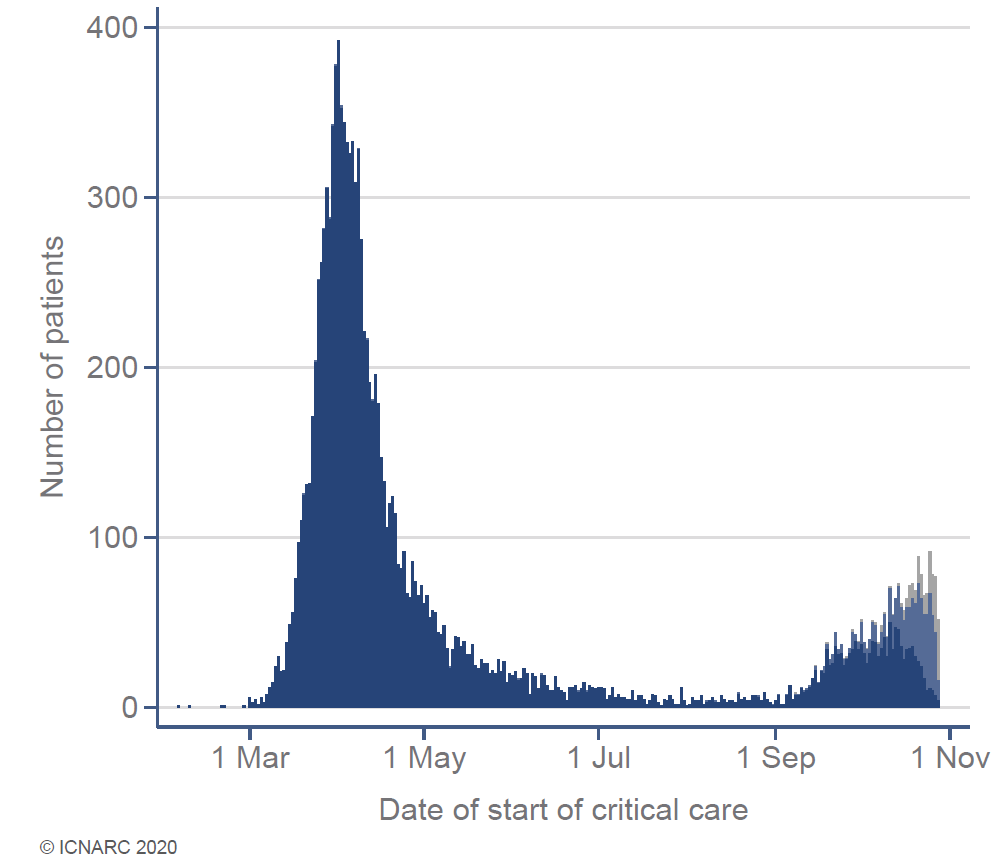
Routine NHS services under big pressure as COVID hospital admissions rise. We cancelled most surgery in the first wave including many cancer operations. Public, patient groups & doctors arguing strongly to keep surgery going this time. This will be a major issue within days. 1/15 

Throughout the NHS, we are desperately trying to avoid another major shut down of services. If you are ill, it is important that you contact your GP or come to hospital just as you normally would. We are busy but happy to see you. 2/15
Sadly, there will be many extra deaths during the pandemic from causes other than COVID-19. Hospitals almost completely shut down in Spring for all but the most urgent cases. Many patients stayed at home when ill, either not wanting to burden the NHS or afraid to come in. 3/15
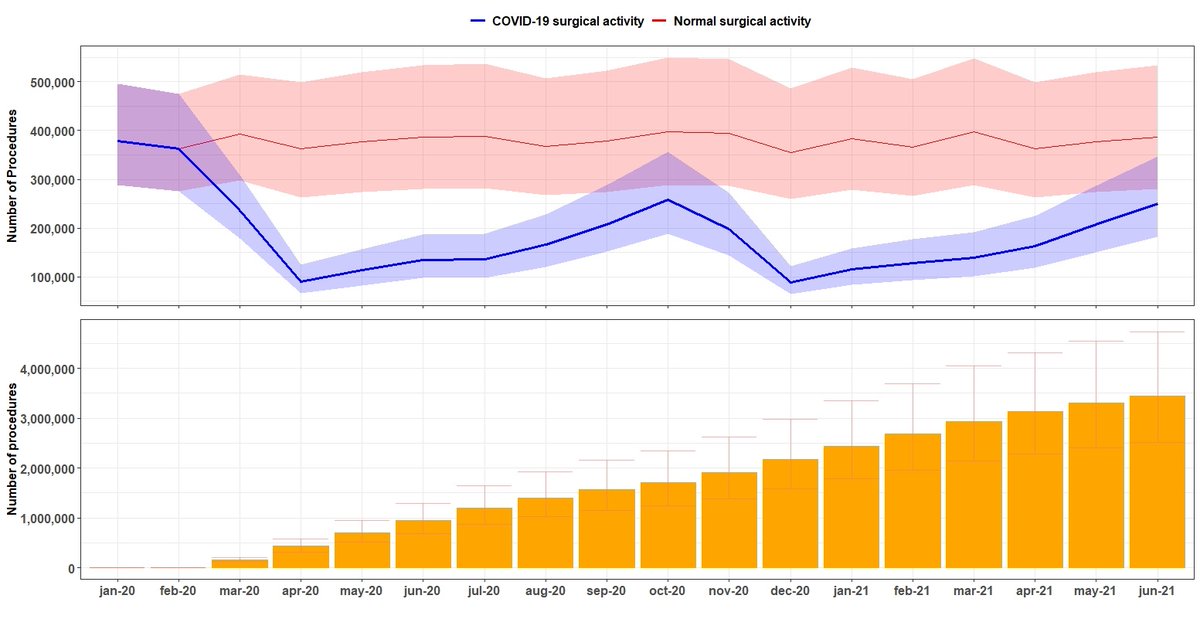
NHS surgeons normally do ~5 million operations a year. The impact of the first wave resulted in huge numbers of cancelled operations. Before the second wave, my colleagues @_alexfowler & @_tomabbott predicted 2 million missed surgeries by March ’21…. tinyurl.com/y3n78jeu 4/15 

...this predicted backlog is now much worse. If COVID-19 hospital admissions continue to rise, the NHS will have a backlog of >3.5 million surgical procedures by June '21. Here red line=normal, blue line is surgery during pandemic and yellow the growing backlog of surgeries. 5/15 
We have made extensive changes to keep NHS hospitals working safely. Hospitals are now split into four zones from Green (COVID free) to Blue (COVID positive). We restrict staff & patient movement between zones and test widely to keep green zones COVID-free. 6/15 
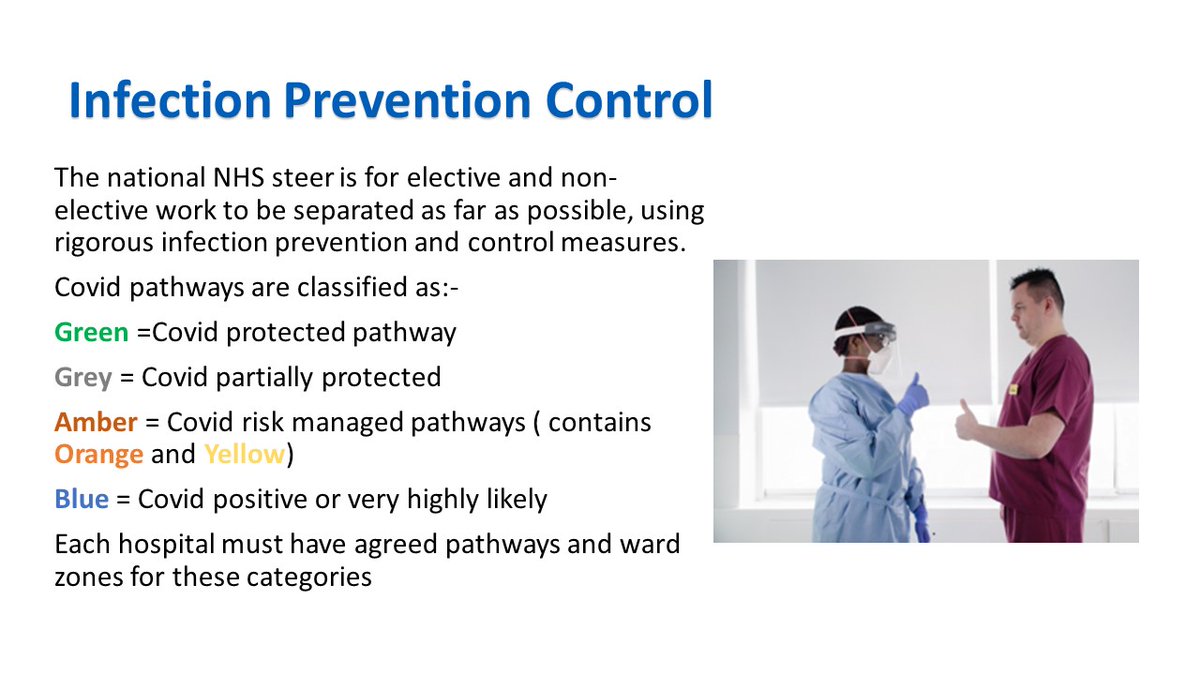
Excellent research from @aneelbhangu @DrJamesGlasbey & @CovidSurg shows ‘Green zones’ do protect patients having cancer surgery but don’t eliminate the COVID risk. Protection will weaken as community infections rise. Testing before surgery seems key. 7/15
ascopubs.org/doi/full/10.12…
ascopubs.org/doi/full/10.12…
Green zones are important because @covidsurg data show pulmonary complications are common for surgical patients infected with SARS-CoV-2. These complications can have a high mortality rate for older patients having major surgery. 8/15
thelancet.com/journals/lance…
thelancet.com/journals/lance…
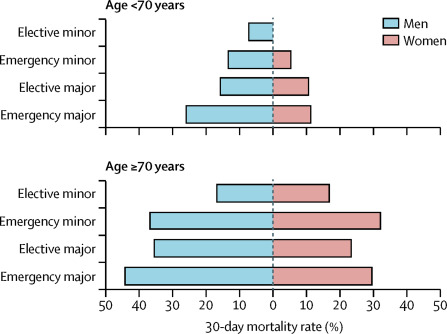
But other data suggest young patients having minor surgery are at little additional risk. Testing before minor surgery may be less important, but a few untested patients might then spread the virus while in hospital. How green should green zones be? 9/15
qualitysafety.bmj.com/content/early/…
qualitysafety.bmj.com/content/early/…
The new zones make hospitals inefficient. They aren’t designed to split into 4. Common spaces like entrances, corridors & lifts don’t work well. We screen patients before surgery and cancel those testing positive. It’s difficult to schedule other patients for vacated slots. 10/15
It's easy to think the substantial reduction in operations is because the NHS somehow 'decided' to treat COVID-19 patients instead. But even without the rise in COVID admissions, the huge challenge of providing surgery safely is really slowing us down. 11/15
We’re also seeing big reductions in patient referrals for diseases which need surgery. We don't know where these expected patients have gone. Sadly, whatever we do next, there will be many excess deaths from untreated surgical disease. 12/15
bma.org.uk/media/2841/the…
bma.org.uk/media/2841/the…
It will be very hard to keep going with NHS business as usual. We must protect patients from coronavirus in hospital. We have staff shortages due to infection, shielding and mental health problems. We now have winter bed pressures too. We're fighting several fronts at once. 13/15
These tensions can only increase as more patients catch SARS CoV-2 in hospital. As community infection rates rise, in-hospital rates will rise too. We can never completely prevent this. Sorry to see this issue already being politicised in Wales. 14/15
bbc.co.uk/news/uk-wales-…
bbc.co.uk/news/uk-wales-…
Politicians, media and public urgently need to understand that there is no way to safely deliver all the usual NHS care whilst treating every COVID-19 patient needing hospital admission. Trying to meet these impossible expectations will take a heavy toll on NHS colleagues. 15/15 

• • •
Missing some Tweet in this thread? You can try to
force a refresh