What reaching the peak means for the NHS: We're increasingly confident we have hit *a* peak and hopefully *the* peak of the second wave of coronavirus infections. Hospital admissions lag behind and will carry on rising for another week or so, but this is still a key moment… 1/10 

I have talked before about how and why the healthcare the NHS provides right now is simply not as good as usual. We have protected emergency care but routine care for cancer, cardiac disease and so many other illnesses has been badly affected. Especially surgical treatments. 2/10
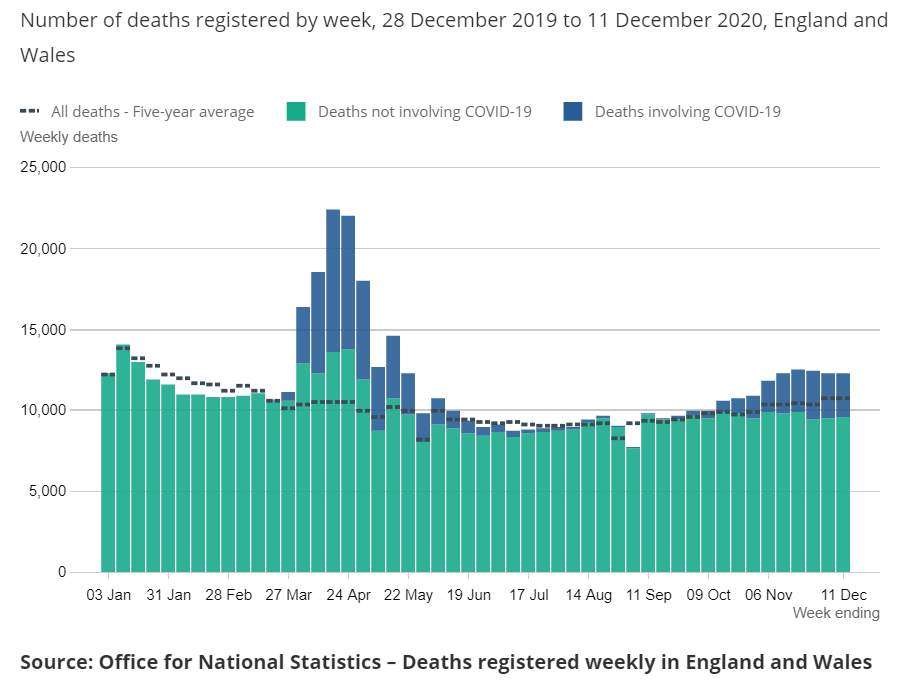
The surge in COVID patient admissions has a huge impact on other parts of the NHS. We see this pattern often in the winter flu season but it is far worse right now. The shortage of normal hospital beds and ICU beds makes in-patient work very difficult. 3/10 

But the key issue is planning. The NHS was not designed to handle huge fluctuations in patient numbers over short periods. We need spare capacity to admit patients into. When the hospital is full, patients must wait to come in, creating serious problems in Emergency Depts. 4/10
Creating spare hospital capacity for a workload we cant predict is difficult. Solutions for small/medium/large patient numbers are all different. If we under-prepare, we cannot admit every COVID patient. If we over-prepare, we ring-fence beds we could use for other patients. 5/10
Once we pass the peak of hospital admissions, we can stop creating spare bed capacity. As time moves on, patients begin to get better and go home. Empty beds become available just through the passage of time. We don’t need to shut down other services to create them. 6/10 

This also means we can begin to return hospital beds to their usual activity. We can stop re-deploying staff to COVID care. We can start thinking about plans for other patient groups waiting for treatment. The same goes for every part of the NHS. 7/10
Emotionally, NHS staff at every level will then know what the system is capable of. The fear of being over-whelmed slowly slips away. Staff become more confident that we can deliver what’s needed, and more focussed as a result. 8/10
The arrival of mass vaccination boosts this confidence even more. Our darkest moment may soon pass. Vaccinated people are much less likely to spread the virus and very unlikely to develop the disease COVID-19. With 3.2 million people vaccinated, we have made a great start. 9/10 

COVID-19 will cast a long shadow. We have huge numbers of patients in hospital. Many will take months to recover. But as each day passes, the task will get easier, and the NHS a little closer to normal. Only when we pass the peak can we hope for a better future. 💙 10/10 

• • •
Missing some Tweet in this thread? You can try to
force a refresh