Warning - some in-the-weeds tweets about vaccine efficacy trials, new strains, and decision making under uncertainty. I offer more questions than answers, but hopefully it can generate some discussion...
1/6
1/6
For COVID vaccine studies, we can imagine two goals:
(1) We aim to measure efficacy precisely (minimize uncertainty, regardless of the true efficacy), or
(2) We simplify our goal and try to measure if the vaccine is doing well enough - is efficacy above our success threshold? 2/6
(1) We aim to measure efficacy precisely (minimize uncertainty, regardless of the true efficacy), or
(2) We simplify our goal and try to measure if the vaccine is doing well enough - is efficacy above our success threshold? 2/6
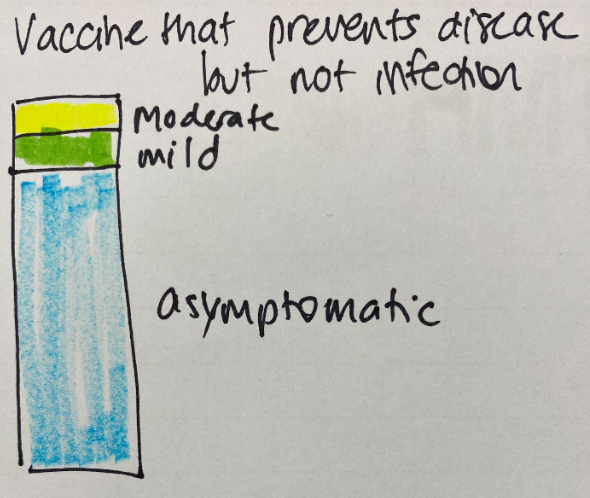
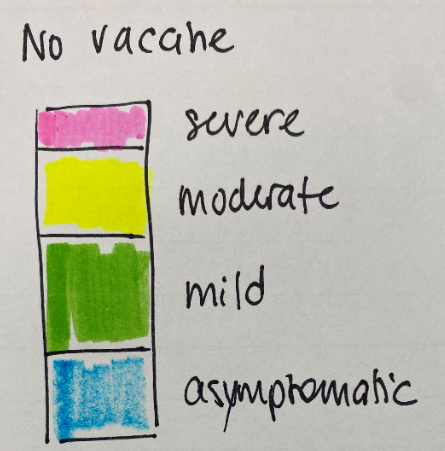
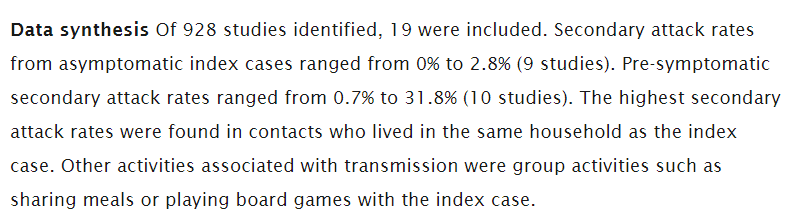
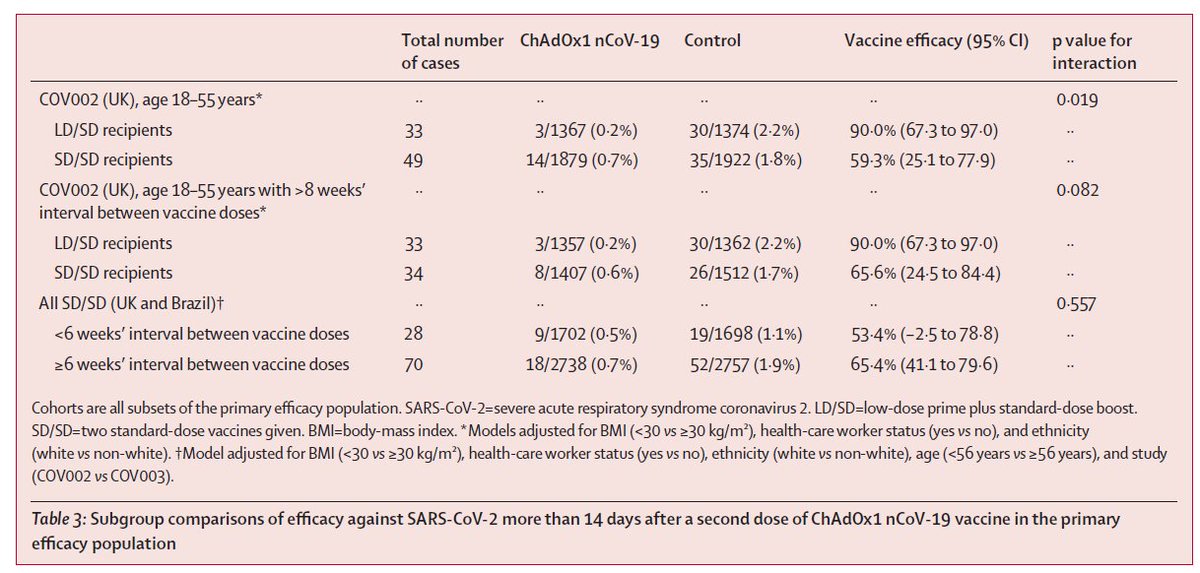
This is relevant for discussions about how well vaccines are performing against different variants. For those who are already vaccinated, we want to know how well the vaccine works against a new strain. What is the efficacy, even if it is lower? This is like the first goal. 3/6
But we are also trying to make decisions about which vaccines to use in the future. Should we care if a vaccine has 20% efficacy or 40% efficacy, if efficacy is below our threshold of 50%? (An honest question.) This is the second type of goal. 4/6
Do we change our goal? Instead of targeting 50% efficacy against disease, do we now target a certain level of efficacy against severe disease? Who decides what that goal should be? And how will we accrue the data needed to check? 5/6
More generally, we have to grapple with how to interpret emerging trial data under uncertainty. We know a vaccine works reasonably well against one strain but not as well against another. How will this impact policy decisions? And what other data do we need to decide? 6/6
• • •
Missing some Tweet in this thread? You can try to
force a refresh