So this really struck a chord with people. Let’s dive in.
https://twitter.com/drdagly/status/1326915822800023552
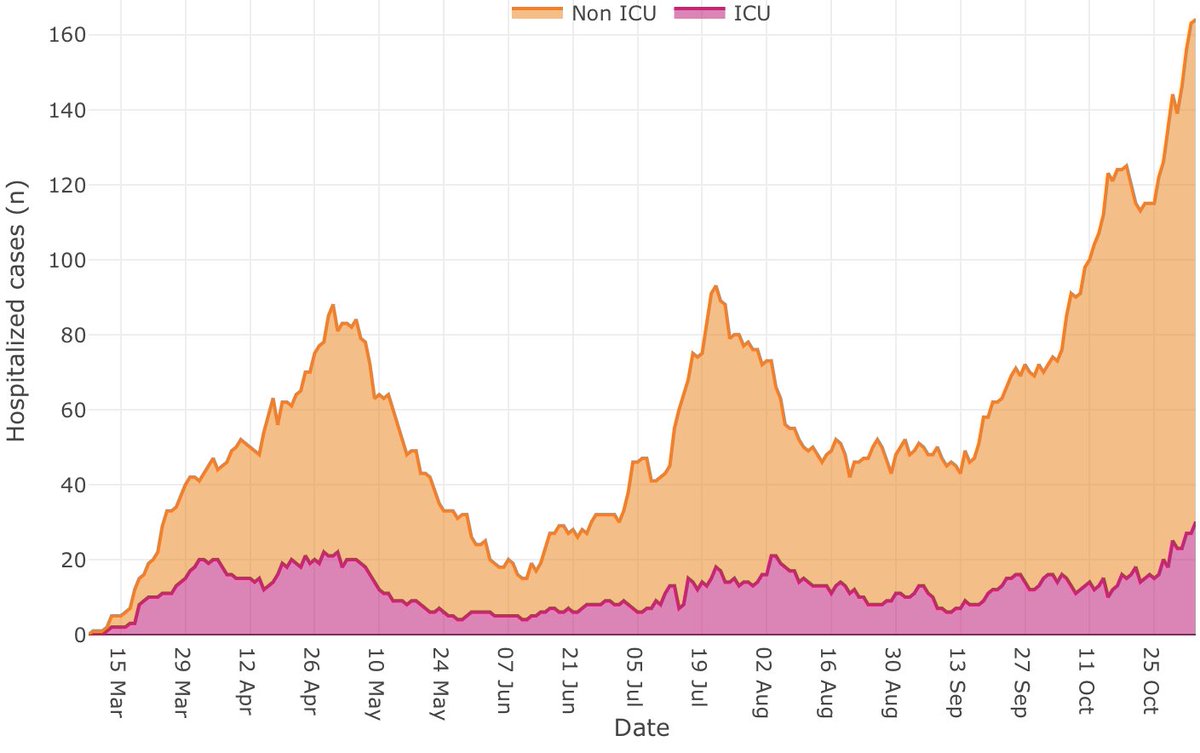
This is not where we are now, but given the ICU admission rates and EXPONENTIAL growth rate of cases, coupled with our inability to contact trace in a timely matter, this is where we are heading. Unless something is done.
If you are reading this thread, you are probably mostly in agreement with the problem. The challenge is to depoliticize this issue. We were all together on this in March, and as a result the first wave was brought under control. Our eastern provinces still have control.
This spread is coming from the community. This is not the fault of businesses or gyms. People are living their pre-Covid lives. However, our data is no longer accurate since contact tracing has been affected. We are using retrospective data. Soon we will be driving blind.
Here is how the hospital system will fail if nothing is done.
Increasing numbers of hospitalized COVID patients require isolation and cohorting. Most of our hospital has limited isolation rooms. Once these are full, it’s down to using algorithms to assess who is likely safe and can bunk together. This is dependent of low community numbers.
Higher incidences lead to more chances of guessing wrong. Higher cases in the hospital increase the risk of outbreaks. Outbreaks shut hospitals and ICUs down. Everything gets harder to accomplish. Patient movement grinds to a halt.
Outbreaks infect staff. Because of the absolute need to protect patients, this drops staffing numbers because of quarantine precautions and self isolation. Less staff, more work, more chances to cross contaminate.
We have a surge plan, and you hear a lot about it in the pressers. You hear that we have 750 beds. Let me be clear. I am uncertain how those can be staffed. Resources will need to be taken away from the rest of the hospital to run them, and this won’t be a normal ICU.
Standards of care will drop. That will be unavoidable. And that will effect all aspects of hospital and outpatient care. Worst case scenarios include triage, age limits for admission to the ICU, estimated benefits of therapy. Hard targets.
We have been told to take more personal initiative and responsibility. We’ve been given a two week time frame to do it. Most Albertans have done this. There is a limit to what individuals can accomplish without the support of government. We are at that limit. Now.
We can do this. But we need to get contact tracing back on line. We also need to get EVERYONE’S attention as to the serous nature of what is happening. That is the purpose of the circuit breaker shut down. Fast and hard and now.
If we don’t do this we will be flying blind. And there are mountains up ahead. This is what took New York down during the first wave.
So .... how would I manage this? Two scenarios based on what our government is doing to deal with community numbers.
Scenario 1: Measures in place, cases plateauing. I’ve got wiggle room. Priority is mother. She’s a quick surgical fix and will require a short stay. Prevent complications and she’s in and out, and there to care for her kids.
Trauma victim: as long as there is no head injury, and I still have OR resources he should be in and out in a week, if he was previously healthy and doesn’t have COVID. (He’s in a high prevalence demographic). That’s reasonable.
COVID nurse. Our mortality numbers have dropped a lot with resourced 1 on 1 care to under 30%. If she has no other problems and no renal failure we can save her, but it’s a 2 week buy in. She will be unwell for months afterwards and still require advanced post ICU care.
Scenario 2: full surge with no foreseeable plateau.
1. Mom takes priority.
2. Trauma gets surgical mgt if OR availability, an epidural pain block and sent to trauma ward.
3. Nurse receives aggressive ward care and palliation if it fails.
1. Mom takes priority.
2. Trauma gets surgical mgt if OR availability, an epidural pain block and sent to trauma ward.
3. Nurse receives aggressive ward care and palliation if it fails.
• • •
Missing some Tweet in this thread? You can try to
force a refresh