
Something interesting is happening in Europe: Population centers along the same latitude and region are seeing a rise starting exactly around December 3rd.
Any idea why? Anything these countries share aside from latitude? (1/x)



Any idea why? Anything these countries share aside from latitude? (1/x)
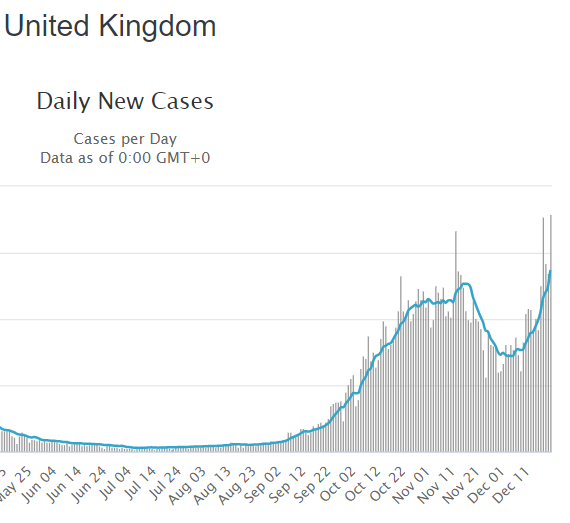

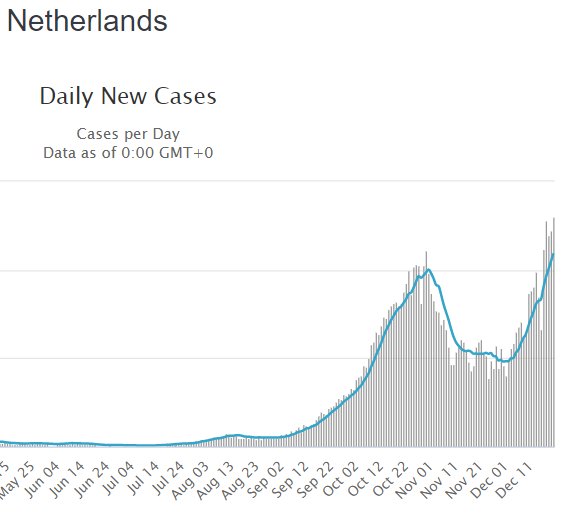

If it is the more infectious variant, as the UK claims, this would mean the variant is already widespread in those other countries as well.
However, I would not expect this to be the case, since the rise would be staggered rather than in concert if that were true. (2/x)
However, I would not expect this to be the case, since the rise would be staggered rather than in concert if that were true. (2/x)
It cannot be human behavior either, as we have seen numerous times by now. The variance in human behavior is too big to cause such orchestrated moves, especially across borders.
Has there been any significant shift in weather in that area around after mid-November? (3/3)
Has there been any significant shift in weather in that area around after mid-November? (3/3)
ADDENDUM: If the rise in London is indeed environmental, it is possible that the new variant is not more infectious, but just happened to be discovered in the wrong place and the wrong time.
I believe the claims 70% more infectious are based on case rates in the area. (4/5)
I believe the claims 70% more infectious are based on case rates in the area. (4/5)
Finally it is possible that both are correct, that this version somehow show a different seasonality pattern, and was already widespread in the region when the weather got right in late November. (5/5)
• • •
Missing some Tweet in this thread? You can try to
force a refresh










