Evaluation and Management of Patients With Stable Angina: Beyond the Ischemia Paradigm
@JACCJournals @ACCinTouch @DLBHATTMD @ESC_Journals @mmamas1973 @ErinMichos @mirvatalasnag @aayshacader @iamritu @AntoniousAttall @Cosyns @ThorEdvardsen @DavidLBrownMD @venkmurthy
#YesCCT



@JACCJournals @ACCinTouch @DLBHATTMD @ESC_Journals @mmamas1973 @ErinMichos @mirvatalasnag @aayshacader @iamritu @AntoniousAttall @Cosyns @ThorEdvardsen @DavidLBrownMD @venkmurthy
#YesCCT
https://twitter.com/accintouch/status/1337827295067844609

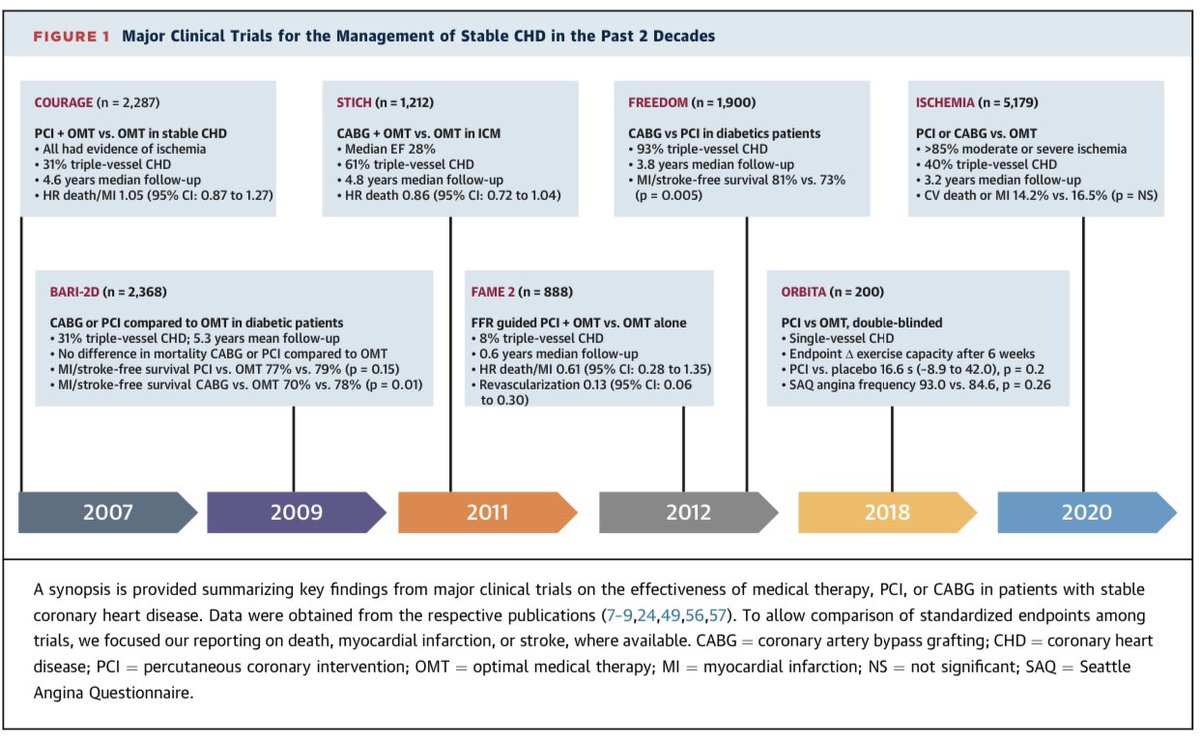


📝 Major Clinical Trials for the Management of Stable CHD in the Past 2 Decades
📌COURAGE (2007)
📌BARI-2D ( 2009)
📌STICH (2011)
📌FAME-2 (2012)
📌FREEDOM (2012)
📌ORBITA (2018)
📌ISCHEMIA (2020)
@mmamas1973 @mirvatalasnag @ErinMichos @DavidLBrownMD @DLBHATTMD @iamritu
📌COURAGE (2007)
📌BARI-2D ( 2009)
📌STICH (2011)
📌FAME-2 (2012)
📌FREEDOM (2012)
📌ORBITA (2018)
📌ISCHEMIA (2020)
@mmamas1973 @mirvatalasnag @ErinMichos @DavidLBrownMD @DLBHATTMD @iamritu
*COURAGE* (n = 2,287)
PCI + OMT vs. OMT in stable CHD
• All had evidence of ischemia
• 31% triple-vessel CHD
• 4.6 years median follow-up
• HR death/MI 1.05 (95% CI: 0.87 to 1.27
PCI + OMT vs. OMT in stable CHD
• All had evidence of ischemia
• 31% triple-vessel CHD
• 4.6 years median follow-up
• HR death/MI 1.05 (95% CI: 0.87 to 1.27
*BARI-2D* (n = 2,368)
CABG or PCI compared to OMT in DM
• 31% TVD ; 5.3 years mean follow-up
• No difference in mortality CABG or PCI compared to OMT
• MI/stroke-free survival PCI vs. OMT 77% vs. 79% (p = 0.15)
• MI/stroke-free survival CABG vs. OMT 70% vs. 78% (p = 0.01)
CABG or PCI compared to OMT in DM
• 31% TVD ; 5.3 years mean follow-up
• No difference in mortality CABG or PCI compared to OMT
• MI/stroke-free survival PCI vs. OMT 77% vs. 79% (p = 0.15)
• MI/stroke-free survival CABG vs. OMT 70% vs. 78% (p = 0.01)
*STICH* (n = 1,212)
CABG + OMT vs. OMT in ICM
• Median EF 28%
• 61% triple-vessel CHD
• 4.8 years median follow-up
• HR death 0.86 (95% CI: 0.72 to 1.04)
CABG + OMT vs. OMT in ICM
• Median EF 28%
• 61% triple-vessel CHD
• 4.8 years median follow-up
• HR death 0.86 (95% CI: 0.72 to 1.04)
*FAME 2 *(n = 888)
FFR guided PCI + OMT vs. OMT alone
• 8% triple-vessel CHD
• 0.6 years median follow-up
• HR death/MI 0.61 (95% CI: 0.28 to 1.35) • Revascularization 0.13 (95% CI: 0.06
to 0.30)
FFR guided PCI + OMT vs. OMT alone
• 8% triple-vessel CHD
• 0.6 years median follow-up
• HR death/MI 0.61 (95% CI: 0.28 to 1.35) • Revascularization 0.13 (95% CI: 0.06
to 0.30)
*FREEDOM* (n = 1,900)
CABG vs PCI in diabetics patients
• 93% triple-vessel CHD
• 3.8 years median follow-up
• MI/stroke-free survival 81% vs. 73%
(p = O.005)
CABG vs PCI in diabetics patients
• 93% triple-vessel CHD
• 3.8 years median follow-up
• MI/stroke-free survival 81% vs. 73%
(p = O.005)
*ORBITA* (n = 200)
PCI vs OMT, double-blinded
• Single-vessel CHD
• Endpoint Δ exercise capacity after 6 weeks
• PCI vs. placebo 16.6 s (–8.9 to 42.0), p = 0.2 • SAQ angina frequency 93.0 vs. 84.6, p = 0.26)
PCI vs OMT, double-blinded
• Single-vessel CHD
• Endpoint Δ exercise capacity after 6 weeks
• PCI vs. placebo 16.6 s (–8.9 to 42.0), p = 0.2 • SAQ angina frequency 93.0 vs. 84.6, p = 0.26)
*ISCHEMIA* (n = 5,179)
PCI or CABG vs. OMT
• >85% moderate or severe ischemia
• 40% triple-vessel CHD
• 3.2 years median follow-up
• CV death or MI 14.2% vs. 16.5% (p = NS)
PCI or CABG vs. OMT
• >85% moderate or severe ischemia
• 40% triple-vessel CHD
• 3.2 years median follow-up
• CV death or MI 14.2% vs. 16.5% (p = NS)
Unroll @threadreaderapp
• • •
Missing some Tweet in this thread? You can try to
force a refresh