Images of Infectious Diseases
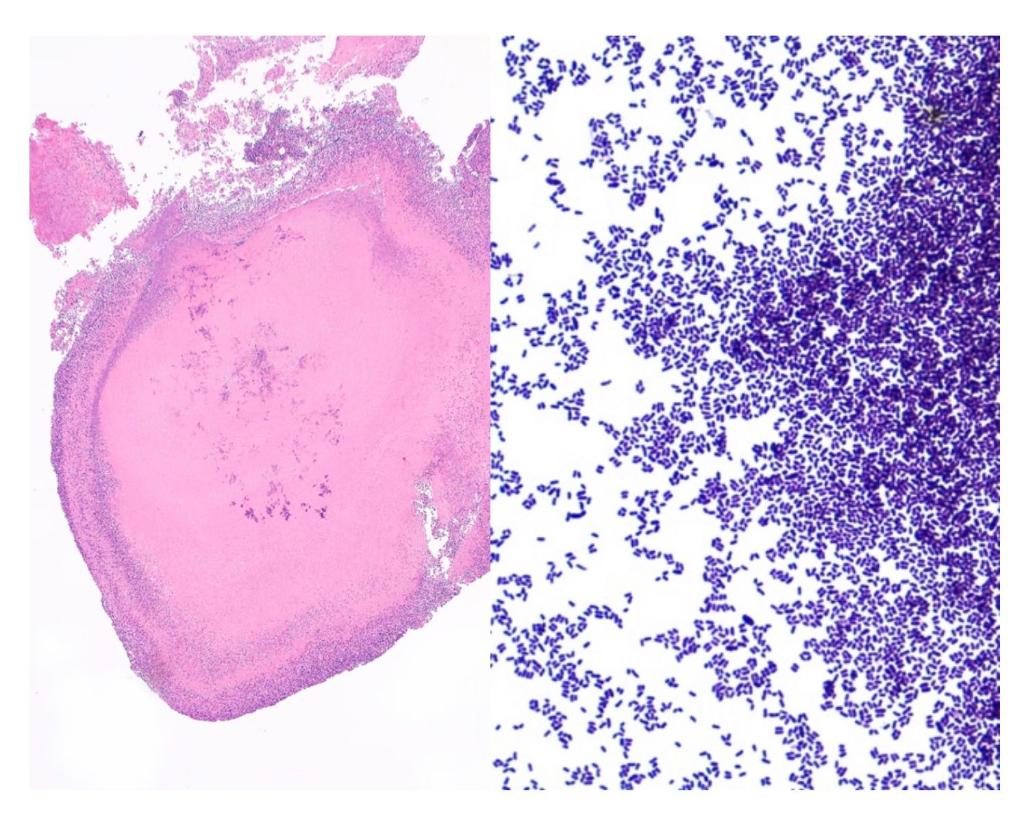
6 mo post-tx: H&E (400x) of cervical biopsy of 46F s/p living unrelated donor kidney tx for adult PCKD.
Belatacept. MMF. Prednisone.
Acute cellular + antibody-mediated rejection.
CMV D+/R-. valganciclovir prophylaxis.
DDx / Rx? #MayoIDQ next
6 mo post-tx: H&E (400x) of cervical biopsy of 46F s/p living unrelated donor kidney tx for adult PCKD.
Belatacept. MMF. Prednisone.
Acute cellular + antibody-mediated rejection.
CMV D+/R-. valganciclovir prophylaxis.
DDx / Rx? #MayoIDQ next

2/
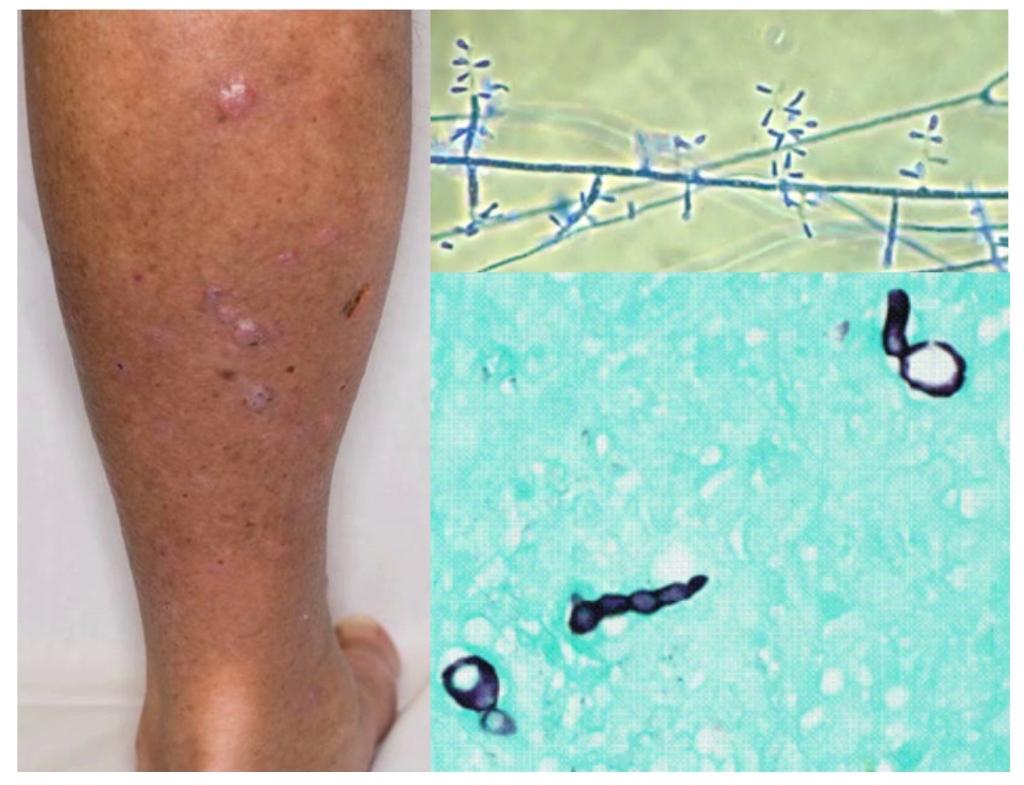
Case diagnosis: breakthrough CMV disease with cervicitis
H&E intranuclear / intracytoppasmic inclusions within endothelial cells in ectocervical stroma.
Immunohistochemistry stain for CMV shows infected endothelial cells with CMV inclusions.
doi.org/10.1111/tid.13…
Case diagnosis: breakthrough CMV disease with cervicitis
H&E intranuclear / intracytoppasmic inclusions within endothelial cells in ectocervical stroma.
Immunohistochemistry stain for CMV shows infected endothelial cells with CMV inclusions.
doi.org/10.1111/tid.13…

3/
#MayoIDQ Breakthrough CMV disease, while receiving valGCV prophylaxis, is concerning for over-immunosuppression, under-dosing of val GCV, and/or drug-resistant virus.
If gene sequencing shows the most common CMV gene mutation, what drug would be recommended Rx?
#MayoIDQ Breakthrough CMV disease, while receiving valGCV prophylaxis, is concerning for over-immunosuppression, under-dosing of val GCV, and/or drug-resistant virus.
If gene sequencing shows the most common CMV gene mutation, what drug would be recommended Rx?
4/
#CMV in kidney #transplantation
Risks:
1. CMV D+/R- mismatch
2. Rejection: cellular / antibody-mediated
3. T cell depletion: thymoglobulin, alemtuzumab
4. T cell dysfunction: combined IS
5. Low ALC <610
doi.org/10.1111/tid.13…
#CMV in kidney #transplantation
Risks:
1. CMV D+/R- mismatch
2. Rejection: cellular / antibody-mediated
3. T cell depletion: thymoglobulin, alemtuzumab
4. T cell dysfunction: combined IS
5. Low ALC <610
doi.org/10.1111/tid.13…
5/
#CMV #belatacept
Belatacept - selective T-cell costimulation blocker. Binds CD80 / CD86 on antigen-presenting cells —> block CD28-costimulation of T cells
High risk of CMV disease and prolonged viral replication in CMV D+/R- kidney recipients
doi.org/10.1111/ajt.16…
#CMV #belatacept
Belatacept - selective T-cell costimulation blocker. Binds CD80 / CD86 on antigen-presenting cells —> block CD28-costimulation of T cells
High risk of CMV disease and prolonged viral replication in CMV D+/R- kidney recipients
doi.org/10.1111/ajt.16…
6/
Resistant / refractory #CMV
Risks: prolonged GCV use in face of lack of CMV-immunity due to prolonged intense over-immunosuppression
1. CMV D+/R-
2. High level immunosuppression (e.g., due to rejection)
3. Prolonged antiviral use
link.springer.com/article/10.100…
Resistant / refractory #CMV
Risks: prolonged GCV use in face of lack of CMV-immunity due to prolonged intense over-immunosuppression
1. CMV D+/R-
2. High level immunosuppression (e.g., due to rejection)
3. Prolonged antiviral use
link.springer.com/article/10.100…
7/
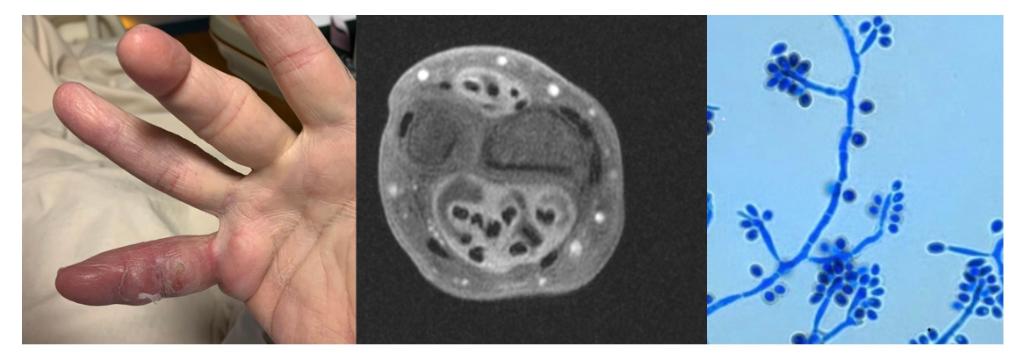
Resistant #CMV mutations
UL97 mutation most common: impairs GCV phosphorylation
- GCV (and Maribavir)
UL54 polymerase mutation
- GCV/cidofovir (often cross-resistant)
- Foscarnet (pyrophosphate binding)
UL56 terminase mutation
- Letermovir
doi.org/10.1080/216787…
Resistant #CMV mutations
UL97 mutation most common: impairs GCV phosphorylation
- GCV (and Maribavir)
UL54 polymerase mutation
- GCV/cidofovir (often cross-resistant)
- Foscarnet (pyrophosphate binding)
UL56 terminase mutation
- Letermovir
doi.org/10.1080/216787…
8/
Resistant #CMV Rx
1. Reduce immunosuppression
2. UL97 mutation: foscarnet drug of choice (answer to MCQ: 74% correct)
Why not:
Cidofovir - 2nd choice (after foscarnet)
Maribavir - investigational
Letermovir- not approved in SOT/Rx
doi.org/10.1111/ctr.13…
Resistant #CMV Rx
1. Reduce immunosuppression
2. UL97 mutation: foscarnet drug of choice (answer to MCQ: 74% correct)
Why not:
Cidofovir - 2nd choice (after foscarnet)
Maribavir - investigational
Letermovir- not approved in SOT/Rx
doi.org/10.1111/ctr.13…
/9
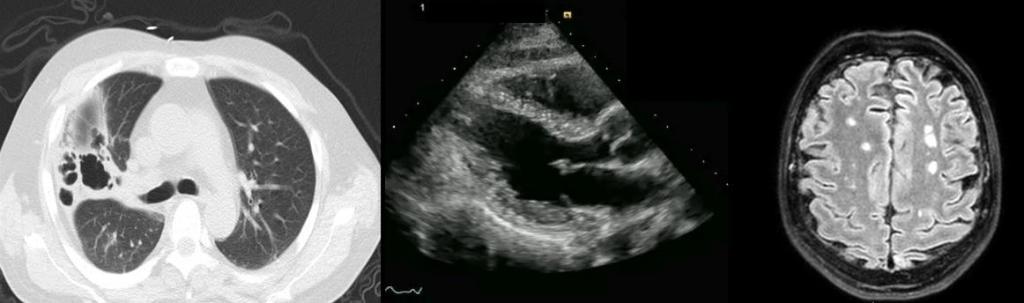
Case resolution:
Breakthrough CMV disease
Risks: D+/R-, cellular and humoral rejection, over immunosuppression, belatacept
H/o cervix adenoma malignum. Biopsy: invasive CMV disease.
Prolonged Rx w/ foscarnet and cautious reduction in IS.
doi.org/10.1111/tid.13…
Case resolution:
Breakthrough CMV disease
Risks: D+/R-, cellular and humoral rejection, over immunosuppression, belatacept
H/o cervix adenoma malignum. Biopsy: invasive CMV disease.
Prolonged Rx w/ foscarnet and cautious reduction in IS.
doi.org/10.1111/tid.13…
• • •
Missing some Tweet in this thread? You can try to
force a refresh