ED 3 AM: 🚨 ambulance rushes in, pt in his 40's unconscious, BP 50/20, HR 140. Reanimation is started and arterial gases are ordered: lactate 10! Two hours later, pt conscious, MAP >65, HR 100, new arterial gases are ordered: lactate 9.
Was reanimation unsuccesful?
Poll & 🧵:
Was reanimation unsuccesful?
Poll & 🧵:
First, let's go #BackToBasics w/ lactate:
💉 2 enantiomers: L & D
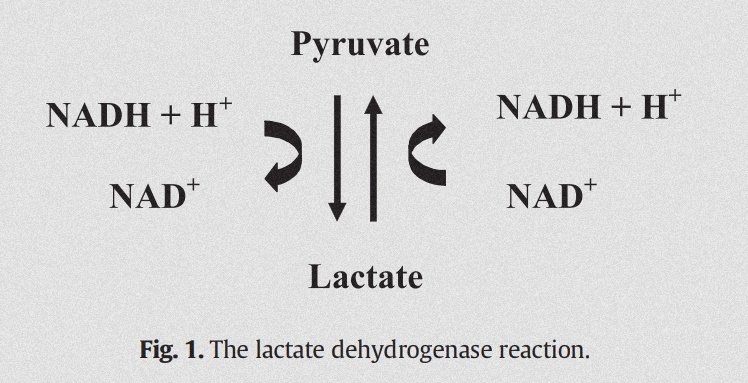
💉 Formed from pyruvate by LDH (usual ratio 10:1)
💉 PKa 3.8 (lactate predominant over lactic acid)
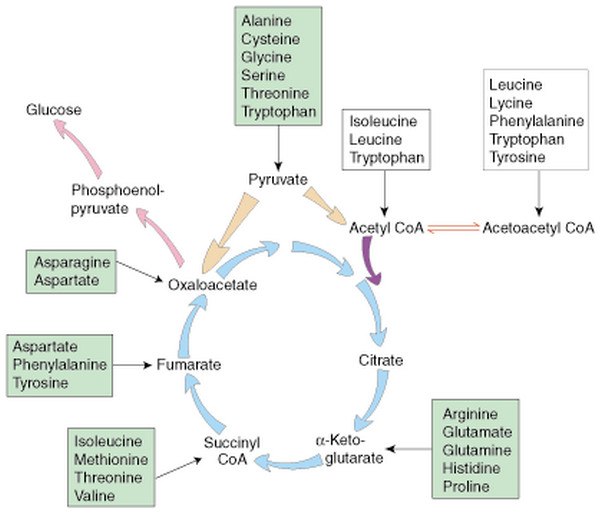
💉 Can be used for ATP formation or gluconeogenesis (lac➡️pyruvate➡️A-CoA or lac➡️pyruvate➡️oxaloacetate)

💉 2 enantiomers: L & D
💉 Formed from pyruvate by LDH (usual ratio 10:1)
💉 PKa 3.8 (lactate predominant over lactic acid)
💉 Can be used for ATP formation or gluconeogenesis (lac➡️pyruvate➡️A-CoA or lac➡️pyruvate➡️oxaloacetate)
We tipically associate 💉 w/⬇️ O2, but what else can ⬆️ 💉? Many things!:
💉 Sepsis
💉 Cyanide
💉 CO
💉 💊: MET, linezolid, paracetamol, NRTI's
💉 ⬇️ thiamine
💉 🍺: Propylene glycol, methanol, ethanol
💉 Malignancy
💉 Cirrhosis
💉 Severe asthma
💉 ❤️ surgery
💉 Sepsis
💉 Cyanide
💉 CO
💉 💊: MET, linezolid, paracetamol, NRTI's
💉 ⬇️ thiamine
💉 🍺: Propylene glycol, methanol, ethanol
💉 Malignancy
💉 Cirrhosis
💉 Severe asthma
💉 ❤️ surgery
So lactate ≠ ⬇️ O2: so far, so good. But it surely does in shock states, right?
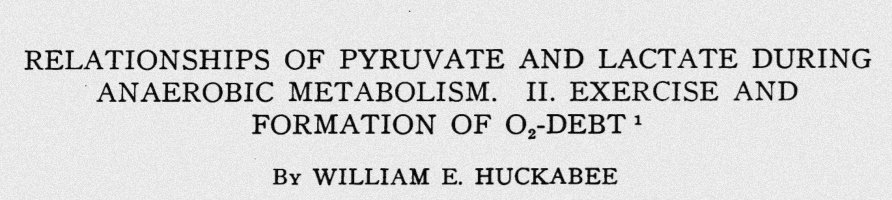
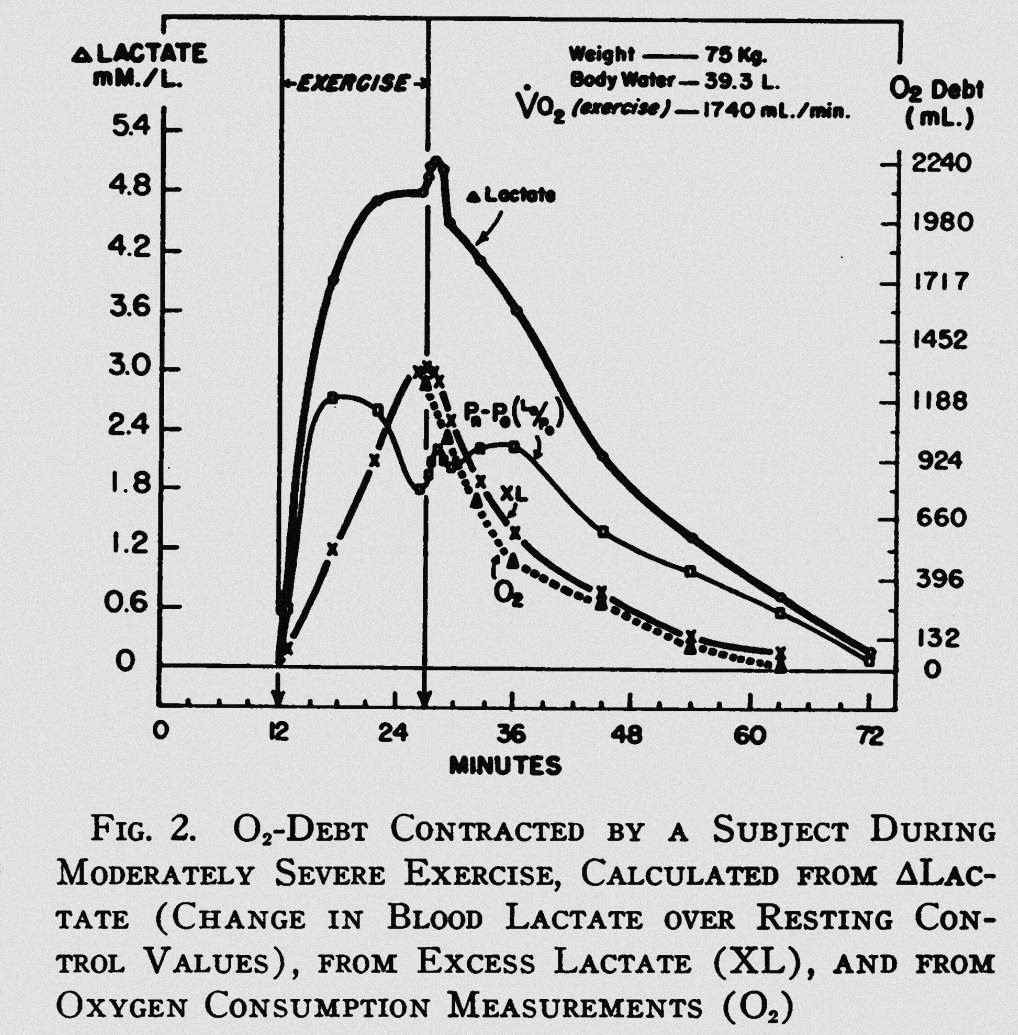
Back in 1958, Huckabee observed the relationship between "oxygen debt" and "excess lactate", plotting almost superposable curves from the relationship of them.
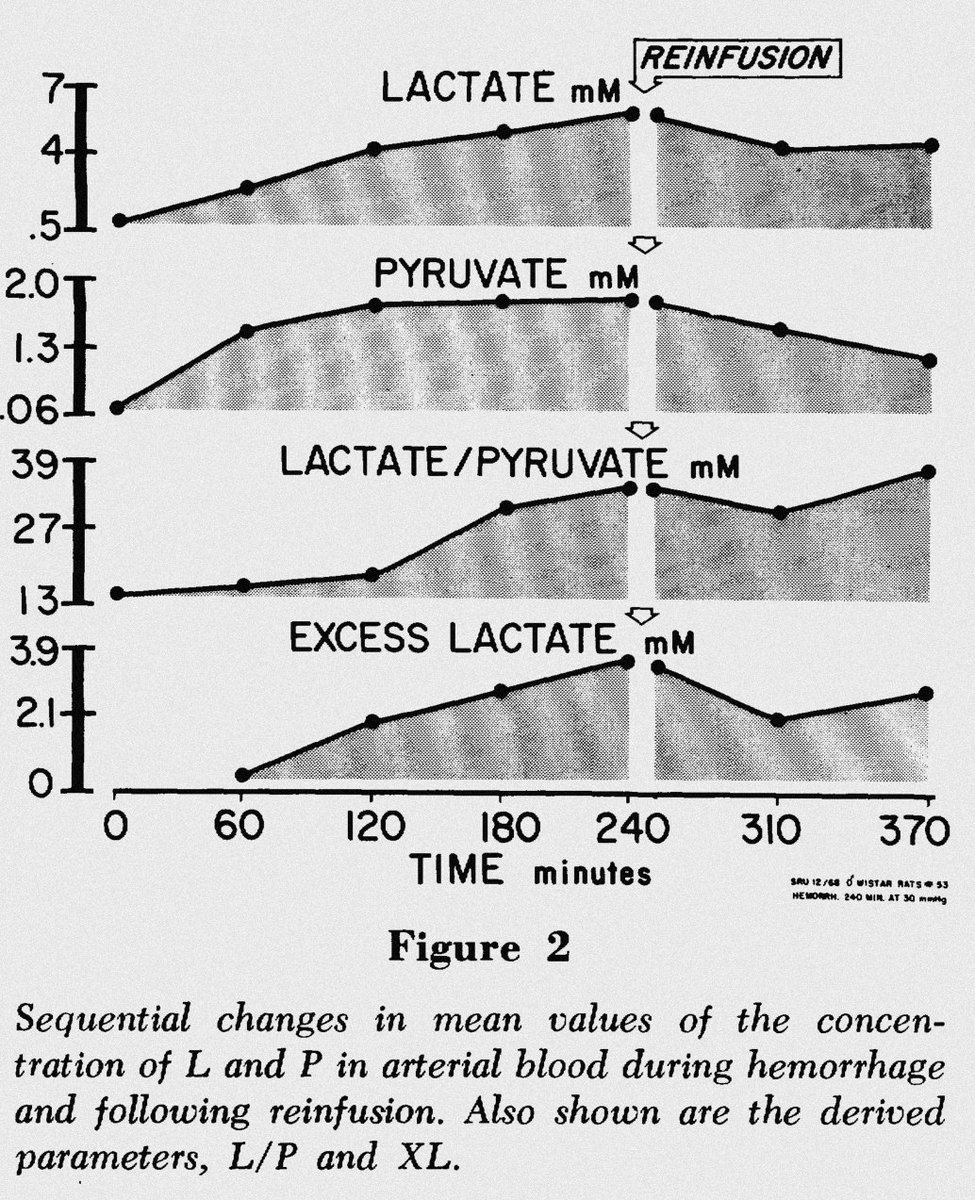
Then in 1970, Weil further supported this data w/ a 🐀 hemorrhagic shock model in which 💉 again correlated w/ O2 debt



Then in 1970, Weil further supported this data w/ a 🐀 hemorrhagic shock model in which 💉 again correlated w/ O2 debt
Furthermore, the classic division of type A and B 💉, assumes the former is always 2/2 a DO2/VO2 mismatch ➡️ anaerobic glycolysis, and is the cause of ⬆️💉 in the critically ill pt, whilst the latter represents ⬆️💉 w/o anaerobic glycolysis.
But... Is it always true? 🤔
But... Is it always true? 🤔
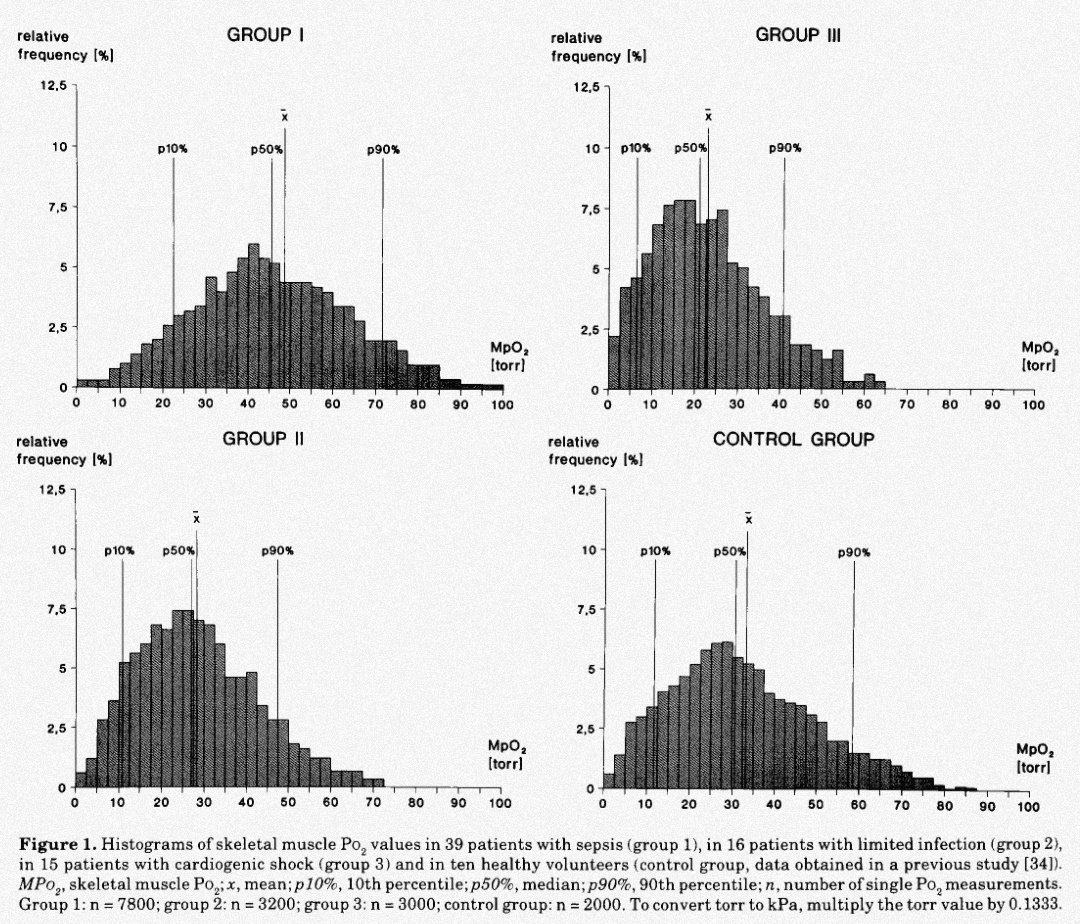
Not quite. In 1994, Boekstegers et al. measured skeletal muscle pO2 in three groups:
🦠 Sepsis
🦠 Limited infection
❤️ shock
They found pO2 to be ⬆️ in sepsis compared to the other 2 groups, being ⬆️ in more severe sepsis states!
But what about cellular dysoxia, you might ask?

🦠 Sepsis
🦠 Limited infection
❤️ shock
They found pO2 to be ⬆️ in sepsis compared to the other 2 groups, being ⬆️ in more severe sepsis states!
But what about cellular dysoxia, you might ask?
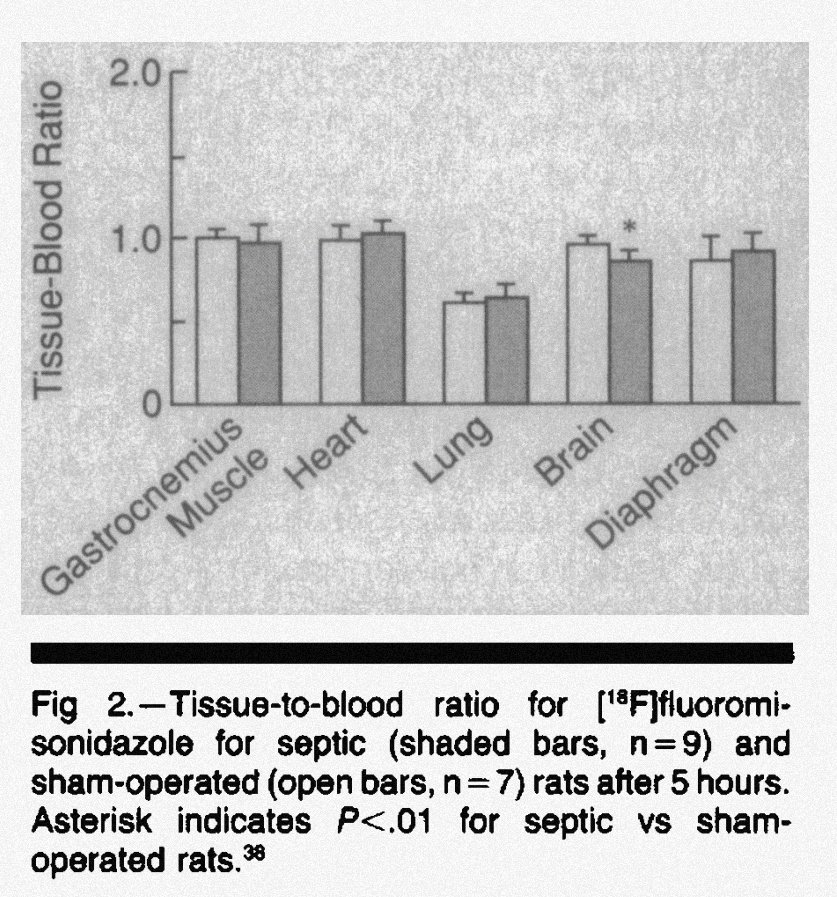
Well, some people asked themselves that same question before! In 1992, Hotchkiss et al. injected fluoromisonidazole (binds covalently to cells in inv proportion to cell O2 tension) in septic and sham operated 🐀, finding no diff in it's concentration in various tissues (but 🧠) 

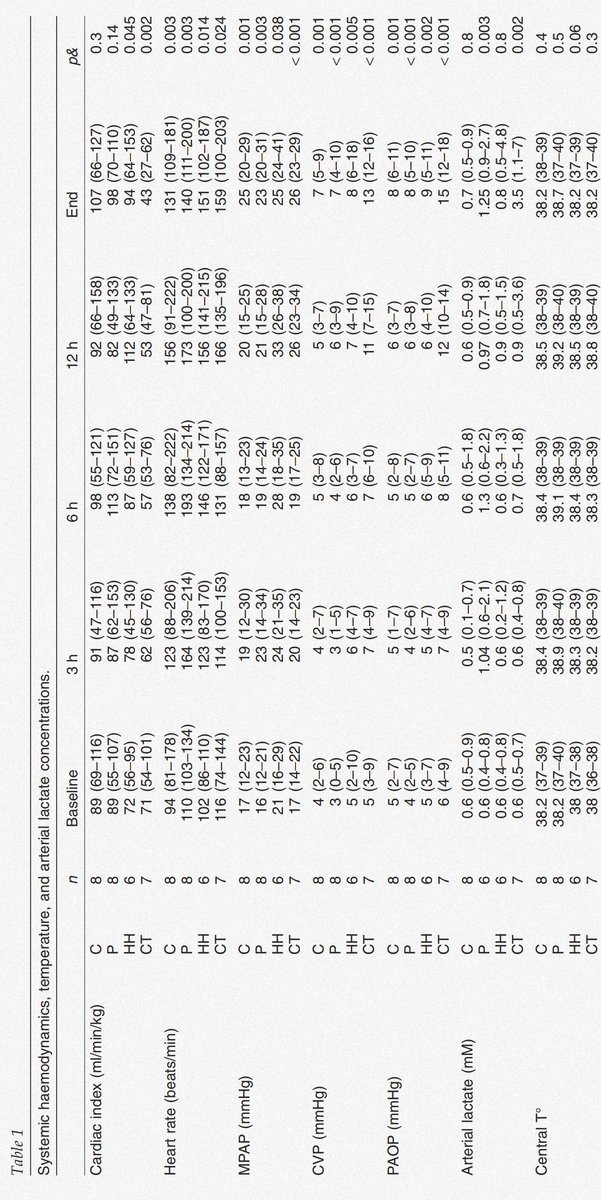
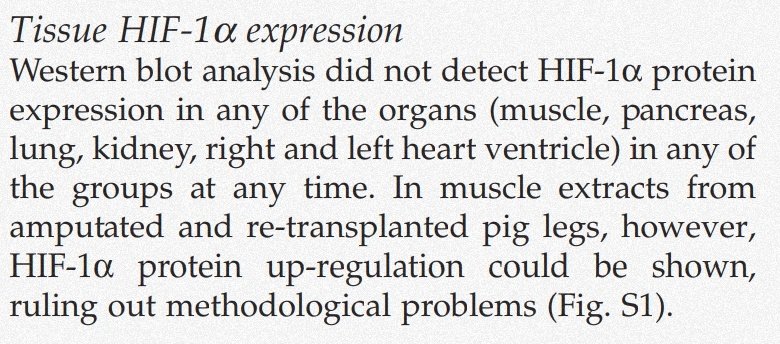
Furthermore, in 2012 Regueira et al. used 32 🐷 w/ 💩 peritonitis, ❤️ tamponade or hypoxemic hypoxia, demonstrating no increase in HIF-1α (hypoxia-inducible factor 1 alpha) in septic animals despite a 2x ⬆️ in lactate levels! 


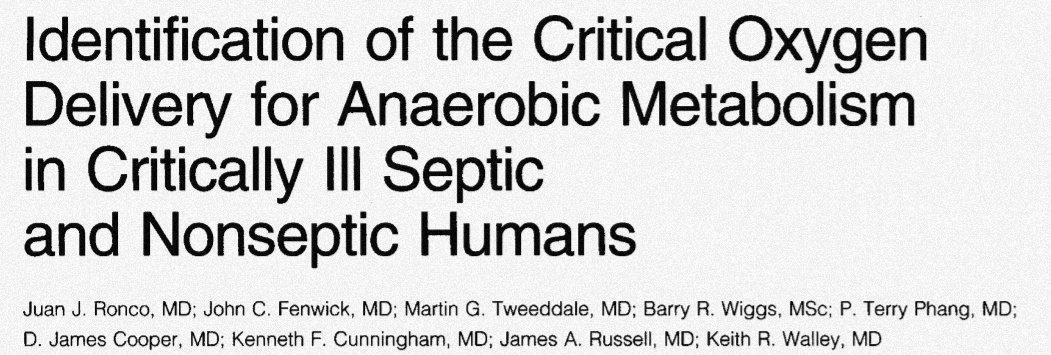
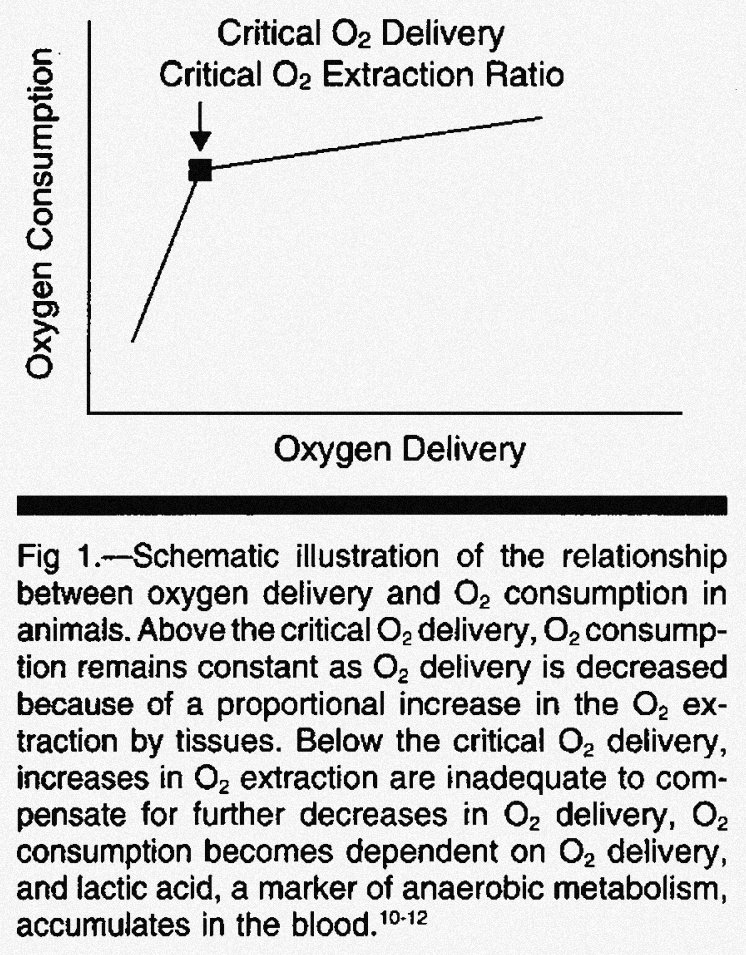
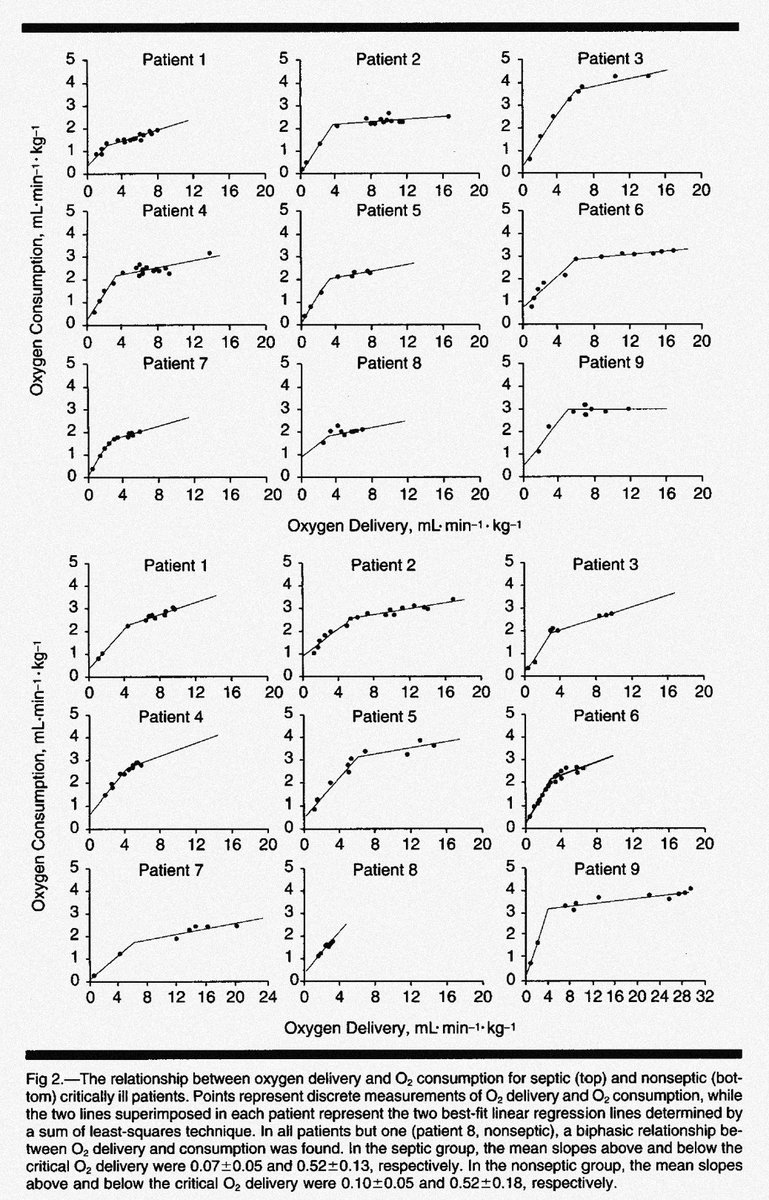
Another theory in sepsis states for ⬆️💉 is a DO2/VO2 mismatch; this was studied in 9 septic critically ill pts by Ronco et al. back in 1993 and... found sepsis didn't modify critical O2 delivery threshold for anaerobic metabolism compared to controls! 


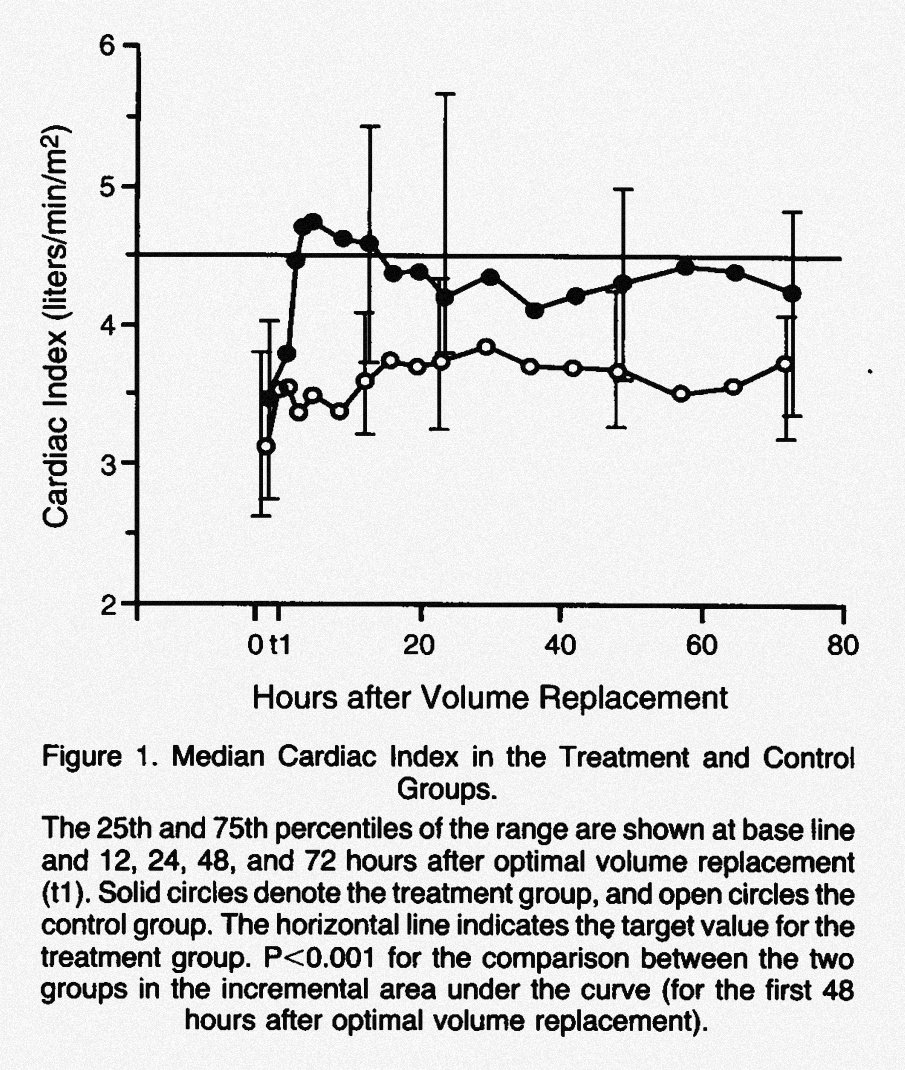
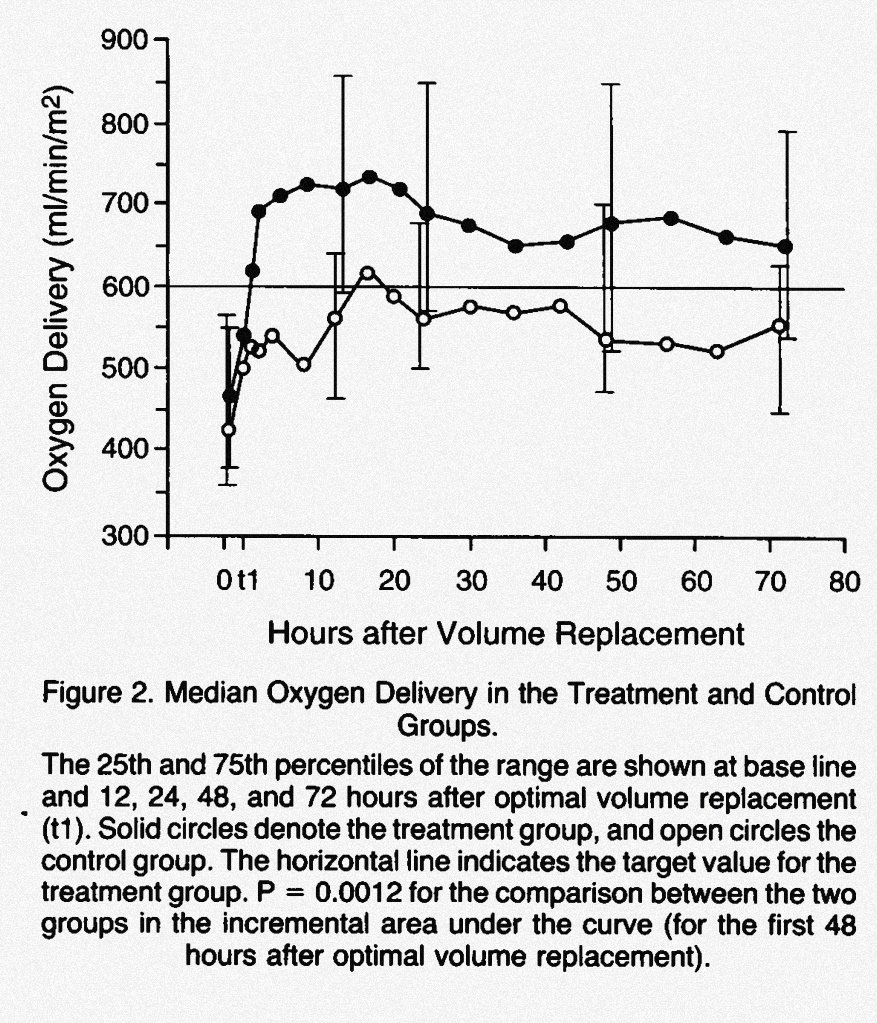
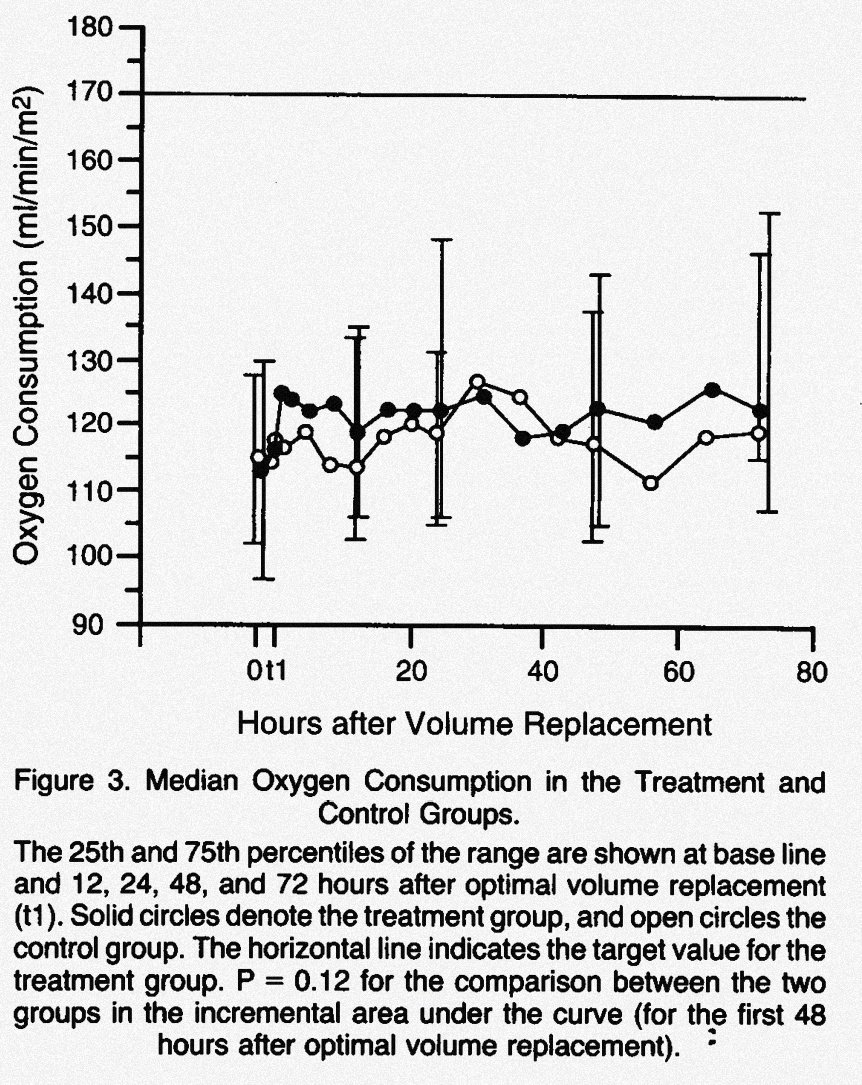
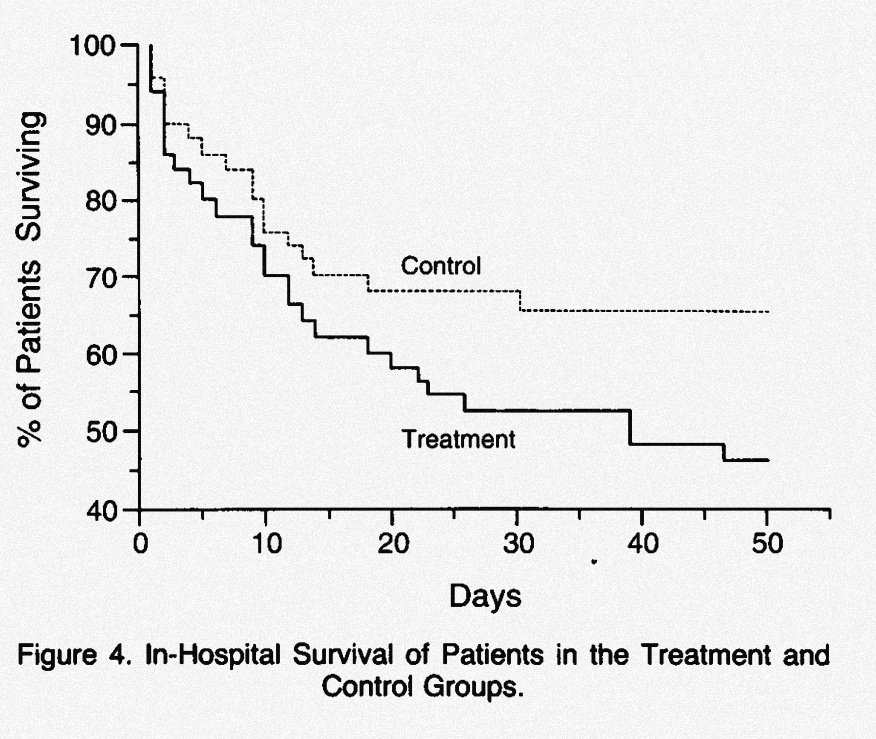
Furthermore, in 1994 Hayes et al. tried to achieve the following goals w/volume ⬆️:
❤️ CI > 4.5 L/min/m²
❤️ DO2 >600 mL/min/m²
❤️ VO2 > 170 mL/min/m²
If 🚫 achieved, ➡️ randomized to dobutamine vs standard care. The results:
🔵 = MAP & VO2
🔴 ⬆️☠️ in intervention group!



❤️ CI > 4.5 L/min/m²
❤️ DO2 >600 mL/min/m²
❤️ VO2 > 170 mL/min/m²
If 🚫 achieved, ➡️ randomized to dobutamine vs standard care. The results:
🔵 = MAP & VO2
🔴 ⬆️☠️ in intervention group!
Ok, so where does lactate come from in sepsis?!
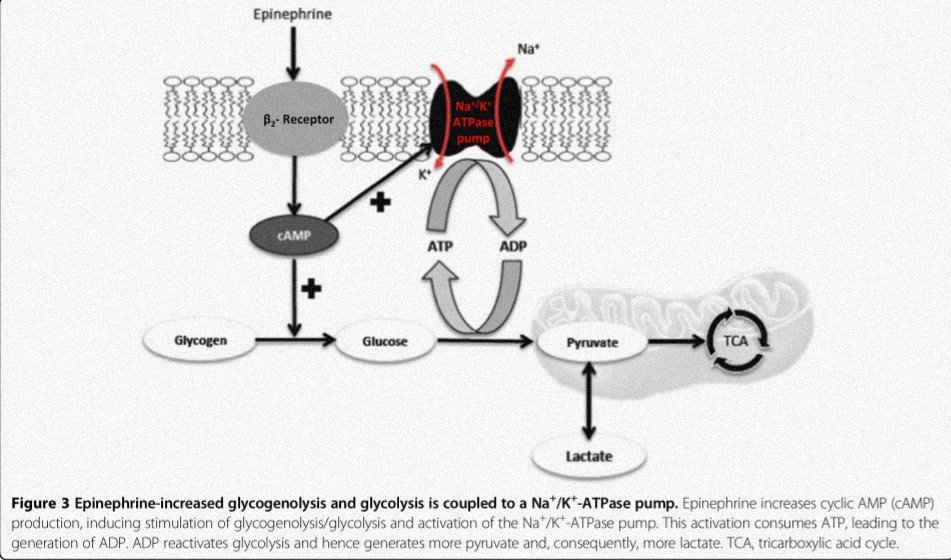
Well, here's an alt theory! ⬆️ aerobic glycolisis 2/2 ⬆️adrenergic state:
⬆️ CHO metabolism exceeds mitochondria oxidative capacity ➡️ piruvate produced at ⬆️ rates than PDH can convert to ACoA ➡️ piruvate ➡️ lac by mass effect
Well, here's an alt theory! ⬆️ aerobic glycolisis 2/2 ⬆️adrenergic state:
⬆️ CHO metabolism exceeds mitochondria oxidative capacity ➡️ piruvate produced at ⬆️ rates than PDH can convert to ACoA ➡️ piruvate ➡️ lac by mass effect
What supports this theory?:
💉 Septic pts whole 🩸 mRNA analyisis: ⬆️ GLUT-1, LDH, PKM-2, hexokinase-3, MCT-4
💉 Isotope dilution methods: ⬆️ Lac and glc turnover in 🦠
💉 Lac kinetics: normal removal (pb source: ⬆️ production)
💉 ⬆️ Cathecolamines ➡️ β2 rec➡️ ⬆️ Na/K ATPase act
💉 Septic pts whole 🩸 mRNA analyisis: ⬆️ GLUT-1, LDH, PKM-2, hexokinase-3, MCT-4
💉 Isotope dilution methods: ⬆️ Lac and glc turnover in 🦠
💉 Lac kinetics: normal removal (pb source: ⬆️ production)
💉 ⬆️ Cathecolamines ➡️ β2 rec➡️ ⬆️ Na/K ATPase act
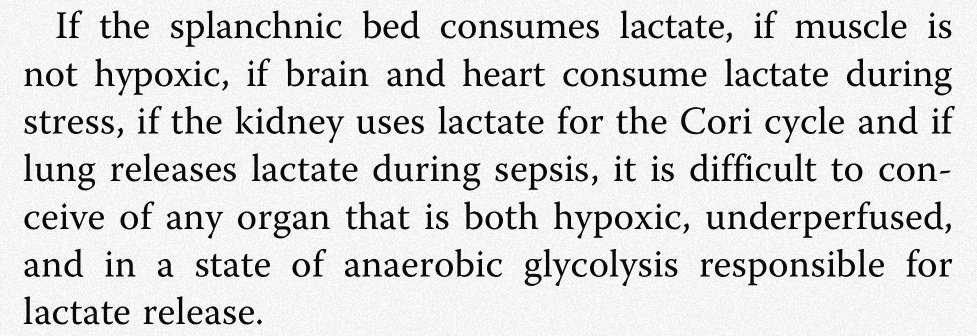
But do all organs produce lactate during sepsis? No! Some ⬆️ production, but some ⬆️ uptake!
The organs that mainly ⬆️ lactate in exp models are 1️⃣ the lung and 2️⃣ the muscle. And uptakers?:
💉 Gut
💉 🧠
💉 ❤️
💉 Kidney
So, as García-Álvarez et al. fairly put it:
The organs that mainly ⬆️ lactate in exp models are 1️⃣ the lung and 2️⃣ the muscle. And uptakers?:
💉 Gut
💉 🧠
💉 ❤️
💉 Kidney
So, as García-Álvarez et al. fairly put it:
Furthermore, studies using labeled exogenous lactate in septic px have shown that 50-60% goes to oxidation by cells, whilst the remaining 30-40% is used as substrate for glycogen synthesis, acting under stress as both:
⛽ Alt fuel to glucose
⛽ A source for glucose itself
⛽ Alt fuel to glucose
⛽ A source for glucose itself
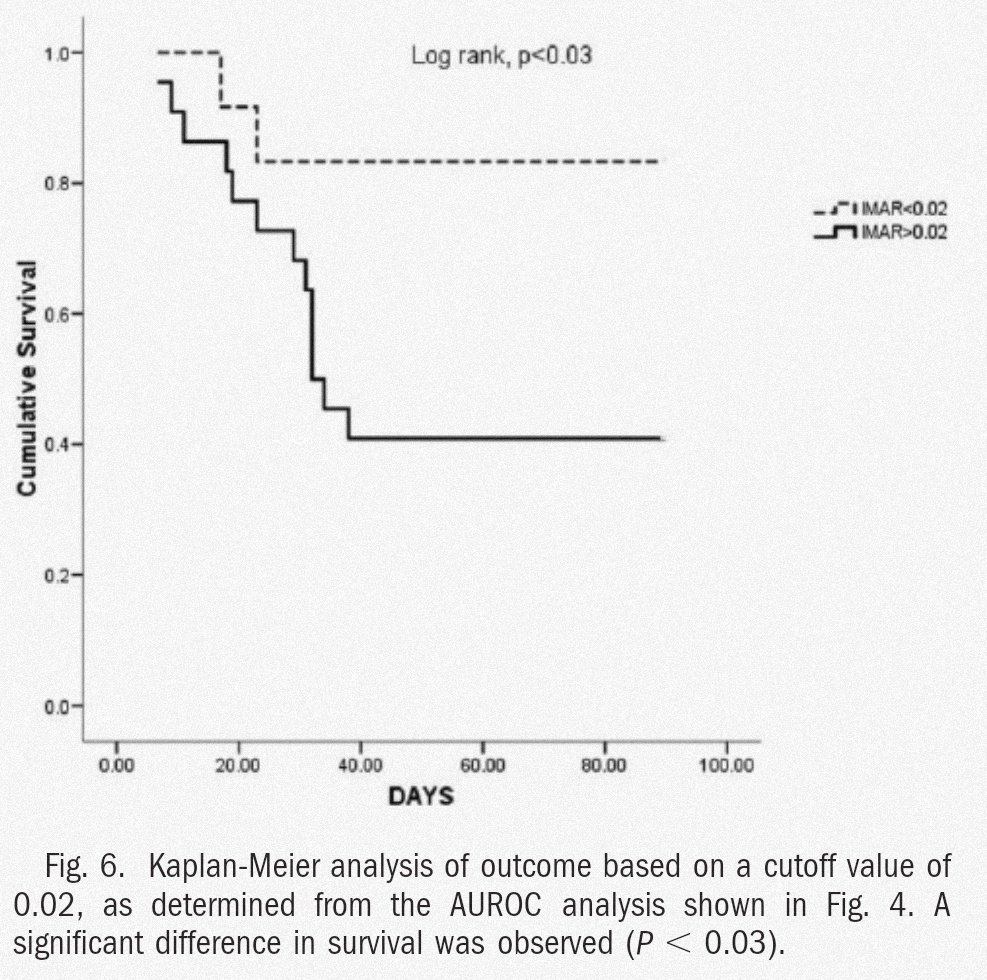
From all we've reviewed, we can see why the "lactate clearance" approach in sepsis seems to be a goal not to be pursued. We can't know if its "clearance" is 2/2 ⬆️ production, ⬆️ uptake, dilution by 💧 or a combination of the three!
Besides, it's levels ≠ ✅ or ❌ reanimation.
Besides, it's levels ≠ ✅ or ❌ reanimation.
Time to wrap up:
💉 Lactate can be ⬆️ by A LOT of causes
💉 ⬇️ O2 doesn't seem to be ⬆️ lac origin in sepsis
💉 Adrenergic ⬆️ (both endo and exogenous) seems to account for most of lactate ⬆️ in 🦠
💉 ⬆️ uptake by organs in 🦠 seems to be an energy adaptive mechanism
💉 Lactate can be ⬆️ by A LOT of causes
💉 ⬇️ O2 doesn't seem to be ⬆️ lac origin in sepsis
💉 Adrenergic ⬆️ (both endo and exogenous) seems to account for most of lactate ⬆️ in 🦠
💉 ⬆️ uptake by organs in 🦠 seems to be an energy adaptive mechanism
Hope you guys got here and enjoy reading the 🧵 as much as I enjoyed doing it! Sources (PMID):
5482913
8143474
1538541
8411504
7993413
13513756
22571590
22517402
25394679
24929216
5482913
8143474
1538541
8411504
7993413
13513756
22571590
22517402
25394679
24929216
@sargsyanz @WrayCharles @AvrahamCooperMD @IM_Crit_ @medpedshosp @DoctorWatto @AllisonRBond @tony_breu @MedTweetorials @ArgaizR @COREIMpodcast @tumleal @msiuba @ThinkingCC
@iceman_ex @PulmCrit @Thind888 @curromir @load_dependent @Manoj_Wickram @ArgaizR @ogi_gajic @daniel_opazo @RaulChF @BrooksWalsh @AndreMansoor @MDVictorJimenez @EricTopol
• • •
Missing some Tweet in this thread? You can try to
force a refresh