The legend Ann Thompson, MD, MHCPM, MCCM talking about her career in #PedsICU, including offering herself up as chief at Pittsburgh 6 months out of fellowship. #CCC50 #PedsICU (her caveat was that the division was 2 people with one fellow, 7 nurses, 10 PICU beds) 

Dr. Laura Evans, FCCM asking Dr. Thompson about that transition from fellowship to leadership, the growth of the program. Dr. Thompson relying back on her guidance from Drs Raphaelly and Downes at CHOP who mentored her. "Holding on by your fingertips" at times. #CCC50 #PedsICU
Dr. Thompson points out that having a strong team helped them persevere. (A team of course that she built over the years). #CCC50 #PedsICU
Dr. Thompson: we're used to expecting quick fixes in the ICU, but it doesn't always happen that way. You need to remain persistent, but telling people to be patient for change is not a viable response to those waiting for change. (topic of Women/POC in medicine) #CCC50 #PedsICU
Dr. Thompson: one of the big and important changes in her career is the presence of families in the ICU. They were initially begrudgingly invited in, even in peds, but eventually, and somewhat suddenly people saw the benefit. #CCC50 #PedsICU
Dr. Thompson now relaying a story of the talk I first saw her give In Hot Springs, Arkansas! It was so awesome. The topic was "What happens to Peds Intensivists 15 years after fellowship?" She started in a shawl and wig, and finished rollerblading off the stage. #CCC50 #PedsICU
Question from @MusaNdidi about opportunities for physicians in color in CCM to address the under-representation: Better communication of experiences, educating colleagues about biases, and awareness. We desperately need a better pipeline into health professions #CCC50 #PedsICU
allowing a platform to share the experiences our colleagues have had in their careers, so we are better aware. #CCC50 #PedsICU
Thompson: school is working on the students. But points out that the faculty are the ones who are most likely to need the education regarding biases. #CCC50 #PedsICU
Thompson: realizes her own lack of awareness at times, sharing an incident where she was curious about a colleague's nationality, but her line of questioning ended up being insensitive, and she found herself needing to give a deserved apology. #CCC50 #PedsICU
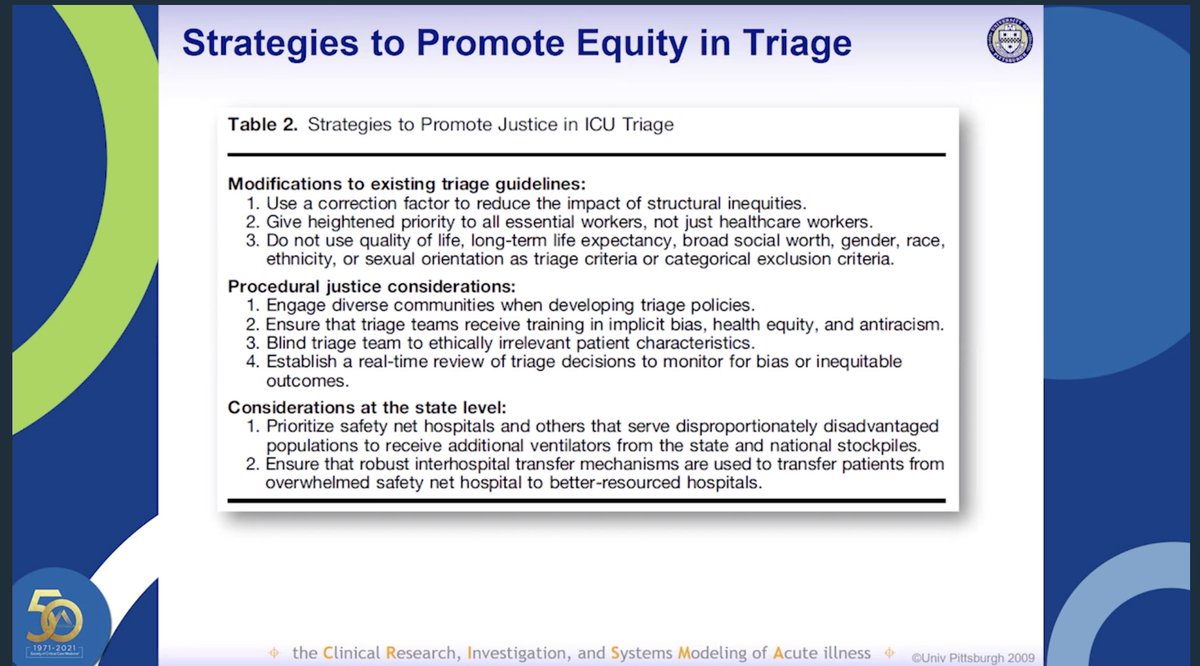
Thompson: would like to see sessions on Equity QI in the ICU, what we are doing to improve the equity among our patients in the ICU #CCC50 #PedsICU
Thompson: most challenging part of SCCM president...still experiencing saying something in a meeting and having it ignored, but a male colleague saying the same thing later with a better response. (But she felt comfortable at that point calling It out) #CCC50 #PedsICU
Thompson: book recommendation Thinking Fast, and slow #CCC50 #PedsICU applies well to ICU powells.com/book/thinking-…
• • •
Missing some Tweet in this thread? You can try to
force a refresh