As the NHS enters what will likely be our hardest ever winter, what about the Nightingales….? is a common question, and for some a retort to news that hospitals are struggling to deliver routine patient care in the face of a rapidly rising patient admissions for COVID-19. 1/10
The speed with which the Nightingale Hospitals were established, and our need to believe in them, has left us with the impression that building a major NHS hospital within a few weeks is a thing we can easily do. It isn’t. 2/10
The old Nightingale style wards had rows of beds down each wall. A few nurses could have sight of many patients, and easily communicate with each other. If a patient has a problem (e.g. cardiac arrest) it is easy to spot and help arrives faster. Photo: Wellcome Collection. 3/10 

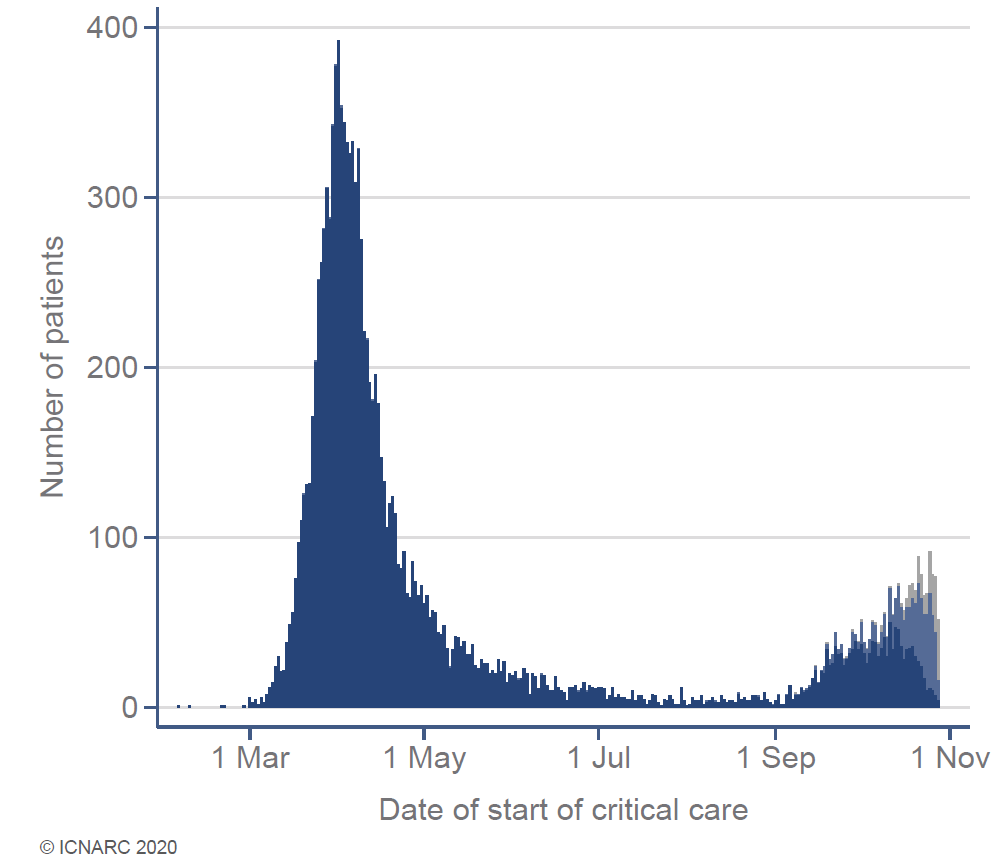
The Nightingale layout was an obvious choice for temporary field hospitals when staff are limited. In the spring, these were set up across the UK, but opened as the first wave had passed it’s peak. Happily, most weren’t needed. 4/10
en.wikipedia.org/wiki/NHS_Night…
en.wikipedia.org/wiki/NHS_Night…

We may think of a hospital as a building with beds in it, but it’s much more a large team of very skilled people working alongside each other. There are more than 350 NHS career paths. This from @charlot_summers..… 5/10
theguardian.com/commentisfree/…
theguardian.com/commentisfree/…
The hospital culture of safety and quality cannot be prefabricated. Hospitals aren’t run they are led. Doctors & nurses have been saying this since January when work started on the Huoshenshan temporary hospital in Wuhan. 6/10
bbc.co.uk/news/in-pictur…
bbc.co.uk/news/in-pictur…
Nightingales cannot provide A&E depts, surgery or the advanced diagnostics of a modern NHS hospital. They can’t handle the huge variety of illnesses which may need hospital care and are best focussed on one disease or part of patient care e.g. recovery & rehabilitation. 7/10
This recent thread from Birmingham surgeon @aneelbhangu explains some of the technical challenges and the complex way different hospital departments interact to deliver surgical treatments for patients. 8/10 
https://twitter.com/aneelbhangu/status/1324086905684824064?s=20

The CLAP study led by an @EdinburghUni team highlights problems with redeployed staff who don’t know each other, working in unfamiliar environments without the right training or experience. There are risks both to patient care and staff well-being. 9/10
ed.ac.uk/usher/biomedic…
ed.ac.uk/usher/biomedic…
Temporary Nightingale hospitals play a role, ensuring we have a hospital bed for every patient. But they are a last resort for exceptional circumstances, not a quick solution to avoid lockdown or depressurise routine NHS services. We should not use them until we have to. 10/10 

• • •
Missing some Tweet in this thread? You can try to
force a refresh