1/11💧 Urine albumin-to-creatinine ratio (UACR) testing in type 2 diabetes (#T2D) – a brief tutorial
👉 What is it?
👉 Why it’s an important complement to eGFR 💉 testing to identify chronic kidney disease (#CKD) in #T2D
COI: #BayerPartner #ItstheKidney ckd-t2d.com
👉 What is it?
👉 Why it’s an important complement to eGFR 💉 testing to identify chronic kidney disease (#CKD) in #T2D
COI: #BayerPartner #ItstheKidney ckd-t2d.com
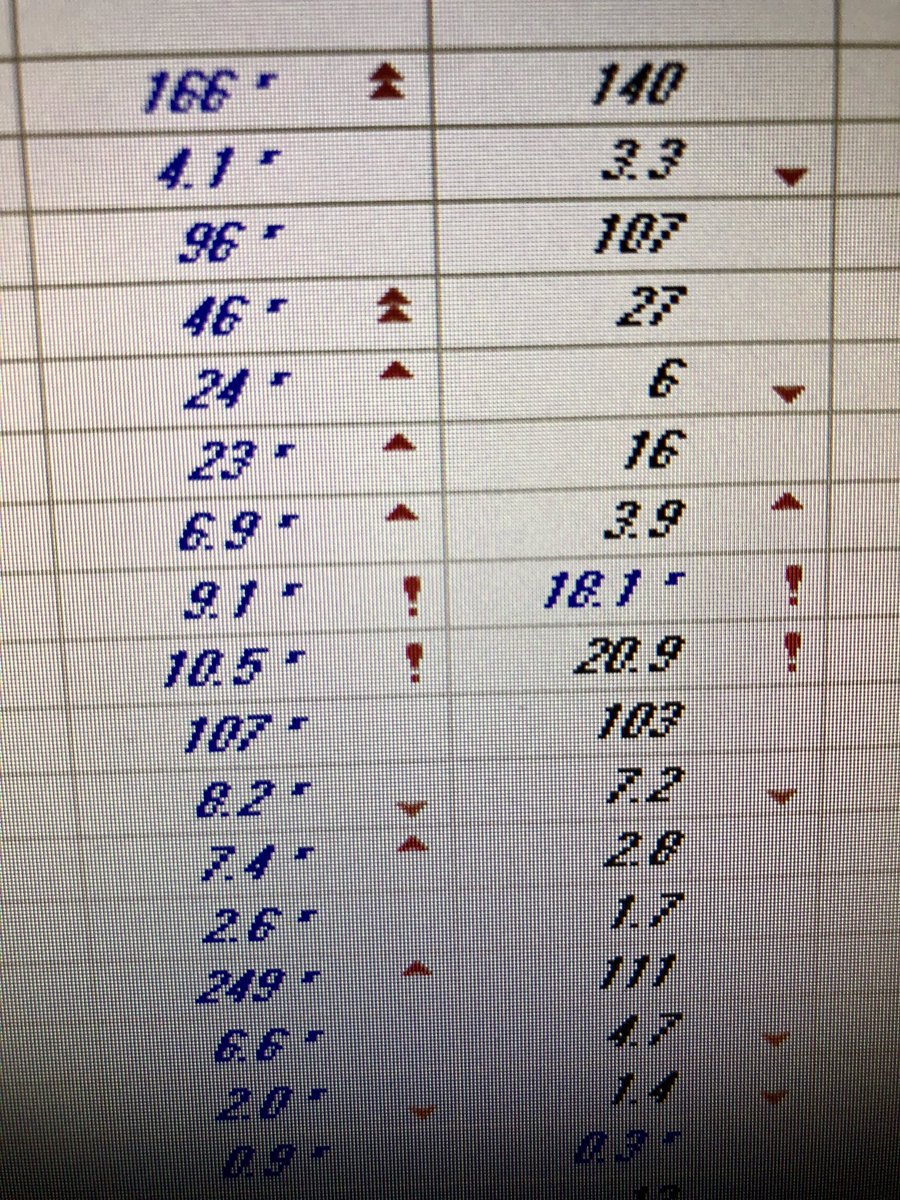
2/11📈UACR estimates 24-hour urine albumin excretion (g/day), assuming that ~1 g of creatinine is excreted in the urine daily.
3/11 An important paper by @NephRodby shows the usefulness of urine protein-to-creatinine ratio (UPCR) in predicting 24-hour protein excretion while critically assessing the values at hand. ajkd.org/article/0272-6… 

4/11 📈Use of UACR to estimate 24-hour urine assessments is supported by longitudinal studies; an example from the Asian Kidney Disease Study (Boon Wee Teo et al 2015; n=232) showed a correlation of r=0.86 between the 2 measures. pubmed.ncbi.nlm.nih.gov/25649135/ 

5/11 Importantly, a young muscular patient 🏋️♂️ may excrete 2 g/day of creatinine; thus, a UACR of 0.5 g/g would be 1 g/day albumin, not 0.5 g/day. Conversely, a thin older patient 👵 may only excrete 0.75 g of creatinine/day; thus, UACR of 0.5 g/g would be 0.375 g/day. 

6/11❔Despite recommendations for annual testing by the American Diabetes Association (ADA), what percentage of patients with #T2D had UACR tests in the ADD-CKD study?
7/11✔The correct answer is (b); only 53% of patients had UACR tests, despite annual testing recommendations by the ADA. Link to the ADD-CKD study here: pubmed.ncbi.nlm.nih.gov/25427285/
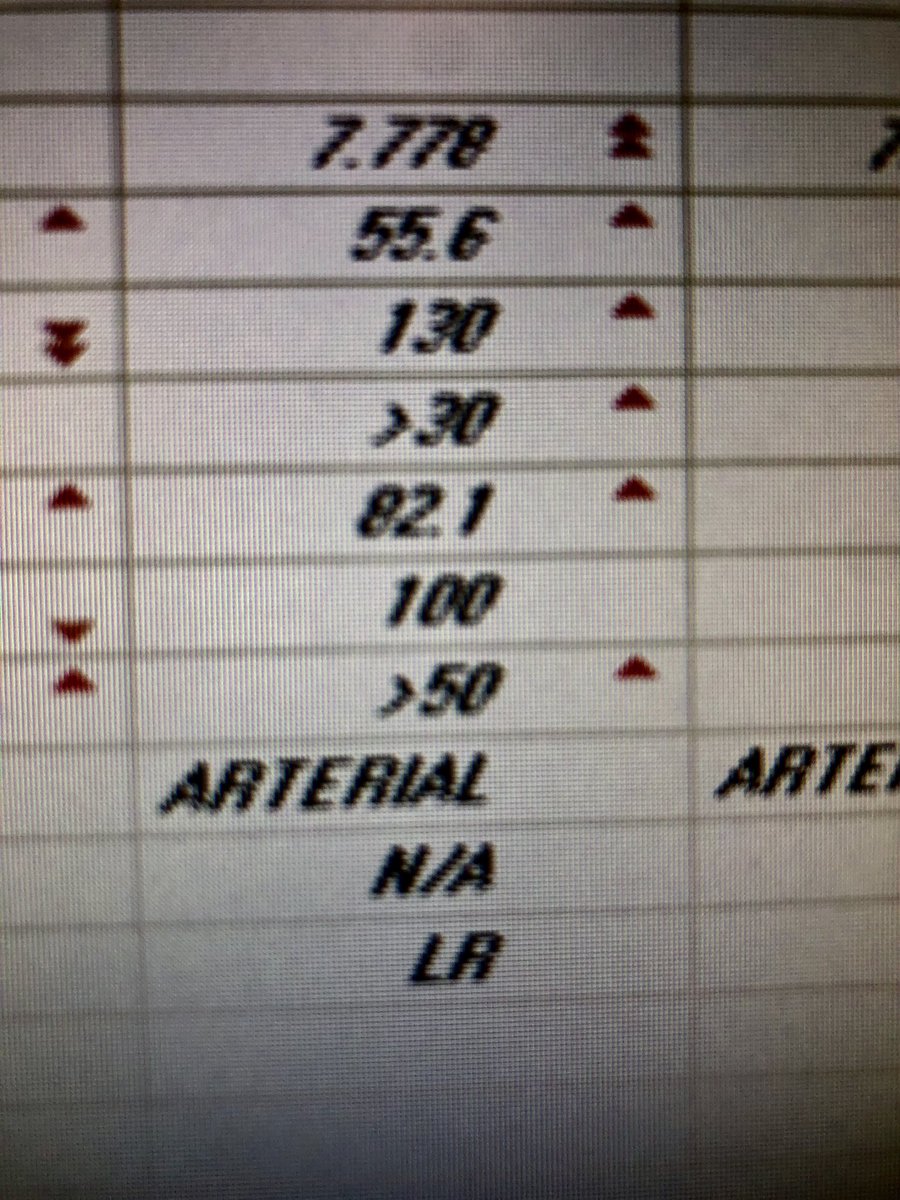
8/11 🔽Underutilization of UACR testing is critical, as we know that kidney damage in #T2D, as evidenced by albuminuria (UACR ≥30 mg/g), can occur years ⏰ before impaired kidney function is detected (eGFR <60 mL/min/1.73 m2). (ncbi.nlm.nih.gov/pmc/articles/P…) 

9/11 Although this is a known fact, it is important to reiterate that albuminuria (UACR ≥30 mg/g) and impaired eGFR (<60 mL/min/1.73 m2) are also both independently associated with increased mortality in patients with #T2D. (pubmed.ncbi.nlm.nih.gov/23362314/) 

10/11 📋 When assessing risk for #CKD, monitoring patients with #T2D at least once a year should include UACR and eGFR. As shown, a patient with eGFR 58 mL/min/1.73 m2 but UACR 700 mg/g is at a greater risk than a patient with eGFR 45 mL/min/1.73 m2 and UACR 50 mg/g. 

11/11 👉 Remember, when referring to a patient with #CKD, “baseline eGFR” is only half of the story; the other half should always be “baseline UACR.” 

• • •
Missing some Tweet in this thread? You can try to
force a refresh