
#HFpEF pearl of the day: Bike stress echo is very helpful in the evaluation of HFpEF. In 1 test you can diagnose HFpEF (E/e') and evaluate for CAD (WMA), health of the LA (Δ LA strain), LV contractile reserve (Δ LV strain), dynamic MR, and dynamic LV outflow tract obstruction.
If RV free wall strain goes down with exercise, could be a sign of dynamic pulmonary vasoconstriction during exercise (i.e., ⬆️PVR with exercise) or intrinsic RV dysfunction.
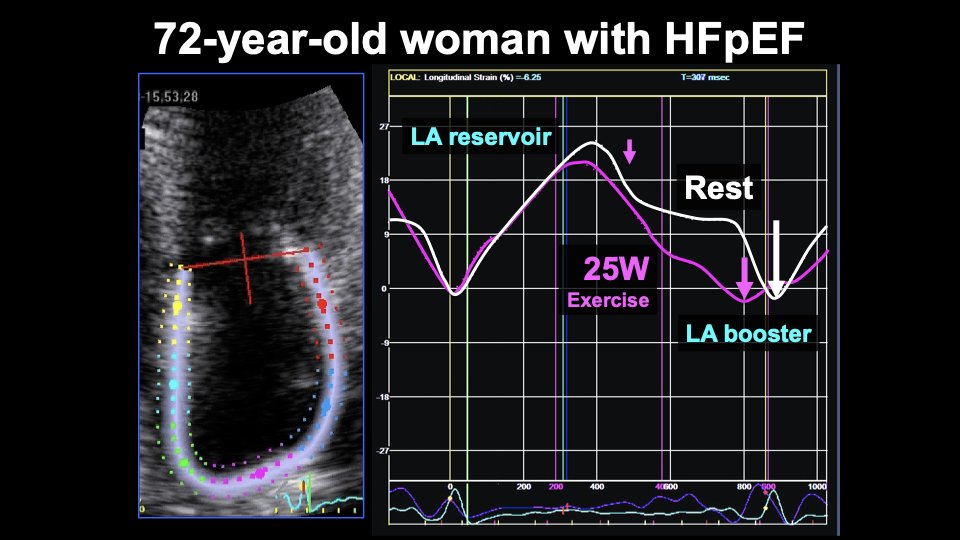
Here is an example. 72 yo woman w/HFpEF. With just 25W exercise, E velocity goes way up. And a' velocity goes down dramatically, indicative of LA contractile dysfunction and ⬆️LV end-diastolic stiffness. 

Here is what happens to LA reservoir strain in the same patient. LA booster strain goes down at 25W of exercise. Conduit strain also goes down. LA reservoir strain = booster + conduit strains therefore also ⬇️. 
Here is another patient with HFpEF who developed significant PAH superimposed (CpcPH) due to systemic sclerosis. Here is baseline echo:
How did this patient's RV systolic function respond to exercise?
Here is the 2D echo (A4c view) at peak stress:
Answer: RV systolic function ⬇️ with exercise. TAPSE and RV s' velocity are unreliable because of tethering effect of the LV, which gets hyperdynamic during exercise, "pulling" the RV longitudinally in the absence of ⬆️RV contractility. Translational motion also problematic. 

Unlike TAPSE and s' velocity, RV free wall strain worsens with exercise, indicating ⬇️RV systolic function. The RV dysfunction is clear on 2D echo w/exercise, so strain not necessarily needed, but helpful to show why it's better than displacement (TAPSE) and velocity (RV s').
RV free wall strain analysis can be helpful for more subtle cases of RV dysfunction is there is a question about whether RV is augmenting appropriately with exercise.
• • •
Missing some Tweet in this thread? You can try to
force a refresh













