Brief primary care rant.
It's 2021. We have developed an effective vaccine for a novel virus in months and we can land a probe on a comet.
There is major cognitive dissonance with our potential as a society vs. the every day struggle to provide basic care for common conditions
It's 2021. We have developed an effective vaccine for a novel virus in months and we can land a probe on a comet.
There is major cognitive dissonance with our potential as a society vs. the every day struggle to provide basic care for common conditions
Let me give a few examples.
Take hypertension. 1 in 3 Americans has it. It causes millions of years of life lost.
What is the process to diagnose and treat it? I have to beg my patient to buy a $40 cuff at a pharmacy, measure their BP, then call or send the numbers to me.
Take hypertension. 1 in 3 Americans has it. It causes millions of years of life lost.
What is the process to diagnose and treat it? I have to beg my patient to buy a $40 cuff at a pharmacy, measure their BP, then call or send the numbers to me.
Alternative is coming to the office to get their BP measured. What a waste of resources. There are no cheap BP cuffs that can upload measurements to our EHR. Insurance doesn't cover them.
Without data I can't just randomly prescribe and titrate a BP med and hope for the best.
Without data I can't just randomly prescribe and titrate a BP med and hope for the best.
The effectiveness of tele-monitoring for hypertension, along with pharmacists management, is REALLY well proven. You can do it in a barbershop too!
No implementation of this on a broad scale (like a state)
jamanetwork.com/journals/jama/…
nejm.org/doi/pdf/10.105…
No implementation of this on a broad scale (like a state)
jamanetwork.com/journals/jama/…
nejm.org/doi/pdf/10.105…
Here's another example that I struggle with. INSOMNIA.
Again, 1 in 3 people have insomnia. It is a major cause of misery and exacerbating other illness.
There is one treatment that is 100% proven to help and is first-line: cognitive behavioral therapy.
acpjournals.org/doi/10.7326/M1…
Again, 1 in 3 people have insomnia. It is a major cause of misery and exacerbating other illness.
There is one treatment that is 100% proven to help and is first-line: cognitive behavioral therapy.
acpjournals.org/doi/10.7326/M1…
I have not been trained to provide CBT for insomnia. We need to refer to therapists. Not that many take insurance and they are all full. It requires many phone calls to find one.
We have social workers in our clinic who can do it but they're overwhelmed with more dire situations
We have social workers in our clinic who can do it but they're overwhelmed with more dire situations
So we have one of the most common medical conditions in the US that is miserable and I have almost no ability to provide the first line level of care.
Any wonder why drugs like Ambien and Lunesta are so popular?
Any wonder why drugs like Ambien and Lunesta are so popular?
I'll give one more example (I have others) and then I'll stop because I have to do other work.
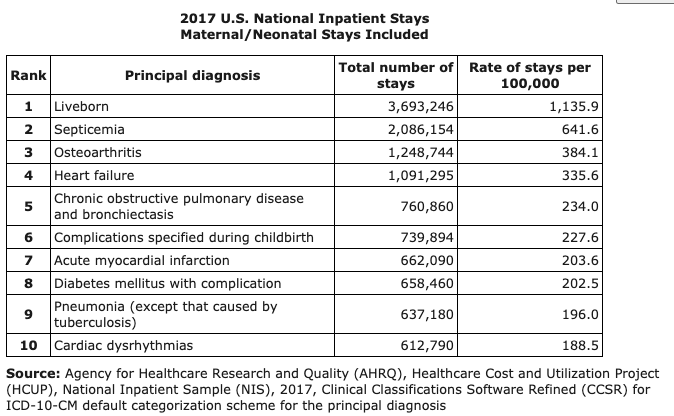
CHRONIC PAIN. Obviously a huge problem. Millions of Americans have difficult-to-treat chronic pain. It's one reason why opioids became so popular.
CHRONIC PAIN. Obviously a huge problem. Millions of Americans have difficult-to-treat chronic pain. It's one reason why opioids became so popular.
PCPs spend a lot of their time managing chronic pain. Usually people don't get into the chronic pain category without having tried and failed multiple medications. Many of the medications we try beyond ibuprofen (eg gabapentin) have poor data backing them.
A 2014 trial established telemedicine protocol with a nurse-pain specialist-PCP team as an effective treatment for chronic pain.
I've never heard of someone implementing this on a larger scale. I could fill up a program just with my tiny panel!!
jamanetwork.com/journals/jama/…
I've never heard of someone implementing this on a larger scale. I could fill up a program just with my tiny panel!!
jamanetwork.com/journals/jama/…
To recap. We have had technology and evidence to provide effective care for hypertension, insomnia and chronic pain for YEARS. YEARS.
But no robust systems to deliver them. ESPECIALLY to BIPOC patients and Medicaid-insured populations.
But no robust systems to deliver them. ESPECIALLY to BIPOC patients and Medicaid-insured populations.
These are just three examples. I didn't even touch mental health, addiction, diabetes, asthma, obesity etc etc.
I know there are people doing good work out there. But my experience just feels too NORMAL given what we can do.
/fin
I know there are people doing good work out there. But my experience just feels too NORMAL given what we can do.
/fin
• • •
Missing some Tweet in this thread? You can try to
force a refresh