
“Just listen to your patient, he is telling you the diagnosis.“ — William Osler
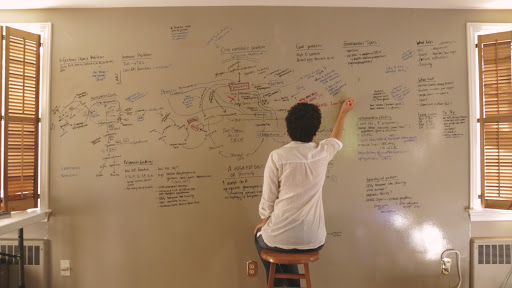
My problem: I was a novel, when all my doctor really wanted or had time for was a tweet.
My problem: I was a novel, when all my doctor really wanted or had time for was a tweet.
That is the reason I have been ill for the better part of a decade. It was all there: diagnosable, treatable, actionable. I simply had too many things wrong with me at once. I was, in a sense, too sick for medicine.
I think I may have stumbled upon my final, outstanding diagnosis, the rare thing that could explain all the dangling symptoms that my other “rare” diagnoses cannot. I’ll never be able to prove it (unless, perhaps, I have another acute episode).
I don’t even want to attempt to talk to a neurologist about this. I can’t.
I think I have been having transient symptoms of corpus callosum disconnection syndrome (also known as “split brain”) for years, secondary to inflammation, edema, infection or some combination of the three.
The corpus callosum is what allows the left and right hemispheres of the brain to communicate. What are the symptoms that lead me to suspect this?
For one, after I got sick, I lost the ability to clap my hands. Clapping would cause immediate confusion and distress. I would maybe get three claps in and then my hands would freeze. I would look at them, confused, distressed, unable to understand them.
Clapping requires left/right brain coordination, since the left hemisphere controls the right hand and vice versa.
Disconnection syndrome could also plausibly account for transient agnosia (of objects, people, and occasionally my own face), agraphia (specifically, the right side of letters), and expressive aphasia.
None of this occurred to me until I had even more profound symptoms of a combination of possible corpus callosum and temporal lobe dysfunction in the context of high-dose prednisone use (I suspect HSV-1 replication *in my brain* may have been the culprit).
The lateralization of my brain functions became...extreme and obvious. Why am I sharing this? I guess because it is the only way that I learn.
While I suspect that what I dealt with may be truly rare, inevitably, when I share, I usually encounter someone out there who has experienced something similar, too.
Even eight years on, the more I learn, the harder and harder it gets to have any faith in medicine, neurology in particular.
Many of these symptoms I had in 2012. A neurologist in the MGH ER told me this was “the most common thing they see.” I got the hardware/software lecture. I was told it was a migraine aura. I have never in my life had a migraine.
And I guess...I wish someone could have told me in 2012: “The seven distinct pathologies/pathophysiologies you are experiencing do exist. They are in the medical literature. They are happening all at once because this is what infections can do...”
“...They are measurable, diagnosable, and treatable. But do not expect that any doctor is going to find them for you. They will all be looking for one thing, not seven, which means they are setting themselves up to fail you from the get-go...“
“...It’s not their fault—this is how they were trained. But you are on your own, kid. And the sooner you realize that, and the sooner you start hitting PubMed, the better off you will be.”
To be fair to myself, I really did try, but I made a fatal error. I assumed that because my one brain scan was ”normal” (it actually wasn’t) that my answers were to be found in the very small. In the biochemical or the molecular. 
No doubt, my disease process is happening at the molecular/biochemical level. However, it is probably happening on *many levels* of resolution, and so I should have been looking at *every level of resolution* for clues, diagnoses, treatments.
My regret is that I did not sit down, take out my list of 40+ symptoms and try to tie every dysfunction to the component of the nervous system that is responsible for the normal operation of that function.
I could have created a heat map of my body that would have lead to/implied potential diagnoses that were never on any doctor’s differential diagnosis list. Had I done this, I might have found the experts who could have helped me, and avoided years of needless suffering.
I know you might be thinking, “It’s not your fault, Jen. It was your doctors’ job to figure it out.” To which I would say, never give anyone that kind of power.
My diagnoses: craniocervical instability, atlantoaxial instability, intracranial hypertension, tethered cord syndrome, compression of the internal jugular vein by the omohyoid muscle, ME/CFS, POTS, MCAS, and (possibly) a L/R hemisphere disconnection syndrome.
• • •
Missing some Tweet in this thread? You can try to
force a refresh


