#HFpEF pearl of the day: In HFpEF pts with #CardioMEMS devices, bike stress echo + continuous CardioMEMS PA pressure recording can help evaluate underlying pathophysiologic abnormalities.
Case: 71 yo woman w/apical HCM, AF s/p ablation, pacemaker, HTN, CKD with cardiorenal syndrome and PH-HFpEF presents with worsening overload. Echo shows preserved LVEF with apical HCM, PASP 85 mmHg, RAP 15 mmHg, RVOT PW notching consistent with ⬆️PVR.
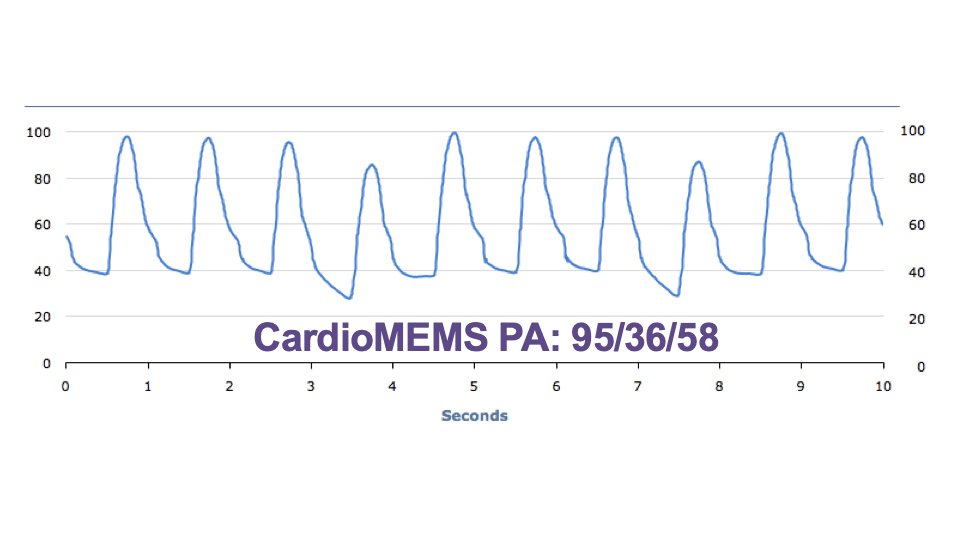
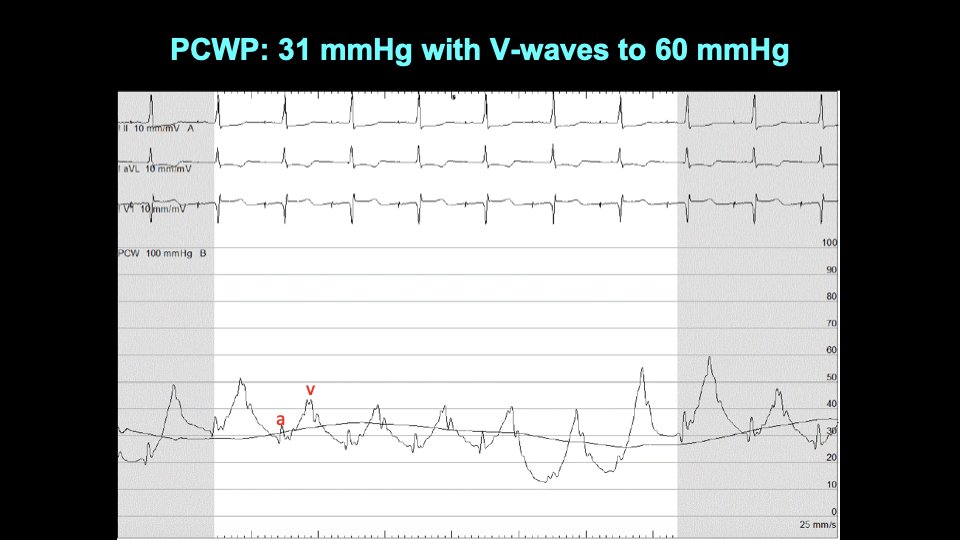
Invasive hemodynamics showed RA pressure 25 mmHg, PA pressure 92/31 (mean 54), PCWP 31 mmHg with V waves up to 60 mmHg. 
She was admitted and underwent IV diuresis. Still very dyspneic. Exercise echo with continuous CardioMEMS pressure recordings done while inpatient. She could only exercise on bike to 15W. ⬆️PA pulse pressure, minimal HR increase. 

Based on the bike stress echo + CardioMEMS it seemed that SV fixed and inadequate HR, so CO was impaired. Blood trapped in the pulmonary circulation w/⬆️ PA pulse pressure and underfilling of LA/LV. Rx'd by ⬆️ basal HR on pacemaker, ⬆️ rate responsiveness: improved symptoms.
Ideally we could’ve done something to ⬆️pulmonary blood flow during exercise so that she could better ⬆️SV but unfortunately no options available. We continued to diurese and Rx her w/hemodynamic-guided mgmt but unfortunately she died ~1 yr later due to progressive renal failure.
• • •
Missing some Tweet in this thread? You can try to
force a refresh