Continuing to hear extremely favorable case reports informally for cyproheptadine even in severe COVID-19.
Publications forthcoming, but worth highlighting now given magnitude of improvement-- extubation within days, reversal of renal failure, stark decline in D-dimer, etc.
Publications forthcoming, but worth highlighting now given magnitude of improvement-- extubation within days, reversal of renal failure, stark decline in D-dimer, etc.
Try it for 48 hours and see. It's just an old allergy medication. Side effects are minor and it is already known to be effective in serotonin syndrome.
It blocks 5-HT2A (platelet activation) and 5-HT2B (cardiac remodeling, pulmonary fibrosis).
It blocks 5-HT2A (platelet activation) and 5-HT2B (cardiac remodeling, pulmonary fibrosis).
https://twitter.com/srrezaie/status/1340778770270216197?s=19
The potential benefit-to-risk ratio is immense.
Cyproheptadine is one of only a handful of drugs for which I have seen decent evidence for large mortality reductions in severe/critical COVID-19.
In combination with standard of care, it appears to be halting and reversing MODS.
Cyproheptadine is one of only a handful of drugs for which I have seen decent evidence for large mortality reductions in severe/critical COVID-19.
In combination with standard of care, it appears to be halting and reversing MODS.
Apparently it has been fairly consistent as well, given fairly soon after intubation or (preferably) before intubation becomes necessary.
Well-established ischemic tissue damage is unlikely to be reversible by any means in the short term, so don't wait.
https://twitter.com/__ice9/status/1342764862074712066?s=19
Well-established ischemic tissue damage is unlikely to be reversible by any means in the short term, so don't wait.
Update--
Still highly favorable practitioner feedback for cyproheptadine in reversing the progressive thrombosis and CNS effects typically observed in severe COVID-19.
Several physicians working from different hospitals able to attest:
Still highly favorable practitioner feedback for cyproheptadine in reversing the progressive thrombosis and CNS effects typically observed in severe COVID-19.
Several physicians working from different hospitals able to attest:
https://twitter.com/farid__jalali/status/1345481621256822784
Note cyproheptadine also succeeded in animal experiments for preventing pulmonary platelet activation and microthrombosis after e.g. endotoxin exposure or physical trauma.
https://twitter.com/__ice9/status/1345198876517670914?s=19
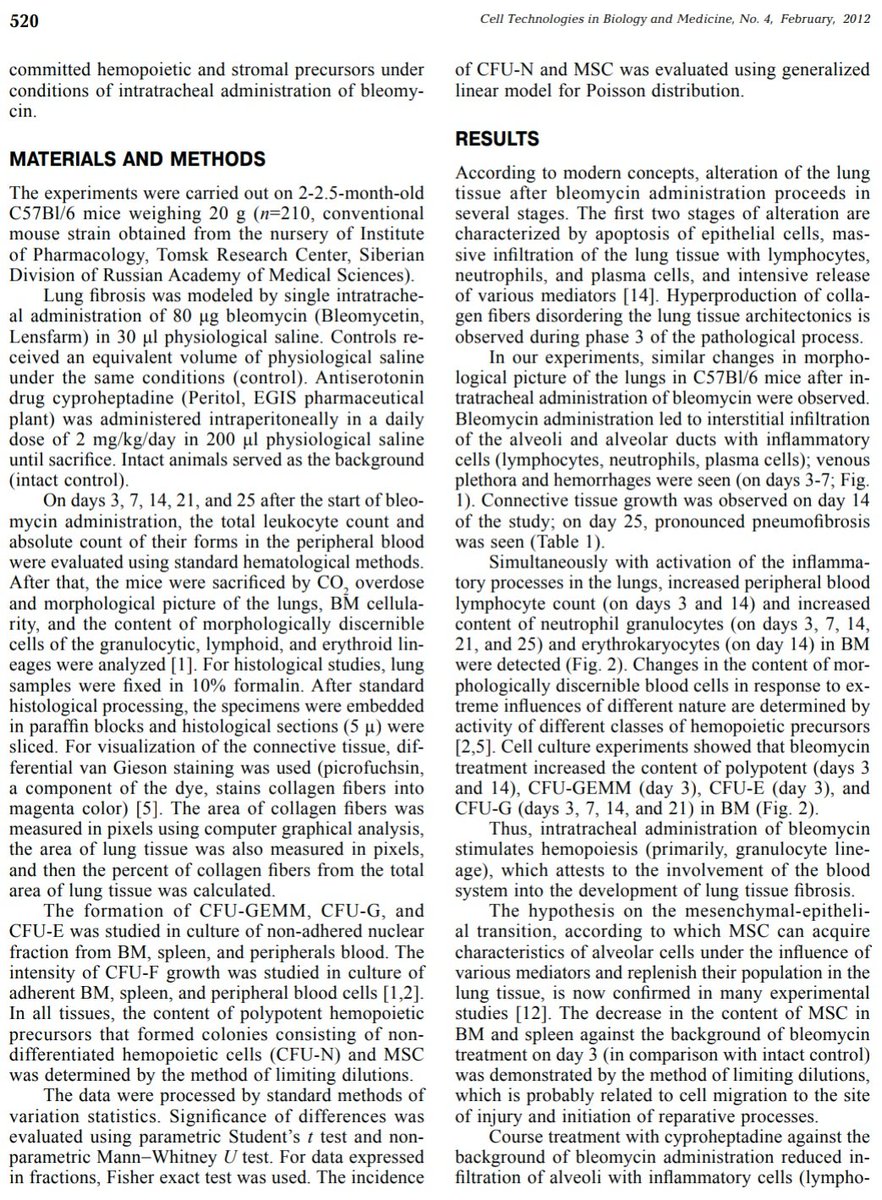
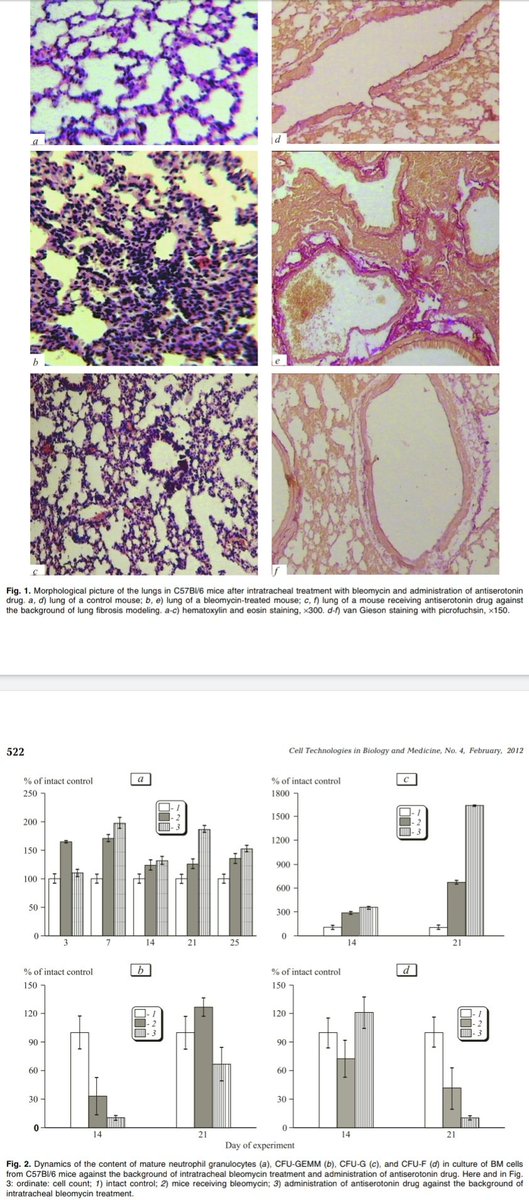
Cyproheptadine also succeeded in preventing pulmonary fibrosis in response to bleomycin exposure, a common animal model thereof:
doi.org/10.1007/s10517…
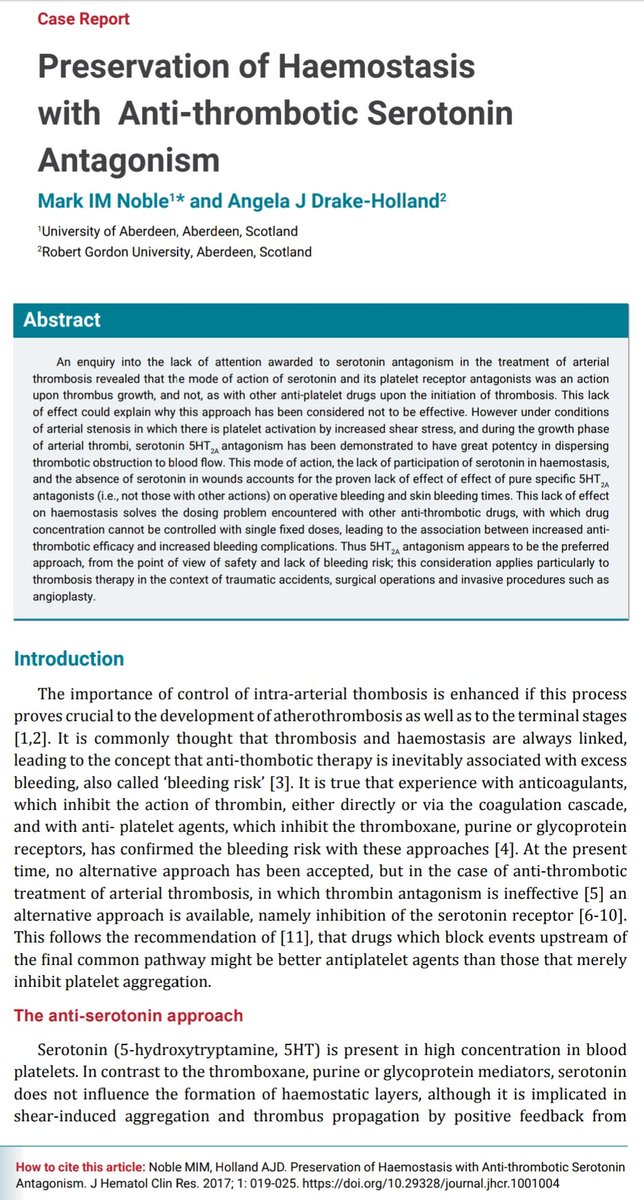
The mechanism is 5-HT2B antagonism (antifibrotic) and 5-HT2A antagonism (antithrombotic/antiplatelet).



doi.org/10.1007/s10517…
The mechanism is 5-HT2B antagonism (antifibrotic) and 5-HT2A antagonism (antithrombotic/antiplatelet).


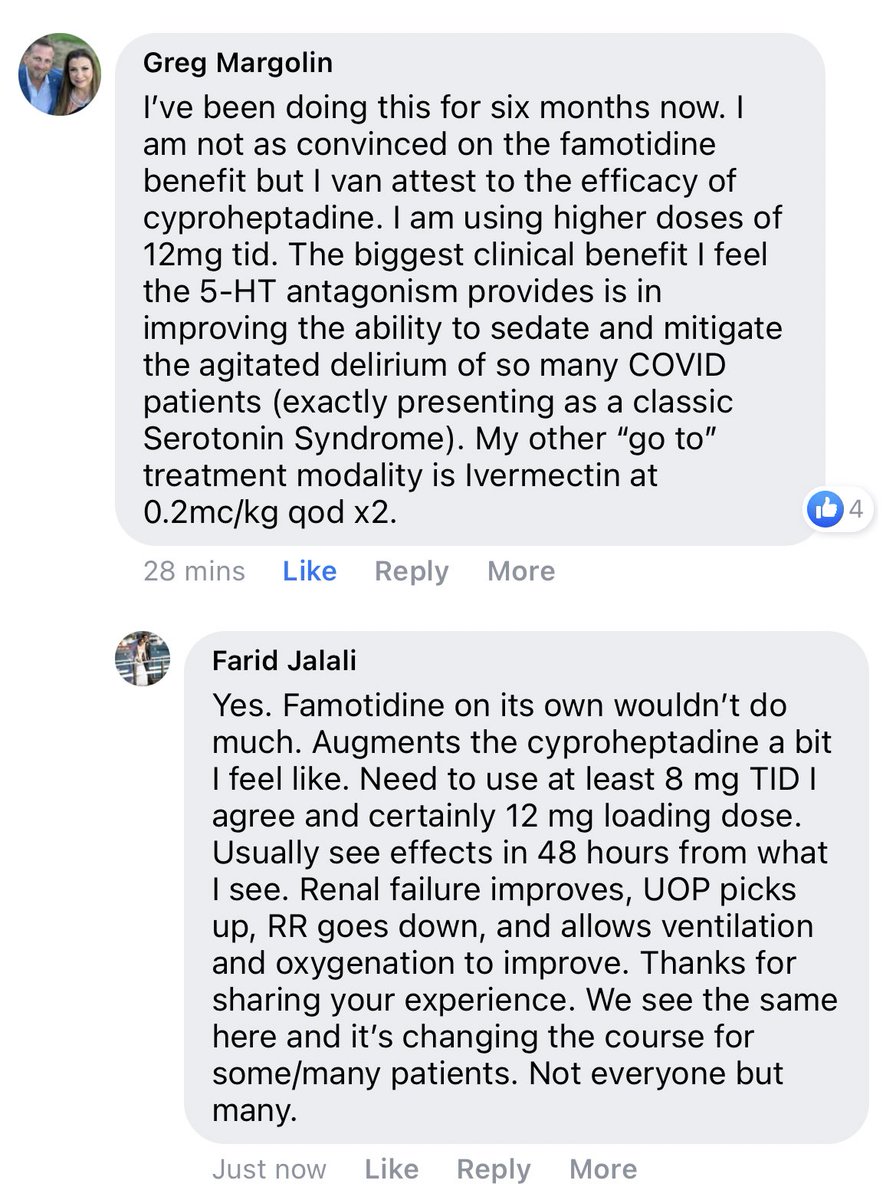
Notes on cyproheptadine use and results in severe COVID-19:
Seems to pair well with famotidine for further effect. Note famotidine has some clinical evidence of efficacy in serotonin syndrome and generally favorable study findings in COVID-19.
https://twitter.com/farid__jalali/status/1345548533533790208?s=19
Seems to pair well with famotidine for further effect. Note famotidine has some clinical evidence of efficacy in serotonin syndrome and generally favorable study findings in COVID-19.
Further favorable practitioner feedback for cyproheptadine in severe COVID-19:
Note famotidine seems mainly useful as an add-on for further effect if cyproheptadine dosing is limited by side effects (as famotidine has ~none). Mechanism is less direct.
https://twitter.com/farid__jalali/status/1345956375935913984?s=19
Note famotidine seems mainly useful as an add-on for further effect if cyproheptadine dosing is limited by side effects (as famotidine has ~none). Mechanism is less direct.
5-HT2A antagonists (e.g. cyproheptadine) have been proposed for arterial thrombotic and vasoconstrictive conditions (like severe COVID-19):
- *no increase in bleeding risk*
- avoids missing the target on clot initiation ('heparin resistance')
@Jopo_dr

- *no increase in bleeding risk*
- avoids missing the target on clot initiation ('heparin resistance')
@Jopo_dr
https://twitter.com/julienpotet/status/1346601014800117764?s=19
• • •
Missing some Tweet in this thread? You can try to
force a refresh