#medtwitter 1/What are the top three diagnoses of which you automatically skeptical? My top 3 are UTI, cellulitis, and CAP. Before talking more about "UTIs:, I must repeat the mantra:
PYURIA DOES NOT = UTI.
I will focus mostly on pyuria
PYURIA DOES NOT = UTI.
I will focus mostly on pyuria
2/ Let's consider the following scenario: A young female comes in fever. Urinalysis is obtained that shows 10WBC, - nitrite negative. Boom! You have diagnosed UTI, done. Just kidding, if only it was that easy.
3/I highly suggest listening to the @thecurbsiders episode on UTI (thecurbsiders.com/podcast/231). An important point they make is that UTI is bacteruria + signs and symptoms that localize to the urinary tract. Bacteruria alone is not enough for treatment.
4/You are admitting an elderly female with mild dementia brought in by her family who increased confusion. Urinalysis with +LE and pyuria. No signs of systemic infection or UTI on questioning or exam. Urine culture grows >100,000 E. coli Eh, just treat for a UTI, right?
5/The connection between UTI and delirium has recently been called into question. The Choosing Wisely campaign suggests against antibiotics for bacteriuria in elderly adults without urinary symptoms.
pubmed.ncbi.nlm.nih.gov/24596591/
choosingwisely.org/clinician-list….
pubmed.ncbi.nlm.nih.gov/24596591/
choosingwisely.org/clinician-list….
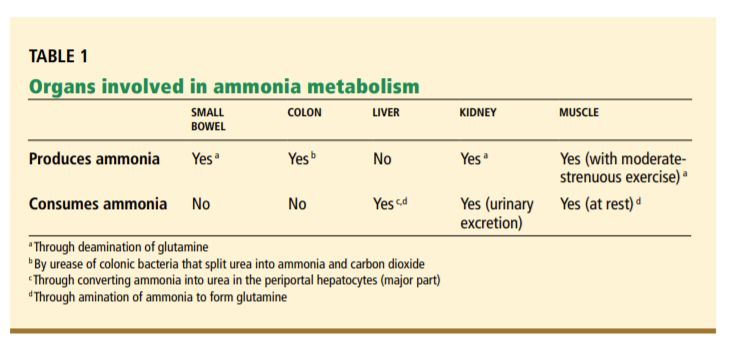
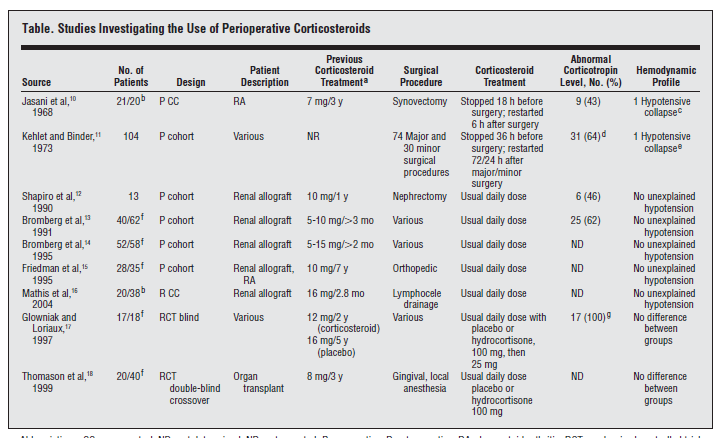
6/ An important thing to remember is that pyuria may be a sign of surrounding abdominal/pelvic inflammation rather than a UTI. In one study of patients hospitalized for non-urinary infections, 30% of adults had pyuria, only 1/3 had a positive culture. (pubmed.ncbi.nlm.nih.gov/24390891/)
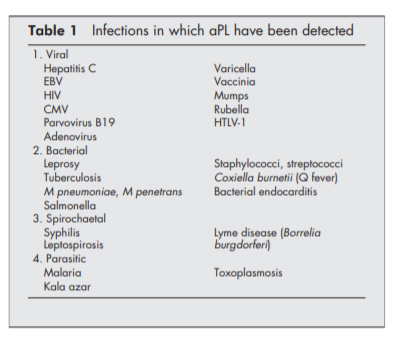
7/ Don't miss another diagnosis d/t early closure. It is always important to remember PUD and other infections including urethritis, prostatitis, viral infections, fungal infections, parasitic infections, TB.
(table source nejm.org/doi/full/10.10…)
(table source nejm.org/doi/full/10.10…)
8/ Up to 13% of F & 2% of M have sterile pyuria. Some elderly females have chronic pyuria/bacteriuria that sis asymptomatic. There are also non-infectious causes of pyuria such as acute interstitual nephritis, GN, SLE, kidney stones/urinary tract abnormalities.
9/ 1 caveat is that you can have sepsis due to a urinary source in absence of urinary symptoms. If no other source is found is a septic patient w/ pyuria >positive culture, treat the urine! Don't see pyuria and stop looking for other sources though.
10/ It is very unlikely (in non-neutropenic pts), to have a urinary source of sepsis without pyuria. Simple cystitis should not cause fevers.
11/I highly suggest reading this NEJM review on pyuria (nejm.org/doi/full/10.10…).
Conclusions:
1. Pyuria without urinary symptoms is likely not a bacterial UTI. Look for other abdominal inflammation, urethritis, other organisms, and non-infectious causes.
Conclusions:
1. Pyuria without urinary symptoms is likely not a bacterial UTI. Look for other abdominal inflammation, urethritis, other organisms, and non-infectious causes.
12/ 2. About 14% of females have sterile pyuria
3. Don't treat asymptomatic pyuria/bacteriuria in elderly patients with delirium
And one more time, PYURIA DOES NOT = UTI.
Other thoughts?
3. Don't treat asymptomatic pyuria/bacteriuria in elderly patients with delirium
And one more time, PYURIA DOES NOT = UTI.
Other thoughts?
13/ Also, I wanted to clarify based on great comments of @PrathitKulkarni about delirium and UTI/bacteruria. Data between "UTI" and delirium is weak. Also, there is not conclusive data that shows treatment leads to improvement of delirium. C. diff %⬆️
pubmed.ncbi.nlm.nih.gov/28624753/
pubmed.ncbi.nlm.nih.gov/28624753/
14/ In a patient w/ encephalopathy who cannot answer ? about symptoms, treatment can be considered if other causes of delirium not identified. Evaluation should not be stopped b/c a lil pyuria on UA. Article also advocates considering "watchful waiting".
amjmed.com/article/S0002-…
amjmed.com/article/S0002-…
15/ Also, found a great summary sheet from an episode of @COREIMpodcast. I will be listening to this episode later). Would love to hear everyone's approach on treating bacteruria in patients with delirium.
coreimpodcast.com/2018/09/12/min…
coreimpodcast.com/2018/09/12/min…
• • •
Missing some Tweet in this thread? You can try to
force a refresh