An update from ground level across the UK NHS. Things are very different to March. UK COVID-19 projections continue to look more like a ‘slow burn’ than a second wave. But the NHS is under very definite and increasing strain. We are going to have a long hard winter…… 1/12 

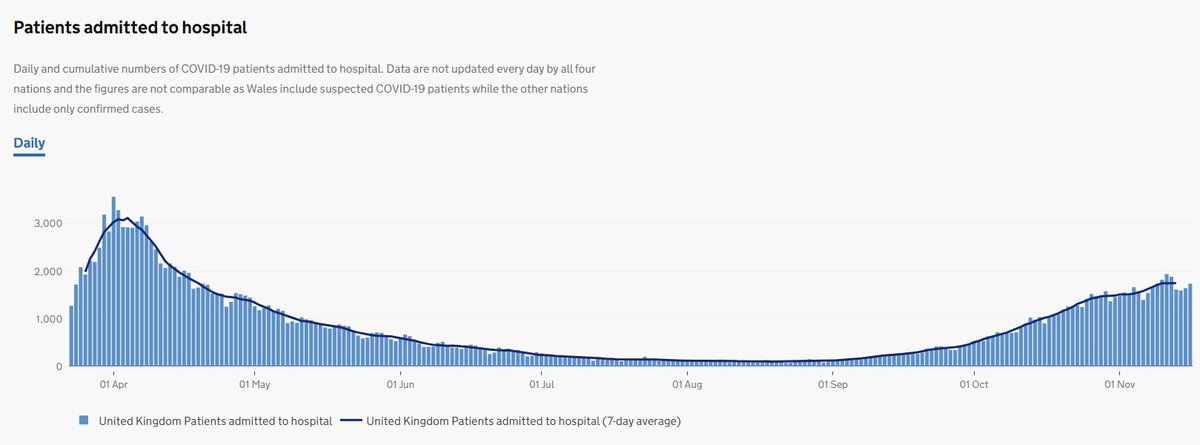
COVID-19 hospital admissions continue to rise. Now 1750 new patients/day. Much less than the mid-April peak of 3100/day but we will reach that same rate in 8 weeks unless the rise slows. It takes at least four weeks for the lockdown to take effect. Perhaps it will soon? 2/12 
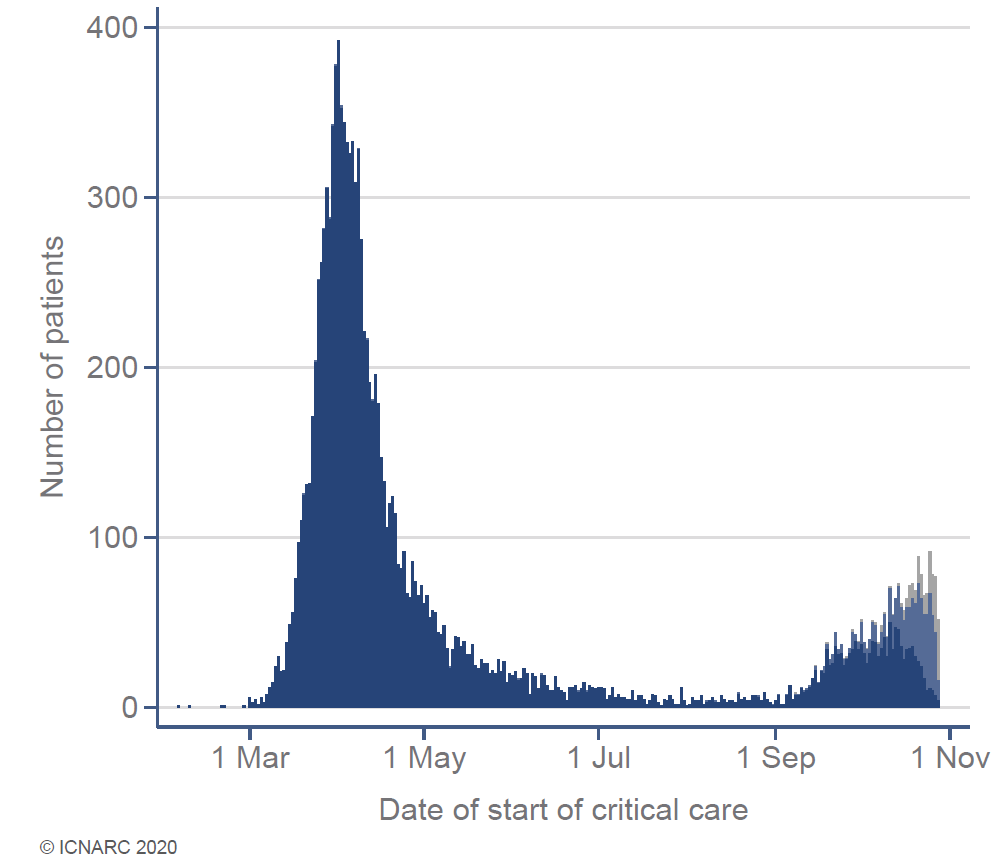
The same pattern is reflected in @ICNARC (independent) data describing COVID-19 admissions to intensive care units: 140 new patients/day and rising with >1500 COVID patients currently in ICU… 3/12 
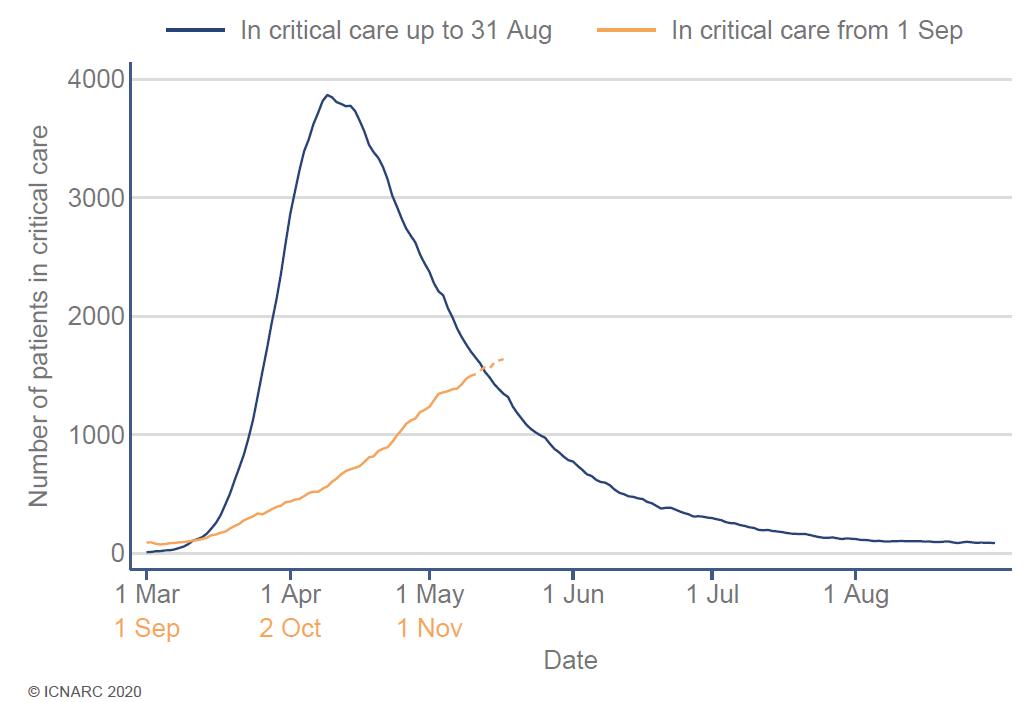
…and in government data describing and the number of COVID-19 patients ‘in mechanical ventilation beds’ (i.e. an ICU bed): Currently 1400 patients (compared to a peak of 3250 in mid-April). NB the numbers in 3 and 4 are defined & calculated differently. 4/12 

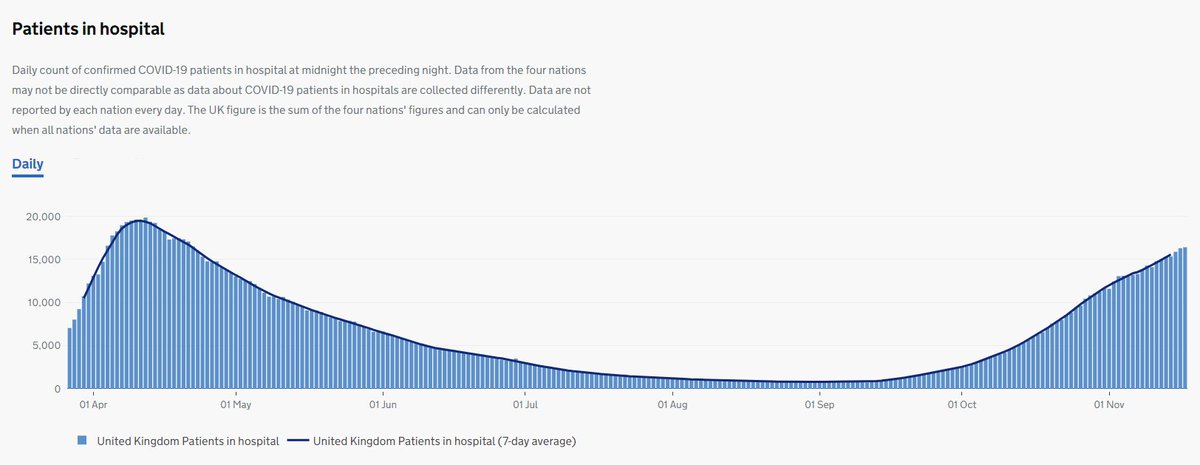
The most important graph is this one. We currently have 15,000 hospital in-patients with COVID-19 and rising compared to the April peak of 20,000 COVID-19 in-patients. But we now have a greater number of patients with other illnesses too (non-COVID pts not shown in graph). 5/12 
.@ICNARC data show we are still putting fewer patients who need ICU on a ventilator than the spring (23% vs 54%). Mortality after ICU also remains lower (23% vs 40%). But REMEMBER: 45% of these patients are still in hospital. They haven’t died but they have yet to survive. 6/12
We could be getting better at treating COVID-19, or the virus may be getting less virulent (harmful). A major reason is that hospitals don't YET have the massive overload of patients we saw in April. This affects which patients go to ICU and the average severity of illness. 7/12
This week I have been chatting with friends working in NHS hospitals across the UK. They report a common experience of struggling to deliver care not only for COVID-19 patients but many more with a wide range of ‘usual’ problems including cancer, heart disease and trauma. 8/12
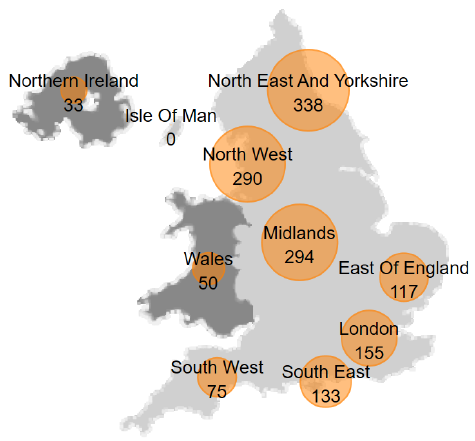
The north of England is still the worse affected with the majority of patient admissions to intensive care in the past 14 days. A few hospitals are shutting down some usual services. ICU admissions are also rising fast in some quieter parts of the country. 9/12 
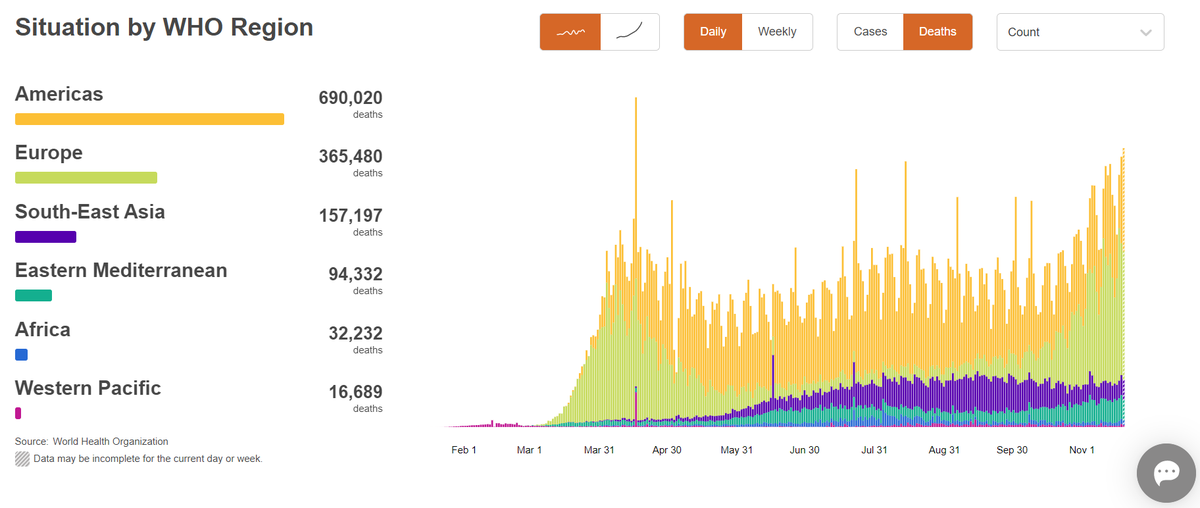
Speaking to ICU doctors around the world in an online meeting this week reveals a similar story in many countries. Things especially bad in the USA, Poland & Romania, but Australia has the virus under control coming into the southern hemisphere spring. 10/12 
The NHS heads into the winter months with many hospital beds occupied by patients with a highly infectious disease. This will definitely be my hardest NHS winter since 1999/2000 when we had a very bad flu season, and probably the hardest of my career. 11/12
NHS staff remain committed and determined to care for every patient with every illness. But we face inevitable media & political scrutiny, some of which will be misleading and negative. I will continue to share objective facts as I see them. Thanks for all your support. 12/12 

• • •
Missing some Tweet in this thread? You can try to
force a refresh