1/ Haven't done this in awhile, but want to share some great literature we discussed this week while on the @UNMC_ID general ID service! So happy to have a big multidisciplinary team led by @DrJRMarcelin along with our pharmacists @Molly_M_Miller & @bergmanscott!
2/ Will start with my favorite article on carbapenem-resistant gram-negative infections from Doi et al with my own adaptation of their super useful table
academic.oup.com/cid/article/69…
academic.oup.com/cid/article/69…

3/ We continue to #RespectTheStaph learning of an unusual manifestation of Staph aureus prostatic abscess from a future @UNMC_ID fellow's paper & another lit review.
academic.oup.com/ofid/article/6…
ncbi.nlm.nih.gov/pmc/articles/P…
academic.oup.com/ofid/article/6…
ncbi.nlm.nih.gov/pmc/articles/P…
4/ Key risk factors for Staph aureus prostatic abscess (PA) include SSTI, hx of GU disease or instrumentation, IVDU, DM, immunodeficiencies & hepatitis C
Most present with GU symptoms & concomitant bacteremia is common
Think of PA when dysuria & Staph aureus bacteremia co-exist
Most present with GU symptoms & concomitant bacteremia is common
Think of PA when dysuria & Staph aureus bacteremia co-exist
5/ I've previously heard of VISA & VRSA, but there is also a phenomenon of VISA in patients with MSSA that I was unfamiliar. This is not due to VanA acquisition, but rather increased cell wall thickness & altered PBPs.
aac.asm.org/content/61/7/e…
academic.oup.com/cid/article/49…
aac.asm.org/content/61/7/e…
academic.oup.com/cid/article/49…
6/ Do you have to treat all patients with findings of candidiasis on EGD?
Well, not if the patient is asymptomatic & immunocompetent. Treatment does not change the natural history for these cases.
pubmed.ncbi.nlm.nih.gov/29702297
pubmed.ncbi.nlm.nih.gov/26083902
ncbi.nlm.nih.gov/pmc/articles/P…
Well, not if the patient is asymptomatic & immunocompetent. Treatment does not change the natural history for these cases.
pubmed.ncbi.nlm.nih.gov/29702297
pubmed.ncbi.nlm.nih.gov/26083902
ncbi.nlm.nih.gov/pmc/articles/P…
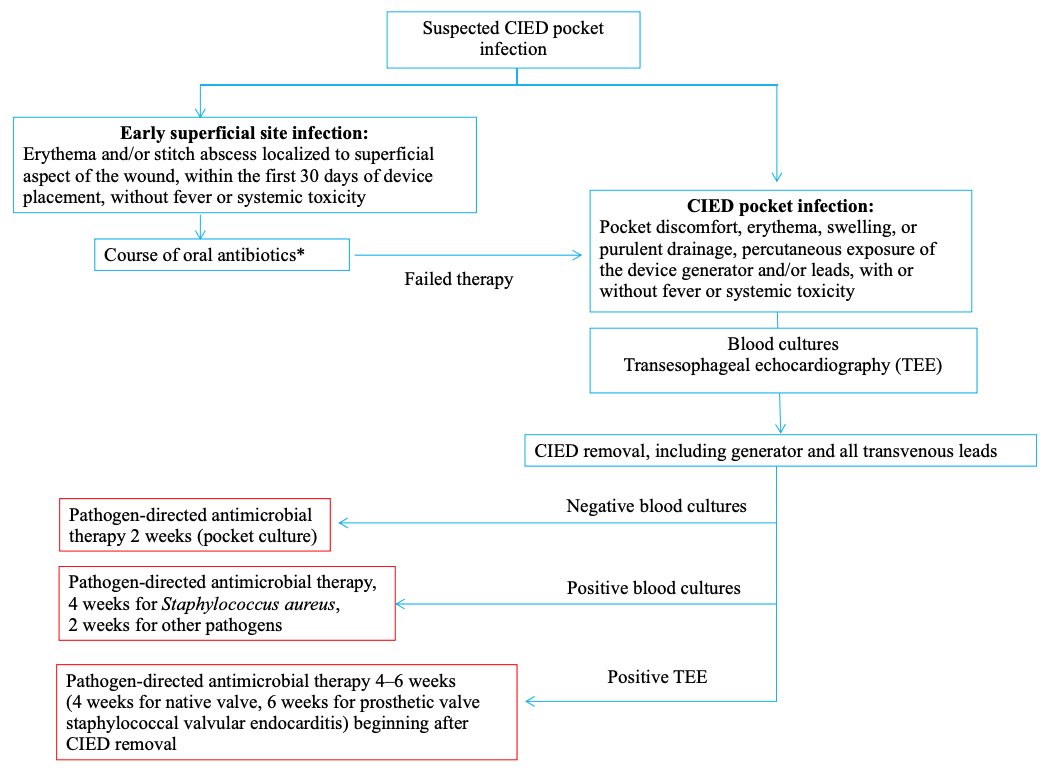
7/ I've officially stored the CIED guideline algorithms to my phone now, these flowcharts are clutch for #IDFellows
hrsonline.org/guidance/clini…


hrsonline.org/guidance/clini…


8/ Lastly, a quick review of antibiotics that are safe in pregnancy (Category B):
👌Beta-lactams
👌Vancomycin
👌Azithromycin
👌Clindamycin
👌Daptomycin
👌Metronidazole
👌Nitrofurantoin
👌Fosfomycin
🚫Avoid: FLQs, Tetracyclines, AGs & TMP-SMX
pubmed.ncbi.nlm.nih.gov/26598097
👌Beta-lactams
👌Vancomycin
👌Azithromycin
👌Clindamycin
👌Daptomycin
👌Metronidazole
👌Nitrofurantoin
👌Fosfomycin
🚫Avoid: FLQs, Tetracyclines, AGs & TMP-SMX
pubmed.ncbi.nlm.nih.gov/26598097
• • •
Missing some Tweet in this thread? You can try to
force a refresh