🚨 Interesting non Covid case yesterday! 🤓
25 YO male, pauci-immune GN previously treated w/ ciclosporine + ⬆️ dose steroids. Arrives @ triage w/ SOB, fever, AKI KDIGO 2 & this CT scan:
25 YO male, pauci-immune GN previously treated w/ ciclosporine + ⬆️ dose steroids. Arrives @ triage w/ SOB, fever, AKI KDIGO 2 & this CT scan:
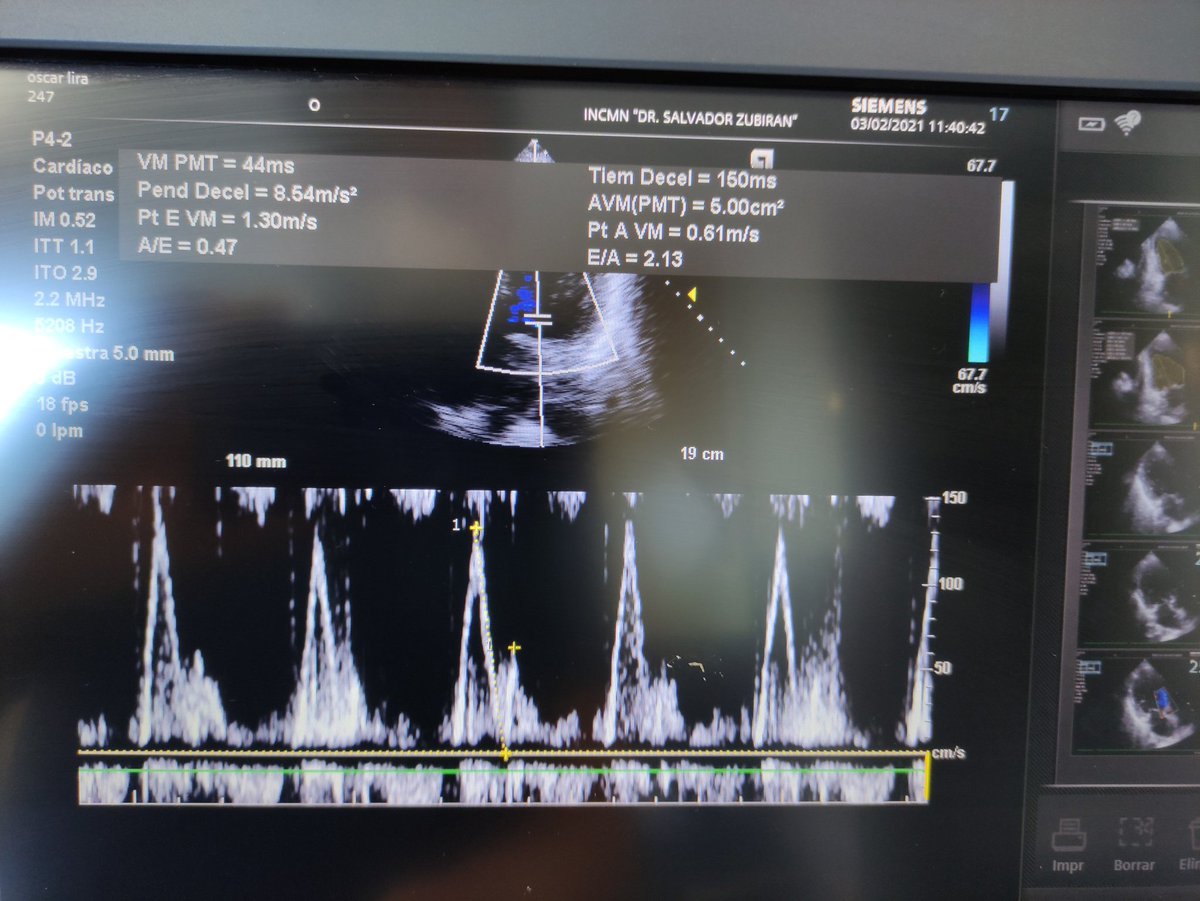
dDx was DAH vs acute pulmonary edema (❤️renal syndrome type 1 vs 3). NIV was started w/ excellent response, FiO2 ⬇️ from 100% to 40%. Met the pt yesterday, already on abs & diuretics, but still ⬇️ UO. Neph wanted to star RRT. Pt had Gallavardin phenomenon on 🩺 + 🥶. #POCUSFirst
PLAx
Ap4Ch
Ap5Ch doppler
3Ch
3Ch doppler
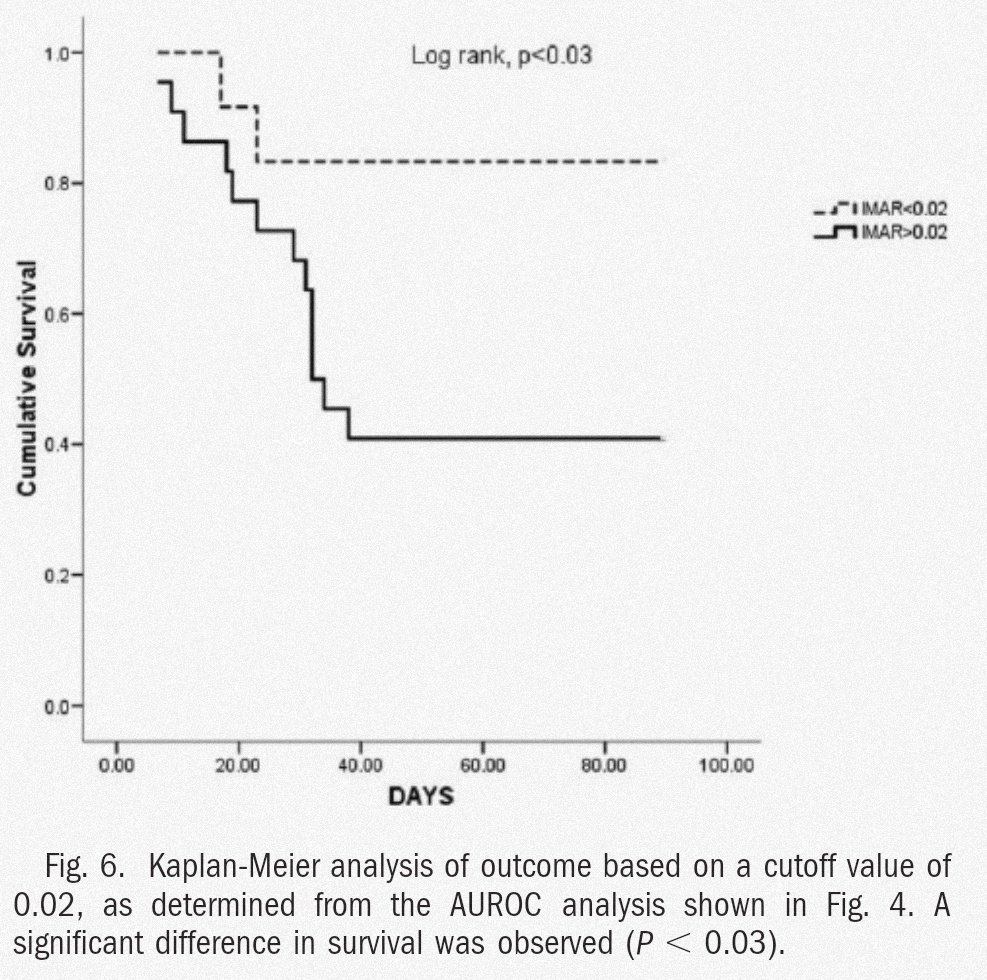
Based on ☝🏽 findings, it seemed to me it was more of a ⬇️ output state rather than 💧 overload, so added vanc, started dobutamine @ 2.5 mcg/kg/min and low dose NE. Pts UO went from 200 mL in 8 hrs ➡️ 1L in the 8 hrs following change in therapy, ScvO2 went 54%➡️ 68%, CRT 5s ➡️ 1s
What do you guys think? Did your initial Dx change with these images?
Would love to read your comments/ suggestions! @BrooksWalsh @EM_RESUS @MaruanCarlos @ogi_gajic @msiuba @ThinkingCC @iceman_ex @PulmCrit @Thind888 @curromir @load_dependent @sargsyanz @AvrahamCooperMD @medpedshosp @ArgaizR @IM_Crit_ @COREIMpodcast @Glenn04716918
Ok first of all sorry guys, I was post call and think the presentation was sllugish 😂, here's my rationale: pt comes initially with what is thought acute pulmonary edema 2/2 fluid overload b/o renal deterioration from preexisting glomerulonephritis➡️
Gets better on NIV but diuretics aren't doing the trick (still low UO), neph still thinks the pt is fluid ⬆️ and benefits from dyalisis ➡️ I see pt, low MAP w/low dyastolic, cold pt, ⬇️CRT, heart murmur stronger on Ao valve ➡️
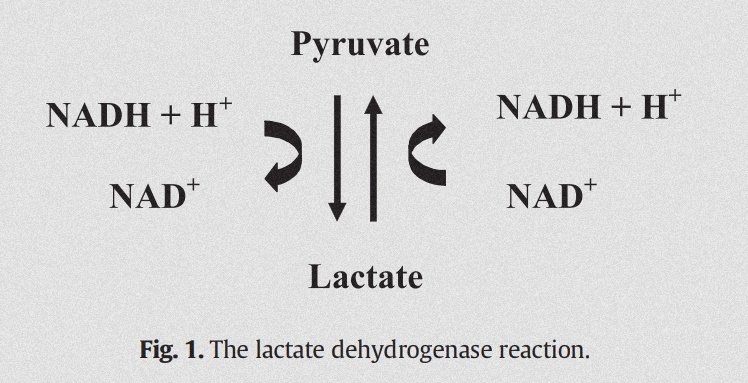
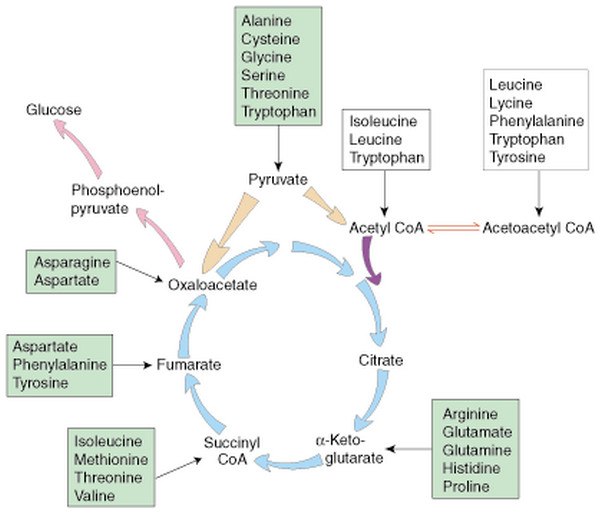
IVC is small & right heart is normal, so I think no fluid overload, LVOT VTI normal but LVEF persistently measured around 30%, see something weird on Ao valve w/ slight reflux and remember pt has been febrile: think of IE w/ LVEF b/o Ao regurgitation and pb a septic component too
Start vanc b/o dx suspicion and inotropic to try to ⬆️ LVEF and MAP to improve renal perfusion➡️ pt starts forming urine, CRT 1 sec, ScvO2 goes from 54% to 68%, new LVEF (not shown) measured at around 65%, me feeling happy
• • •
Missing some Tweet in this thread? You can try to
force a refresh