From Dan Kahneman: Thinking, Fast and Slow
THE ILLUSION OF VALIDITY
p.221
SPEAKING OF ILLUSORY SKILL
“She is a hedgehog. She has a theory that explains everything, and it gives her the illusion that she understands the world.”
#FreshAirNHS #COVIDisAirborne
THE ILLUSION OF VALIDITY
p.221
SPEAKING OF ILLUSORY SKILL
“She is a hedgehog. She has a theory that explains everything, and it gives her the illusion that she understands the world.”
#FreshAirNHS #COVIDisAirborne

Transmission of SARS-CoV-2: implications for infection prevention precautions
'Scientific Brief' @WHO
who.int/news-room/comm…
'Scientific Brief' @WHO
who.int/news-room/comm…
‘Transmission of SARS-CoV-2 can occur through direct, indirect, or close contact with infected people through infected secretions such as saliva and respiratory secretions or their respiratory droplets, which are expelled when an infected person coughs, sneezes, talks or sings.’ 

'Respiratory droplets are >5-10 μm in diameter whereas droplets <5 μm in diameter are referred to as droplet nuclei or aerosols.' 

Resp droplet transmission can occur when...in close contact (<1 m) with an infected person who has...symptoms (coughing/sneezing) or who is talking/singing; in these circs, respiratory droplets that include virus can reach the mouth, nose/eyes of a...person+..result in infection. 

Comment: Clearly a virion either knows that a cough/sneeze has occurred (to be infectious such ballistic droplets must contain live virus) to jump on/remain on board. Or, if virions are w/o agency, physical laws dictate this behaviour.
Obv madness: I’ll come back to this later.
Obv madness: I’ll come back to this later.

'Indirect contact transmission involving contact of a susceptible host with a contaminated object or surface (fomite transmission) may also be possible (see below).' 

Airborne transmission: the spread of an infectious agent caused by the dissemination of droplet nuclei (aerosols) that remain infectious when suspended in air over long distances+time. Airborne transmission of SARS-CoV-2 can occur during medical procedures that generate aerosols. 
Comment: Clearly, a virion either knows that a medical procedure-related AGP has occurred (to be infectious such aerosols must contain live virus) so it jumps on/remains on board, or if virions are without agency, physical laws completely dictate this behaviour. 

WHO, together with the scientific community, has been actively discussing+evaluating whether SARS-CoV-2 may also spread through aerosols in the absence of aerosol generating procedures, particularly in indoor settings with poor ventilation.
IMO WHO=in a crisis of anchoring bias.
IMO WHO=in a crisis of anchoring bias.

Ref 17: 'The simultaneous detection of viral RNA in small,
airborne-sized (<4.7 mm) and large, droplet-sized
(≥4.7 mm) particles produced on breathing and
coughing by children and adults with symptomatic
respiratory infections was observed in this study.'
(cont'd)...
airborne-sized (<4.7 mm) and large, droplet-sized
(≥4.7 mm) particles produced on breathing and
coughing by children and adults with symptomatic
respiratory infections was observed in this study.'
(cont'd)...
'Viruses detected included hRV, Influenza A virus,
Parainfluenza 1 and 3 viruses and RSV'
(cont'd)
pubmed.ncbi.nlm.nih.gov/23959825/
Parainfluenza 1 and 3 viruses and RSV'
(cont'd)
pubmed.ncbi.nlm.nih.gov/23959825/
'When samples from all viral RNA positive participants were pooled and considered, viral RNA produced on breathing and coughing was detected on all six stages of the Andersen Sampler.'
(cont'd)
(cont'd)
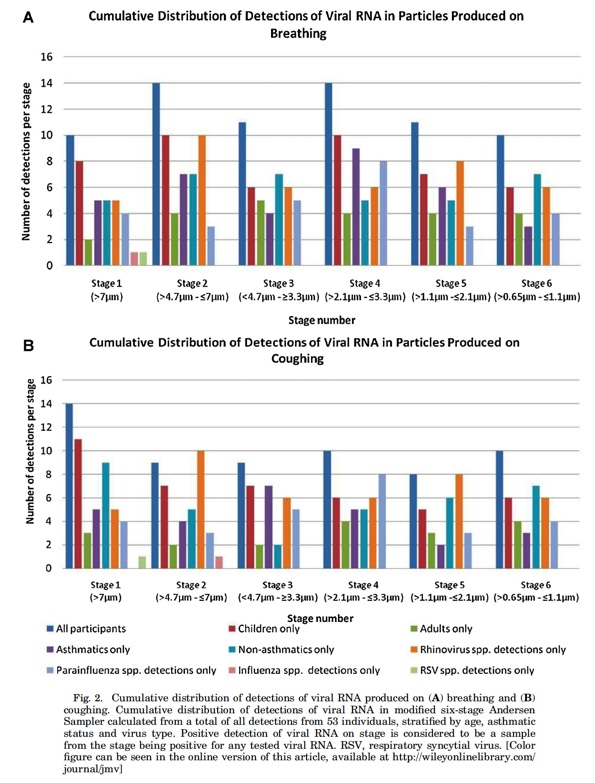
'The observation of similar rates of detection from 10 min of breathing compared with 10 coughs, involving 2–5 min of breathing, may indicate that breathing alone is an unappreciated source of virus...cont'd 

,as breathing occurs continuously whereas the natural frequency of coughing is low for most people.'
(cont'd)
(cont'd)

'The exact determinants of shedding by these routes remains under-explored yet findings from this study suggest that infection control recommendations need to recognise breathing, along with coughing, is a vehicle of aerosolised transmission.' 

Overall findings in this study complements the work of others, where particles sized <5 and ≥5 microns were produced by infected individuals on coughing+breathing,+previous work in which viral RNA+replication competent virus was shown to be expelled during tidal breathing+cough' 

'Ultimately, any definitive model of aerosolised transmission of a respiratory virus will require the demonstration of virus presence, viability and infectivity in expelled aerosolised particles.'
Wise words.
Wise words.
'One experimental study quantified the amount of droplets of various sizes that remain airborne during normal speech.'
doi.org/10.1073/pnas.2…
doi.org/10.1073/pnas.2…
"These observations confirm that there is a substantial probability that normal speaking causes airborne virus transmission in confined environments." 

'However, the authors acknowledge that this relies on the independent action hypothesis, which has not been validated for humans and SARS-CoV-2.'
Comment: IAH 👇, a deal-breaker?
Comment: IAH 👇, a deal-breaker?

'Another recent experimental model found that healthy individuals can produce aerosols through coughing+talking, +another model suggested high variability between individuals in terms of particle emission rates during speech, w high rates correlated w ⬆️amplitude of vocalisation. 

Comment: For coughing/talking-related aerosols to be non-infectious, a virion must *know* that coughing/talking is occurring (i.e. not a ‘medical AGP’, see?!), so it can jump off.
Or, if virions are without agency, physical laws completely dictate this behaviour.
Or, if virions are without agency, physical laws completely dictate this behaviour.

Note: (1) These physical laws must be different from those operating during ‘medical AGPs’, since ‘medical AGPs’ contain infectious virus;
(2) 👇🤷♂️
(2) 👇🤷♂️

Note: (3) Live virus *must* be able to determine droplet particle size, since even though cough/talking-related aerosols are non-infectious, as WHO stated above;
‘*Respiratory DROPLET* transmission can occur when a person is in close contact (<1 m) with an infected person etc..'
‘*Respiratory DROPLET* transmission can occur when a person is in close contact (<1 m) with an infected person etc..'

'Experimental studies have generated aerosols of infectious samples using high-powered jet nebulizers under controlled laboratory conditions. These studies found SARS-CoV-2 virus RNA in air samples within aerosols for up to 3 hours in one study (21) and 16 hours in another..' 

'which also found viable replication-competent virus. These findings were from experimentally induced aerosols that do not reflect normal human cough conditions.' 

Comment: A high powered jet nebuliser sounds like a ‘medical AGP’ and confirms AEROSOLISED SARS-CoV-2 LONG-LASTING VIABILITY.
Unless virions knew they were in a Goldberg drum (not room air) and decided to behave differently – you know, for a laugh. 🤷♂️
nejm.org/doi/full/10.10…
Unless virions knew they were in a Goldberg drum (not room air) and decided to behave differently – you know, for a laugh. 🤷♂️
nejm.org/doi/full/10.10…
'These findings were from experimentally induced aerosols that do not reflect normal human cough conditions.' 

Back to this: For coughing/talking-related aerosols to be *non-infectious*, a virion must KNOW that coughing/talking is occurring (not a ‘medical AGP’), so it can jump off any and all aerosols created. Or, if virions are without agency, physical laws dictate this behaviour. 👇 

Ref 29: 'We investigated the indoor air of the wards of intensive care unit (ICU)-Thorax, Internal, ICU-General and ICU-Heart surgery to detect SARS-CoV-2 at Imam Khomeini Hospital complex as the largest hospital in Iran.'
ncbi.nlm.nih.gov/pmc/articles/P…
ncbi.nlm.nih.gov/pmc/articles/P…
"Forty-four patients confirmed with COVID-19 that were receiving oxygen mask (n=22) and intubation (n=22) treatments.
Given the Table 1, all air samples which were taken 2-5 m from the patients' beds were negative."
"10 air samples were collected"
(cont'd)
Given the Table 1, all air samples which were taken 2-5 m from the patients' beds were negative."
"10 air samples were collected"
(cont'd)

"A possible limitation of our study could be that the volume of air collected for each sample (90 L) influenced the ability to detect a PCR peak. As we had limited access to the wards, the number of collected samples might not be generalized to the all wards of hospital..." 

Comment: You bet!
Half the patients were intubated and half were wearing O2 masks, plus this was a well-ventilated space. 🙂👇
#FreshAirNHS
Half the patients were intubated and half were wearing O2 masks, plus this was a well-ventilated space. 🙂👇
#FreshAirNHS

Ref 30: "Patients with newly diagnosed COVID-19 who were hospitalized singly in AIIRs with separate toilet and shower facilities and who consented to participate in air sample collection were recruited."
ncbi.nlm.nih.gov/pmc/articles/P…
ncbi.nlm.nih.gov/pmc/articles/P…
"To increase the proportion of exhaled air sampled+to reduce the proportion of environmental air from the air conditioning system with 12 air changes/hr, an umbrella fitted with transparent plastic curtain was used as an air shelter to cover patients during sample collection" 

"Briefly, the air sampler was perpendicularly positioned 10cm away from the patient’s chin. At a rate of 50L/min, 1,000L of air was collected by each gelatin filter for 20mins while patients were with or without a surgical mask that complies with the ASTM F2100 level 1 standard." 

"...while patients were WITH OR WITHOUT A SURGICAL MASK that complies with the ASTM F2100 level 1 standard."
Well which was it? With, or without?!
It makes a big difference, right? 🙂
Well which was it? With, or without?!
It makes a big difference, right? 🙂

"SARS-CoV-2 RNA was not detectable by air samplers, which suggests that the airborne route is not the predominant mode of transmission of SARS-CoV-2."
But as ever 👇
WERE THEY INFECTIOUS +/- MASKED-UP, OR NOT?! 🤷♂️
But as ever 👇
WERE THEY INFECTIOUS +/- MASKED-UP, OR NOT?! 🤷♂️

This table is cool though - check out the study at the bottom: notice anything? 🙂
WHO Scientific Brief author(s?) chose not to mention this. Odd, isn't it?
WHO Scientific Brief author(s?) chose not to mention this. Odd, isn't it?

Ref 31: "From Jan 24 to Feb 4, 2020, 3 patients at the dedicated SARS-CoV-2 outbreak center in Singapore in airborne infection isolation rooms (12 air exchanges/hr) with anterooms and bathrooms had surface environmental samples taken at 26 sites."
jamanetwork.com/journals/jama/…
jamanetwork.com/journals/jama/…
"There was extensive environmental contamination by 1 SARS-CoV-2 patient with mild upper respiratory tract involvement." 

"Air sampling was done on 2 days using SKC Universal pumps (with 37-mm filter cassettes+0.3-μm polytetrafluoroethylene filters for 4 hrs at 5 L/min) in the room+anteroom+a Sartorius MD8 microbiological sampler (with gelatin membrane filter for 15mins at 6 m*3/h) outside the room" 

"Air samples were negative despite the extent of environmental contamination. Swabs taken from the air exhaust outlets tested positive, suggesting that small virus-laden droplets may be displaced by airflows and deposited on equipment such as vents."
#FreshAirNHS
#FreshAirNHS

Simple Qs:
1. Was patient C shedding live virus during the sampling period?
2. If so, was it at detectable levels given the sampling methods used?
3. How confident can we be about n=1 patient?
#FreshAirNHS 🙂

1. Was patient C shedding live virus during the sampling period?
2. If so, was it at detectable levels given the sampling methods used?
3. How confident can we be about n=1 patient?
#FreshAirNHS 🙂


'Within samples where SARS-CoV-2 RNA was found, the quantity of RNA detected was in extremely low numbers in large volumes of air and one study that found SARS-CoV-2 RNA in air samples reported inability to identify viable virus.'
ONE study...👇
medrxiv.org/content/10.110…
ONE study...👇
medrxiv.org/content/10.110…
"Samples were obtained in the NQU on days 5-9 of activation, i.e. when mildly ill or asymptomatic individuals infected with SARS-CoV-2 were housed in their rooms for 5-9 days. Samples were obtained in the NBU on day 10, when Patients 1 and 2 had been admitted for 10 days." 

"Air samples that were +ve for viral RNA by RT-PCR were examined for viral propagation in 15 Vero E6 cells. Cytopathic effect was not observed...to date, +immunofluorescence +W blot analysis have not, so far, indicated the presence of viral antigens suggesting viral replication."
Q: If that's the case, why does fig 2 show a day 8 sample with CULTURABLE SARS-CoV-2 FROM HALLWAY AIR (dotted background tricky to see but it's there)? 👇 

Have the 'Transmission of SARS-CoV-2: implications for infection prevention precautions Scientific Brief' authors ACCIDENTALLY INCLUDED a study which PROVES THAT VIABLE SARS-CoV-2 WAS BE ISOLATED FROM HALLWAY AIR, at University of Nebraska Medical Center?
😳
She won't be happy.👇
😳
She won't be happy.👇

'Recent clinical reports of health workers exposed to COVID-19 index cases, not in the presence of AGPs, found no nosocomial transmission when contact+droplet precautions were appropriately used, including the wearing of medical masks as a component of the PPE.'
INCORRECT
INCORRECT

"Between 13 March and 16 March 2020, three HCP from three different hospital units (specialist medical unit, specialist surgical unit, general surgery unit) were found to be positive at SARS-CoV-2 swab after becoming symptomatic for COVID-19"
ncbi.nlm.nih.gov/pmc/articles/P…
ncbi.nlm.nih.gov/pmc/articles/P…
23 Feb-5 Mar, the Monaldi Hospital Italy, adopted a...policy of IP&C, specifically directed to SARS-CoV-2 containment among HCP, as well as patients.
..included standard, contact+droplet precautions,+led to a dramatic ⬆️..use of surgical face masks+hydro-alcoholic gel solutions.
..included standard, contact+droplet precautions,+led to a dramatic ⬆️..use of surgical face masks+hydro-alcoholic gel solutions.

👆🏻 Note FRSM use. 🙂
"The 3 individuals were deemed to have acquired the infection out of hospital. All actively worked during the pre-symptomatic phase for 4 days, and for one shift after becoming symptomatic."
"The 3 individuals were deemed to have acquired the infection out of hospital. All actively worked during the pre-symptomatic phase for 4 days, and for one shift after becoming symptomatic."

"SARS-CoV-2 screening swabs were performed on 17 Mar on all unit HCP (n=107) as well as all current inpatients (n=29). Only one additional nurse, who was working the same shifts as the index Case 1, was found to be positive for SARS-CoV-2 nasal/oropharyngeal swab."
But U said👇🤔
But U said👇🤔

Lost yet?!
That was ref 38, next up 39.
[remember, it helps to repeat 'AEROSOL SARS-CoV-2 TRANSMISSION DOES NOT OCCUR' a few times before reading this kind of article - makes the methods seem far less important, if you know what I mean]
And don't worry, it will be over soon.🤦♂️
That was ref 38, next up 39.
[remember, it helps to repeat 'AEROSOL SARS-CoV-2 TRANSMISSION DOES NOT OCCUR' a few times before reading this kind of article - makes the methods seem far less important, if you know what I mean]
And don't worry, it will be over soon.🤦♂️

PS Sorry about study 38: I have no idea whether this graphic bears any relevance to the true denominator of fellow 'same shift'-working HCPs - a really important aspect, but sadly not clarified during journal peer review. 

Ref 39: "Ward A is a 53-bedded female medical ward for renal patients, with five open cubicles and two three-bedded rooms."
ncbi.nlm.nih.gov/pmc/articles/P…
ncbi.nlm.nih.gov/pmc/articles/P…
"The patient had stayed in an open cubicle (bed 2) of ward A with 10 other patients for 35h (including 18.5h of O2 therapy at 8 L/min) before transferring to AIIR (12AC/hr) for intubation with implementation of contact and airborne precautions." 



"Our index patient with COVID-19, despite a 35-h stay in an open cubicle in a general ward, did not result in any secondary nosocomial infection in any contacts at the time of writing."
But: admitted on day 8 of illness (note infectious viral load characteristics, pic 2)! 🤦♂️

But: admitted on day 8 of illness (note infectious viral load characteristics, pic 2)! 🤦♂️


But WHO Scientific Briefing then states: 'Further studies are needed to determine whether it is possible to detect viable SARS-CoV-2 in air samples from settings where no procedures that generate aerosols are performed and what role aerosols might play in transmission.' 

WHAT ARE THEY ON?
1. THEY HAVE ALREADY ACCIDENTALLY INCLUDED A STUDY DEMONSTRATING CULTURABLE VIRUS FROM HALLWAY AIR SAMPLES, NEBRASKA.
1. THEY HAVE ALREADY ACCIDENTALLY INCLUDED A STUDY DEMONSTRATING CULTURABLE VIRUS FROM HALLWAY AIR SAMPLES, NEBRASKA.

2. Virions can't selectively jump on/off expelled respiratory secretions according to particle size:
(a) they can’t instantaneously 'measure' the particle size as far as I'm aware - happy to see some data on this
(b) they cannot move of their own volition (as above, no data)
(a) they can’t instantaneously 'measure' the particle size as far as I'm aware - happy to see some data on this
(b) they cannot move of their own volition (as above, no data)

3. Virions can't cunningly decide to mislead research teams by choosing to survive for up to 16 hrs in artificially-created aerosols (surely they don’t know they are being created in experimental conditions, not a human host), and yet immediately die in room air?
#FreshAirNHS
#FreshAirNHS

You'll no doubt be delighted to learn that I'm done.
I've wasted enough of my life (and have pushed my wife+kids' patience to the limit, bless them🙏) on this - well, I can't put what I really think here; it wouldn't be professional.
But to this point it's been simply horrific.
I've wasted enough of my life (and have pushed my wife+kids' patience to the limit, bless them🙏) on this - well, I can't put what I really think here; it wouldn't be professional.
But to this point it's been simply horrific.

But lets make our hedgehog proud by quoting WHO authors:
'To date, transmission of SARS-CoV-2 by this type of aerosol route has not been demonstrated; MUCH MORE RESEARCH IS NEEDED GIVEN THE POSSIBLE IMPLICATIONS OF SUCH ROUTE OF TRANSMISSION.'
'To date, transmission of SARS-CoV-2 by this type of aerosol route has not been demonstrated; MUCH MORE RESEARCH IS NEEDED GIVEN THE POSSIBLE IMPLICATIONS OF SUCH ROUTE OF TRANSMISSION.'

How's that for anchoring bias: have you forgotten everything you've just read?
THE ILLUSION OF VALIDITY
“She is a hedgehog. She has a theory to explains everything, and it gives her the illusion that she understands the world.”
THE ILLUSION OF VALIDITY
“She is a hedgehog. She has a theory to explains everything, and it gives her the illusion that she understands the world.”

@BarryHunt008 @jljcolorado @kprather88 @linseymarr @PHE_uk @TheBMA @ahmedaftab68 @AgnesAyton @jeremyphoward @trishgreenhalgh @mmamas1973 @amibanerjee1 @DrAsifQasim @chiafanliang @NHSEngland @doctorsdilemma @doctorshaib @mjb302 @microlabdoc @gaswomancometh @mancunianmedic
@threadreaderapp unroll please. 🙏🙂
• • •
Missing some Tweet in this thread? You can try to
force a refresh