1. Clickbait title but content worth discussing- my thoughts over the next few tweets
➡️Questions around AMI definition.
Dr Taggart and others were part of the discussions that agreed to AMI definition. I think it was right because- see2.
medscape.com/viewarticle/93… via @medscape
➡️Questions around AMI definition.
Dr Taggart and others were part of the discussions that agreed to AMI definition. I think it was right because- see2.
medscape.com/viewarticle/93… via @medscape
2. an endpoint should have same prognostic impact in each trial arm. EXCEL definition does, UDMI doesnt
however:
➡️Should probably only include spontaneous AMI post procedure (>72 hrs), whatever definition you use, CABG better in long term
however:
➡️Should probably only include spontaneous AMI post procedure (>72 hrs), whatever definition you use, CABG better in long term
3. ➡️I personally dont think perceived COI have had any impact on the running / outcomes of the trial. Without industry support this trial would never have happened, nor would have many other fundamental trials. This is a smoke screen
4. ➡️Question around data & safety monitoring board (DSMB) requesting an analysis without time capping is a concern.
- why was this request turned down? would be interested 2 see arguments against this.
Investigators should be duty bound to address concerns of DSMB where poss.
- why was this request turned down? would be interested 2 see arguments against this.
Investigators should be duty bound to address concerns of DSMB where poss.
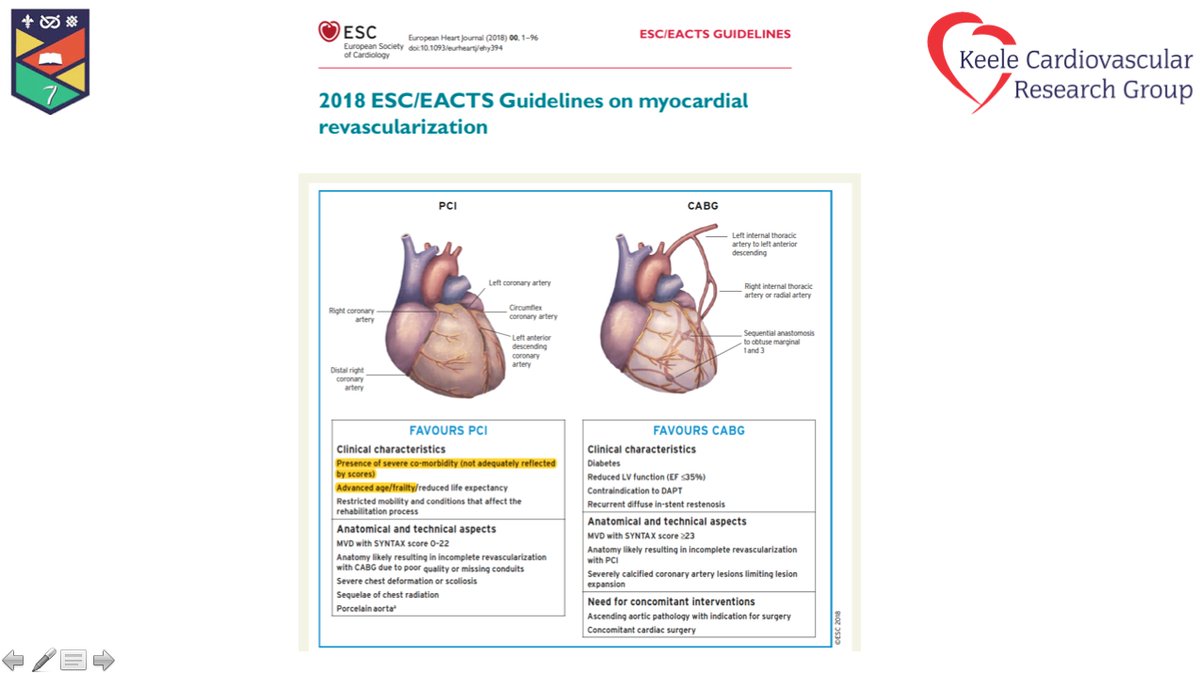
5. ➡️Question around guidelines
The authors of guidelines should not be the ones that have run the RCTs - there is a clear COI. If they are, then should not be involved in the parts that pertain to their trials, ie LMS recommendations.
The authors of guidelines should not be the ones that have run the RCTs - there is a clear COI. If they are, then should not be involved in the parts that pertain to their trials, ie LMS recommendations.
6. ➡️Independent reviews
When independent reviews are sought, in areas of stalemate- then these independent reviews should be circulated to all stakeholders. If this was not the case, then this is a serious problem of guideline committee, not the trialists.
When independent reviews are sought, in areas of stalemate- then these independent reviews should be circulated to all stakeholders. If this was not the case, then this is a serious problem of guideline committee, not the trialists.
7. ➡️Need for change in guidelines
Absolutely! because of the evidence that has accumulated from trials like EXCEL. @GreggWStone and colleagues should be congratulated for bring us this trial. but in my view, totality of evidence now does not support equivalence for PCI and CABG
Absolutely! because of the evidence that has accumulated from trials like EXCEL. @GreggWStone and colleagues should be congratulated for bring us this trial. but in my view, totality of evidence now does not support equivalence for PCI and CABG
8. ➡️It is my view that CABG should be class 1, PCI IIa for LMS.
CABG associated with long term ⬇️in spont AMI, need for rpt procedures (that have prognostic impact) and possibly a mortality impact (but not seen in totality of data)
CABG associated with long term ⬇️in spont AMI, need for rpt procedures (that have prognostic impact) and possibly a mortality impact (but not seen in totality of data)
9. Tone of article including "grubby" is unprofessional. LMS represents 3% of all PCI. LMS PCI is not a big market for stent companies.
10. There are some questions to be answered both around decsions taken by EXCEL but also guideline committee (see above)
➡️Remember, #EXCEL has given us wonderful data to inform management of this group of pts, but also discuss which endpoints to use and their impacts in trials
➡️Remember, #EXCEL has given us wonderful data to inform management of this group of pts, but also discuss which endpoints to use and their impacts in trials
11. Penultimately EXCEL has given us the data for much needed change in guidelines. In my view these should swing back towards CABG.
➡️EXCEL trialists should be congratulated in bring this trial to community
➡️But 2 questions above need to be answered
Finally...
➡️EXCEL trialists should be congratulated in bring this trial to community
➡️But 2 questions above need to be answered
Finally...
12. ➡️Need to think carefully about how guidelines are created and who is on them. Shouldnt be trialists that have run the trials.
To my mind this is the greatest COI, not the trial. Any external review should be transparent and available to all members of committee. The end 😉
To my mind this is the greatest COI, not the trial. Any external review should be transparent and available to all members of committee. The end 😉
• • •
Missing some Tweet in this thread? You can try to
force a refresh