach
⭐️ Ensure learners feel safe in the Stretch Zone

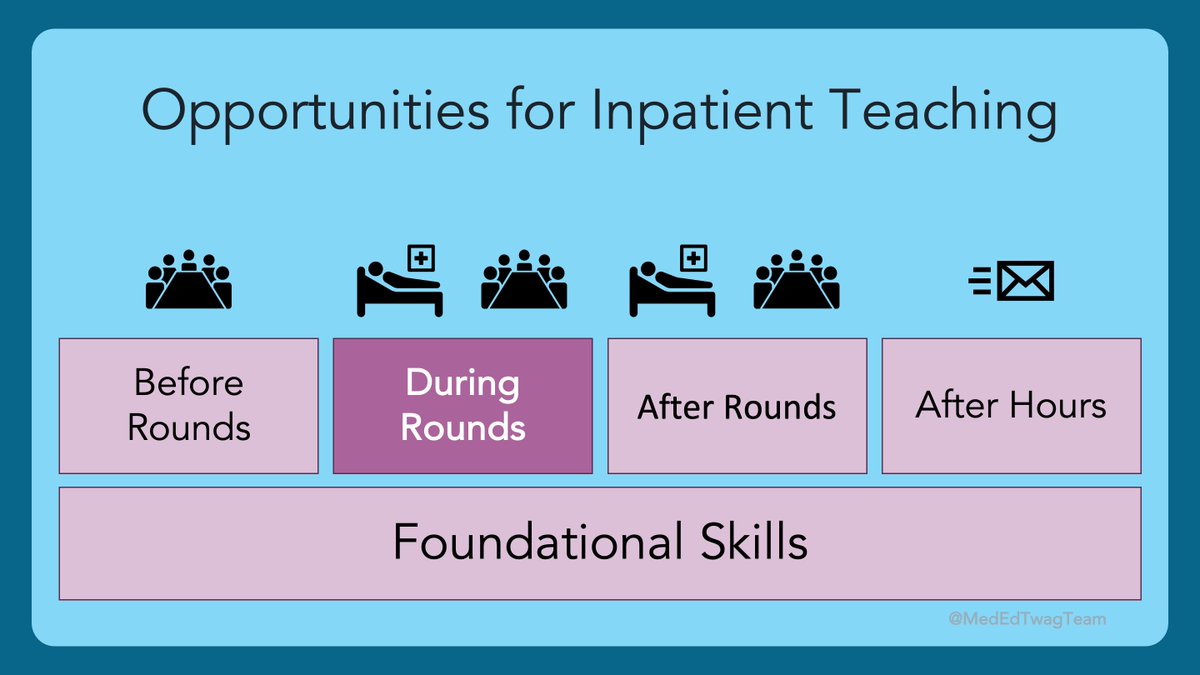
14/ Next week on our journey through the #HierarchyOfTeachingSkills, my #WorkBFF @JenniferSpicer4 will be talking about how to build trust on your clinical teams.
Happy #TweetorialTuesday, Y’all!
Happy #TweetorialTuesday, Y’all!

• • •
Missing some Tweet in this thread? You can try to
force a refresh