What could happen next with novel variants like P.1 in the UK? There are four possible scenarios. A short thread with some thoughts... 1/
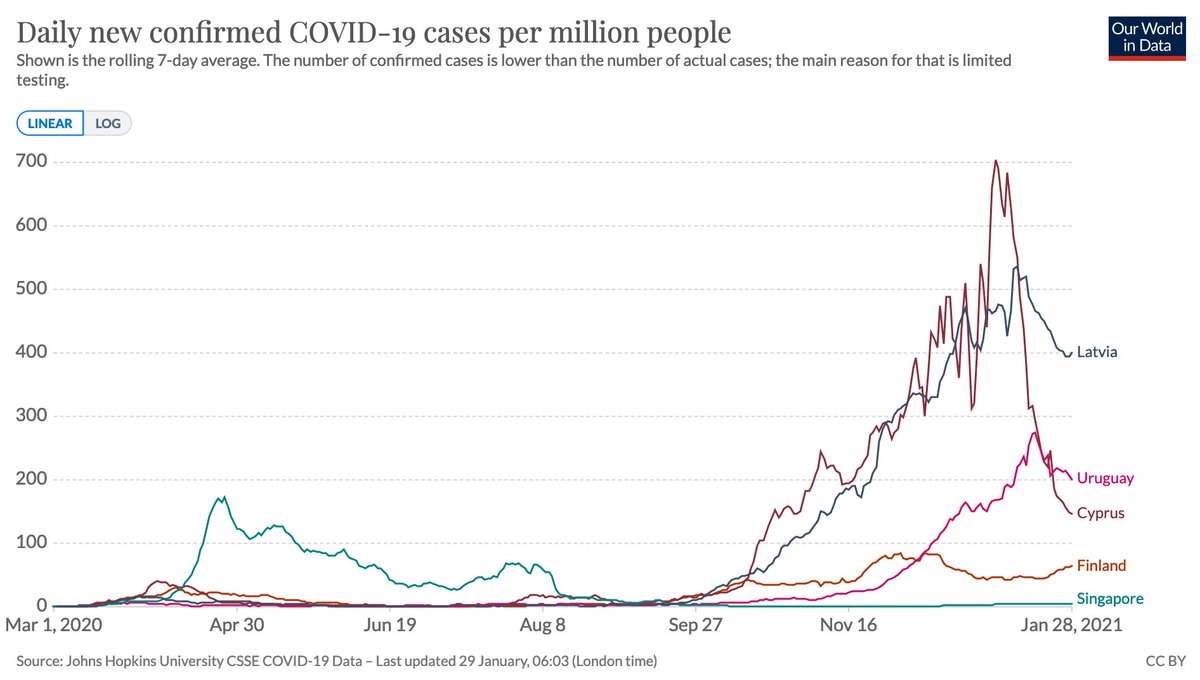
Scenario A: R<1 for both dominant B.1.1.7 variant and other variants of concern like P.1. This is likely situation we're currently in, but staying there is conditional on slow relaxation of control & substantial reduction in infectiousness via vaccines.
https://twitter.com/MoritzGerstung/status/1366059023884312576?s=202/
However, even if R<1 for a novel variant, there could still be a lot of cases to come before outbreak ends, depending on value of R:
https://twitter.com/AdamJKucharski/status/1324662478316408833?s=203/
Scenario B: R>1 for B.1.1.7 variant but R<1 for variants of concern identified in Brazil/South Africa etc. (let's call these nVOCs). This could happen if measures relaxed overall, but aggressive targeted containment prevents imported nCOVs taking hold. 4/
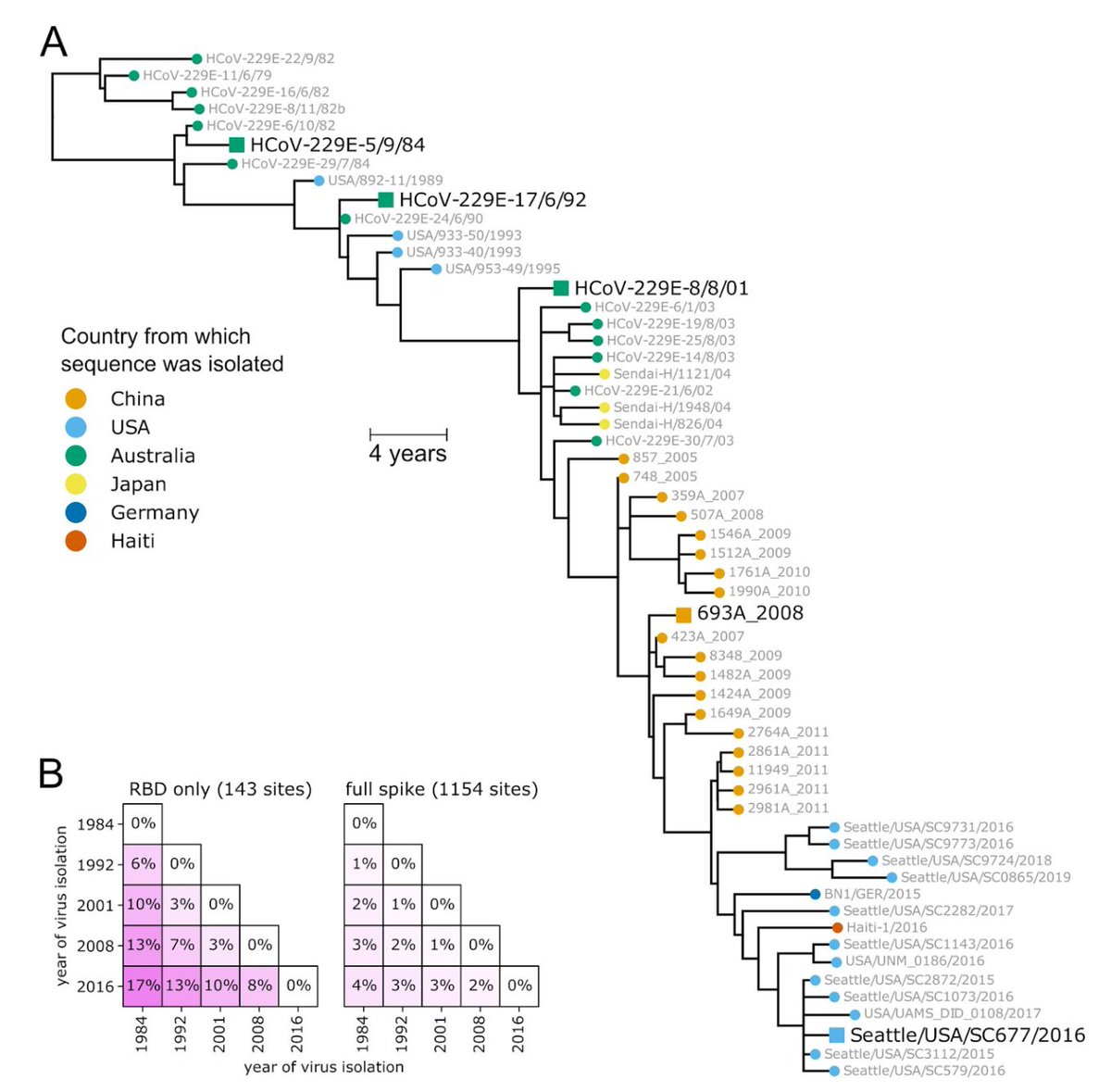
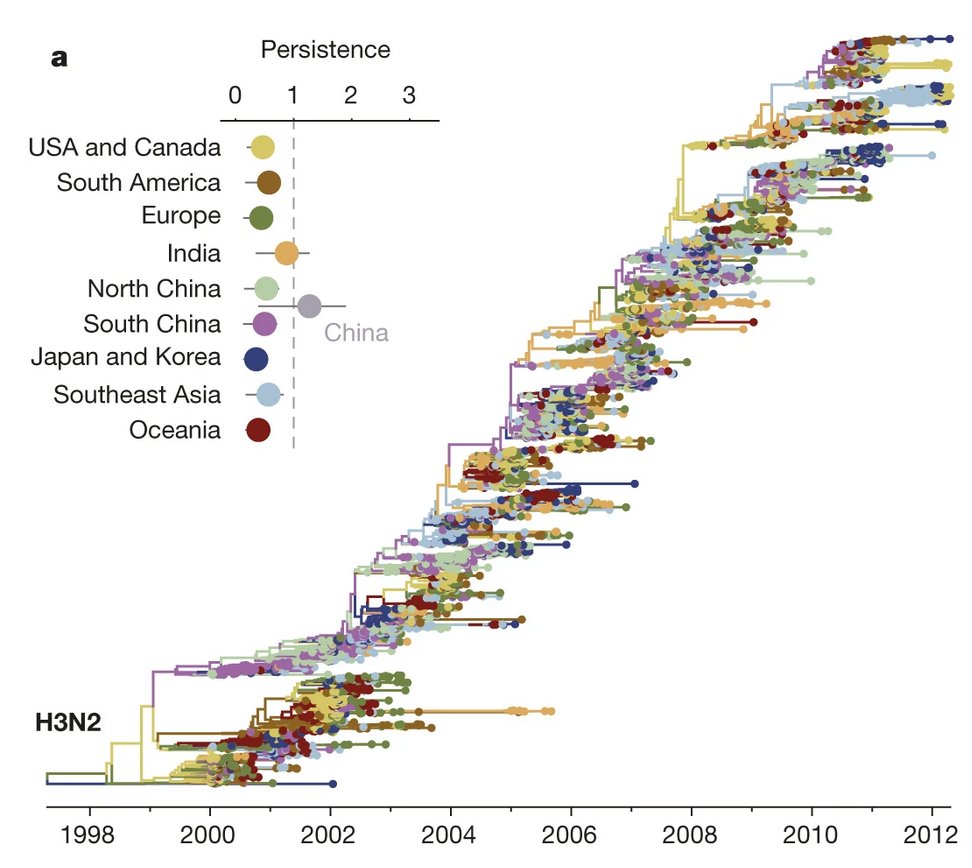
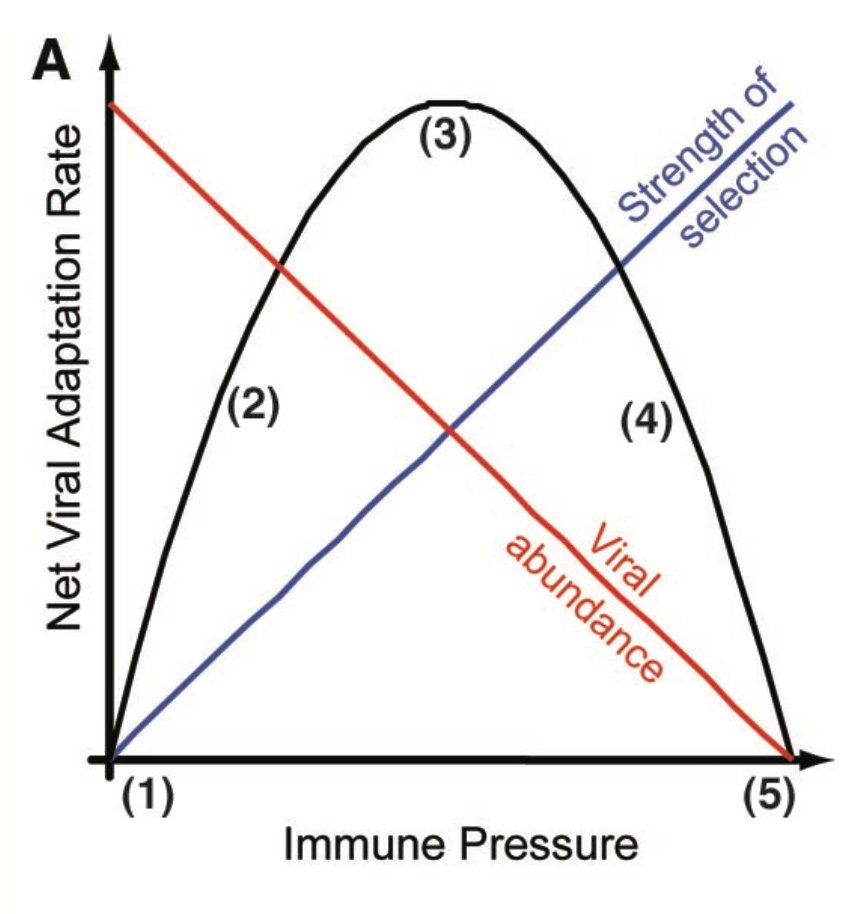
Of course, this doesn't account for novel variants of concern that emerge domestically but aren't immediately detected, which could well happen if transmission ongoing in a partially vaccinated population:
https://twitter.com/AdamJKucharski/status/1358762039569694725?s=205/
Scenario C: R<1 for B.1.1.7 but R>1 for nVOCs. At the moment, the low reproduction number for B.1.1.7 depends both on accumulated immunity and control measures. So if nVOCs can escape immunity to some extent and take hold, they could grow even if B.1.1.7 slowly declining. 6/
More on the point at which this cross-over could occur:
https://twitter.com/AdamJKucharski/status/1359193937907449863?s=207/
Scenario D: R>1 for B.1.1.7 and R>1 for nVOCs. If UK reopening follows the provisional dates not data, then could end up in this scenario, and outcome would depend on how well vaccines work against nVOCs... 8/
Vaccines are still likely to have some effect against the currently identified variants (e.g. helping to prevent more severe outcomes) but the exact impact is currently uncertain:
https://twitter.com/profshanecrotty/status/1355552003531755521?s=209/9
• • •
Missing some Tweet in this thread? You can try to
force a refresh