
As we come to terms with a second lockdown, some reflections on the latest report on Intensive Care admissions for COVID-19 published on Friday. A big shout out to the @ICNARC team and the many ICU staff who collect the data. 1/12
icnarc.org/Our-Audit/Audi…
icnarc.org/Our-Audit/Audi…

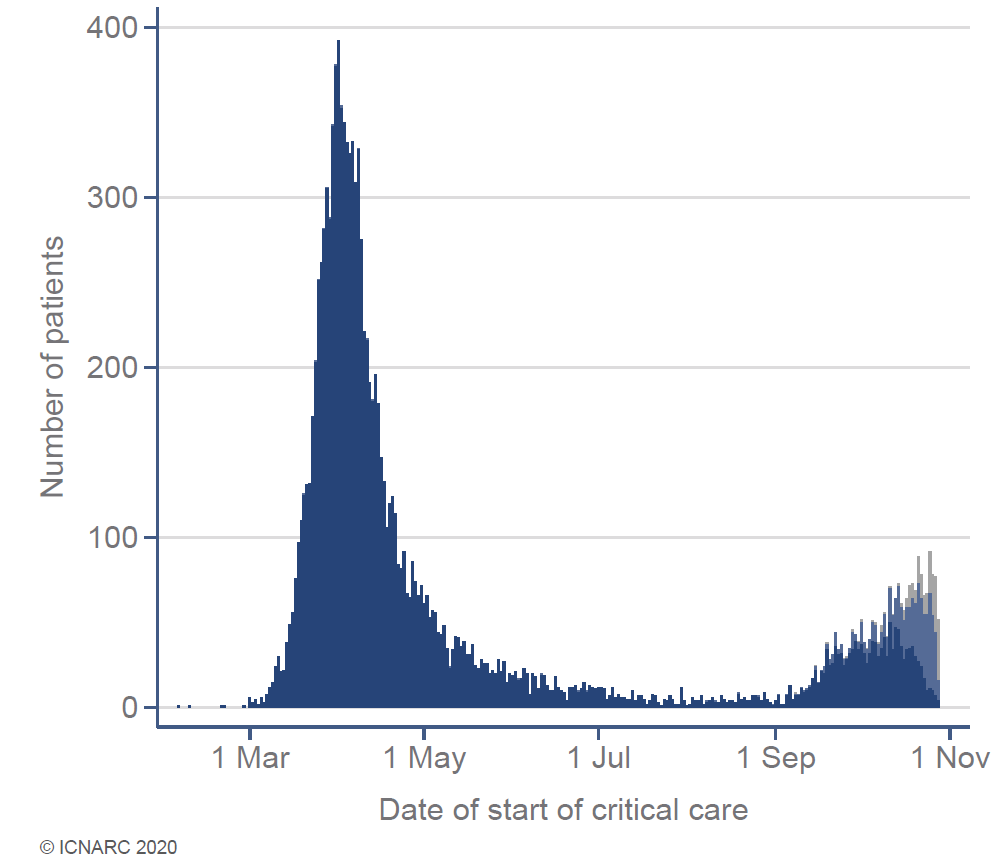
Patient admissions to Intensive Care with COVID-19 continue to rise steadily. The trajectory is slower than March but still enough to take us to those patient numbers by January. If we don’t stop this rise, even widespread use of temporary ICU facilities will not be enough. 2/12 
As expected, ICU admissions currently reflect the heavy impact of COVID-19 on the north of England. Some ICUs are already in trouble. Thoughts with friends and colleagues doing their very best in tough circumstances. 3/12 

In the second wave (since 01/09/20) we are seeing more COVID-19 patients admitted to ICU from areas of high social deprivation, likely reflecting the areas of the UK most affected. As with almost all diseases, the poor are hit hardest. 4/12 

We also have (since 01/09) a slightly higher proportion of white patients and a slightly smaller proportion of Black and Asian patients. This may reflect demographics in northern England. Importantly, admission rates now seem to better reflect local ethnicity distributions. 5/12 

@SundayTimes readers will be interested to see this graph which shows most COVID-19 patients admitted to intensive care are over 60 years and a significant number are over 80 years. This shows elderly patients are offered ICU care if doctors think they can benefit. 6/12 

So far in the second wave, we are seeing roughly half the number of patients being placed on a ventilator. The mortality rate for ICU patients also remains about half that in the first wave (19% vs 39%). Together these observations seem very important because…. 7/12 

…it may mean a) COVID-19 is getting less severe b) we are better at treating the disease or c) we have changed treatment strategy with more patients getting facemask ‘CPAP’ and fewer sedated & ventilated. 8/12
But it’s too early to know if SARS CoV-2 is getting less virulent. We may be better at treating it but not enough to halve mortality (that would be incredible). In this graph mortality in different risk groups since 01/09/20 (yellow) is mostly similar to first wave (blue). 9/12 

Survival may be a little better but the patients (casemix) admitted since 01/09 are less sick than the first wave. They need fewer treatments and less time in ICU. Thats because (since 01/09) we had enough ICU beds to admit the less seriously ill patients. That is changing. 10/12
A big note of caution before we reflect on whether ICU outcomes are better or worse. Half the patients admitted to ICU since 01/09/20 are still in hospital. They may not have died from COVID-19 but they haven’t survived yet either. Outcome data are incomplete. 11/12 

My interpretation of the ICU outcomes data hasn't changed since this earlier thread: I hope we are getting better at treating COVID-19 but only time will tell. Winter is coming and ICUs will be very full even with the lockdown. 12/12
Photos @jometsonscott

Photos @jometsonscott
https://twitter.com/rupert_pearse/status/1317453371784237058?s=20

• • •
Missing some Tweet in this thread? You can try to
force a refresh





