Spoke too soon. Two weeks ago I was hopeful that the second COVID tide was starting to turn. Things weren’t easy but had stabilised and national numbers were down. Now we're seeing rising numbers at national level in and several regions, including where I work in east London. 1/7 

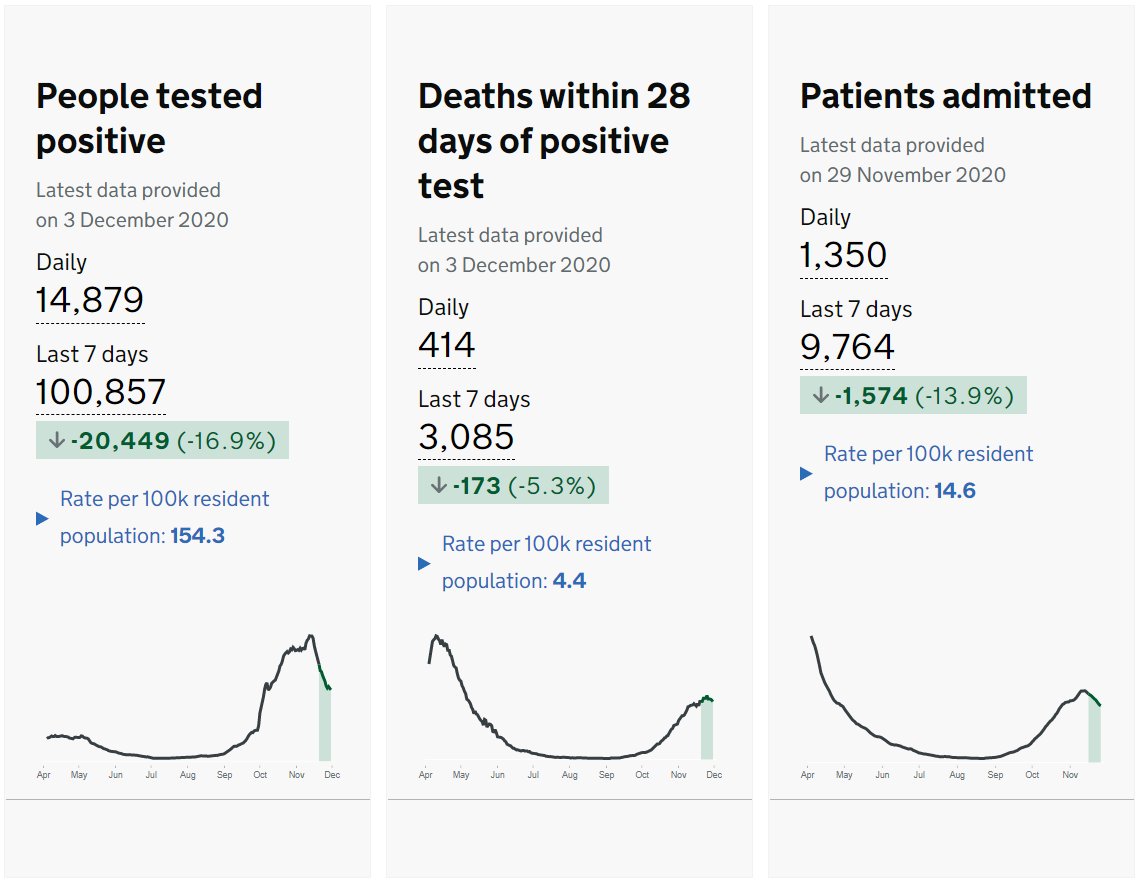
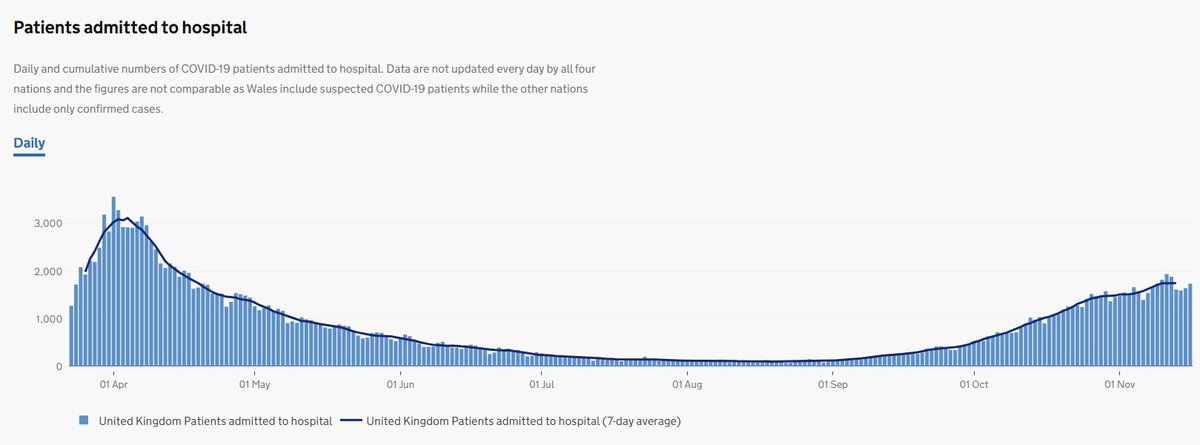
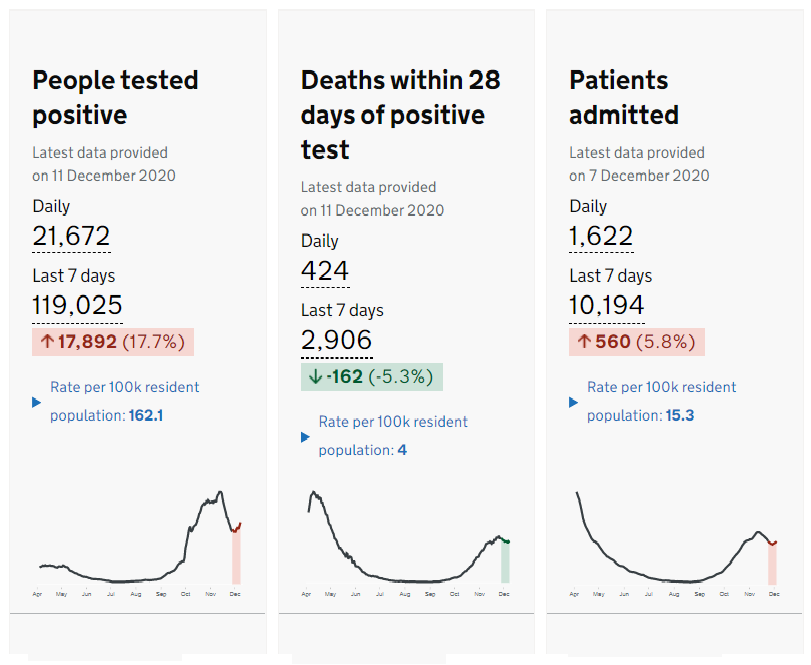
The number of people testing positive for SARS Cov-2 is definitely up in the last 7 days, while the number of patients admitted to hospital with COVID-19 is beginning to rise, and the number of deaths (which lags behind admissions) was falling but has now levelled off. 2/7 
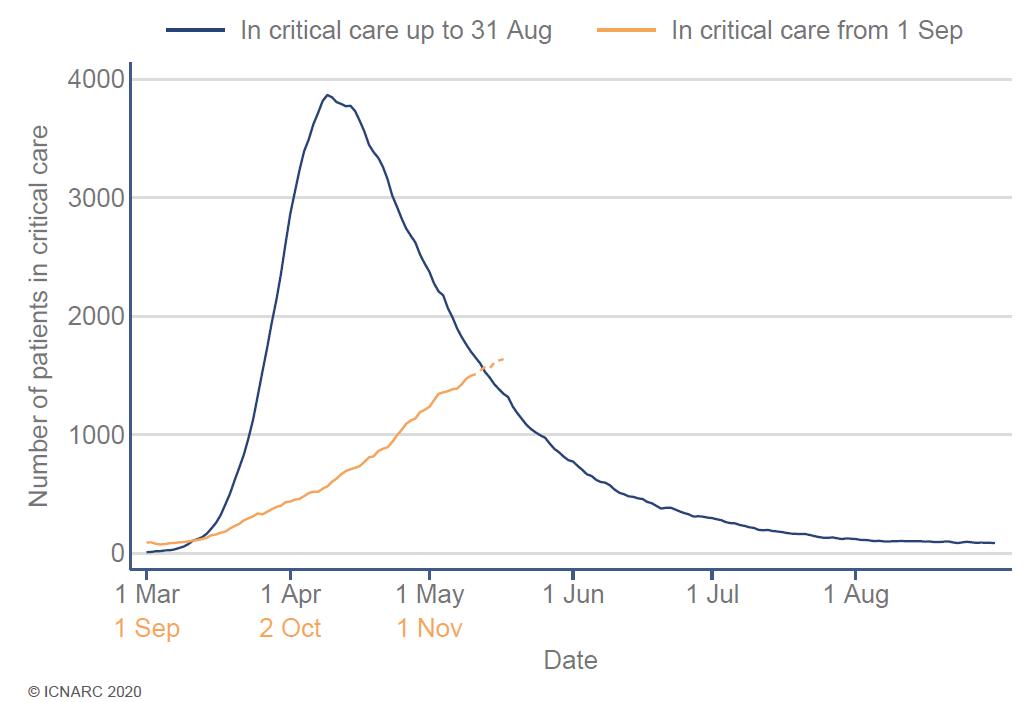
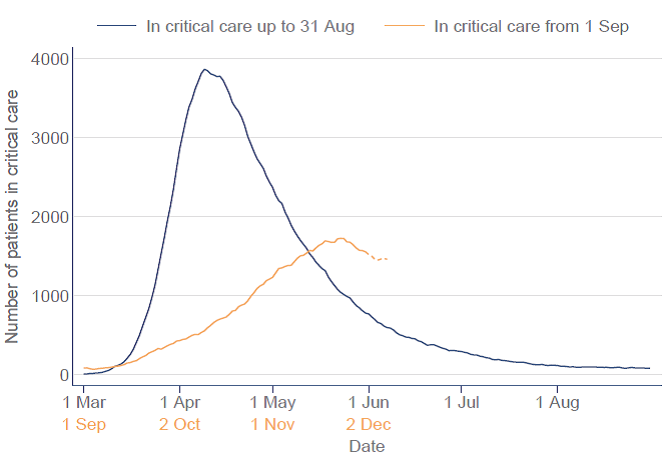
Government data fit with the independent data from @ICNARC describing intensive care admissions. The number of patients in ICU with COVID-19 appeared to be falling 7 days ago but not any more. 3/7 
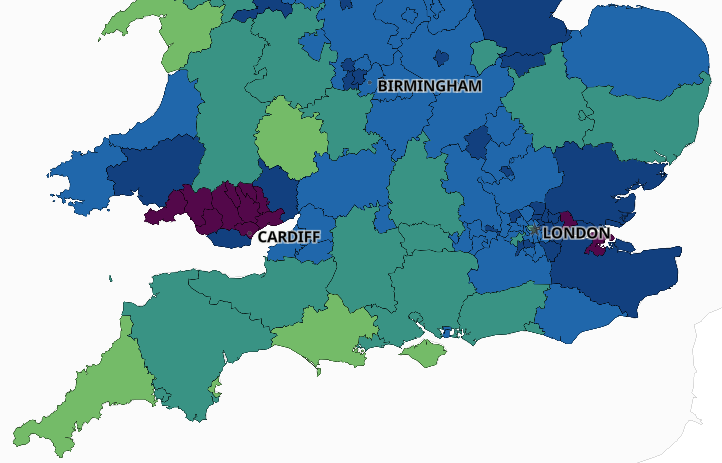
Sadly these national data fit with local experiences of doctors. Hospitals are very busy in hotspots in various areas such as south Wales, east London and north Kent. Some good news: numbers are falling in the north of England and Northern Ireland. 4/7 
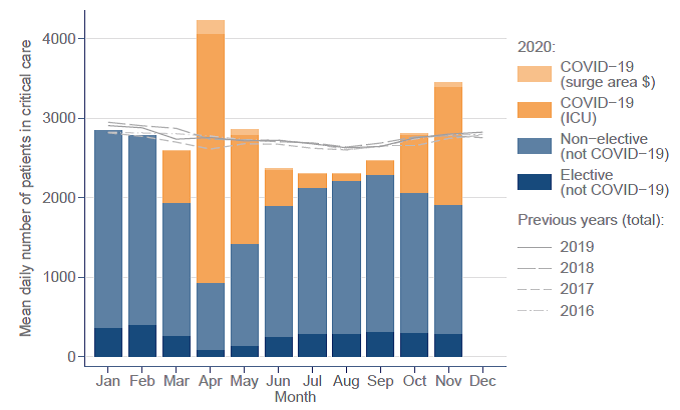
NHS hospitals are still looking after a lot of patients with ‘usual’ medical problems (strokes, heart attacks, surgery, etc) but these services are being increasingly squeezed by the need to deliver COVID care. Some elective work will have to stop soon. 5/7 
The coronavirus will be with us for a long time to come, even if not at pandemic levels. Years even. Vaccines will really help but it will be spring before we have achieved population levels of immunity through vaccination. Our main defence is STILL #HandsFaceSpace 6/7
Sorry there isn't new or better news. NHS staff are really grateful for all you are doing but please keep up the good work. Think carefully about your Christmas plans. Get vaccinated if you can (I definitely will) and stay safe. #DocsForVax 7/7 

• • •
Missing some Tweet in this thread? You can try to
force a refresh