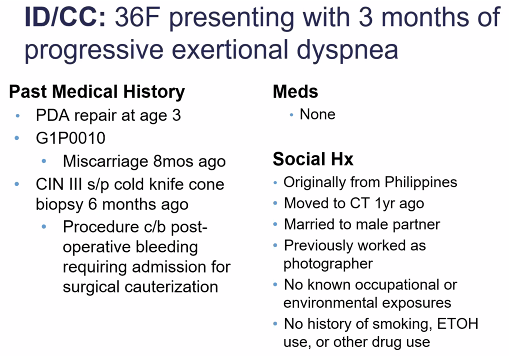
Excited for our upcoming Case of the Year Presentation by Drs. Hilary Zetlen and @tpeck_86, "Under Pressure: Trading One Problem for Another". Will be live-tweeting the case (to the best of my ability) below so you can follow along!
https://twitter.com/HarvardPulm/status/1369789019190665217
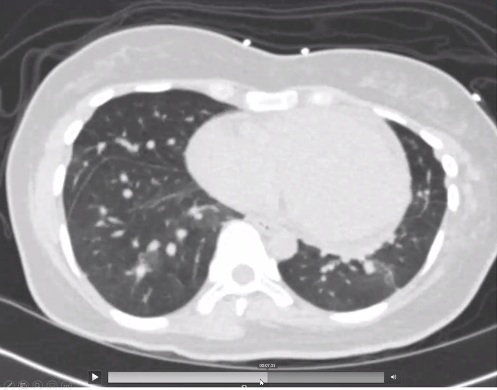
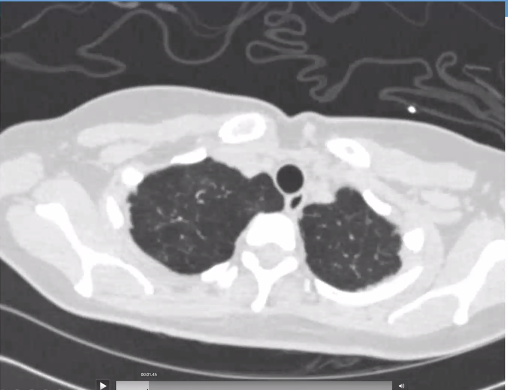
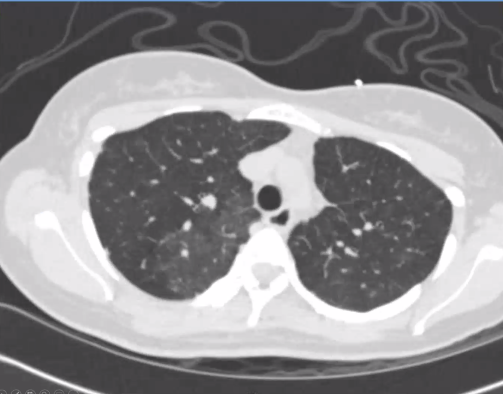
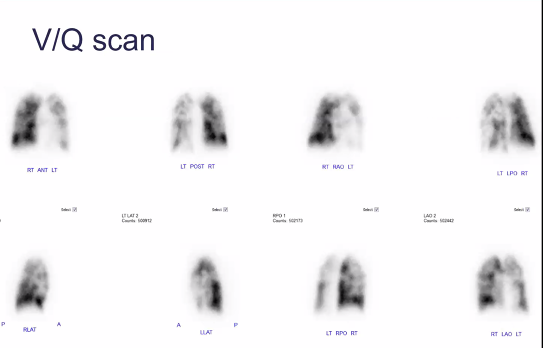
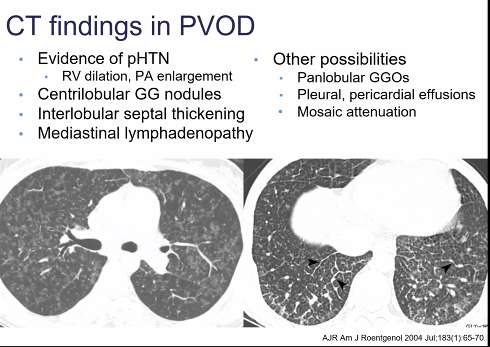
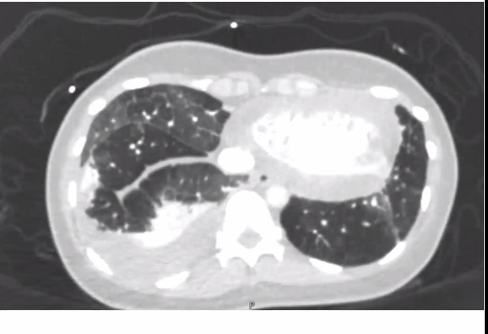
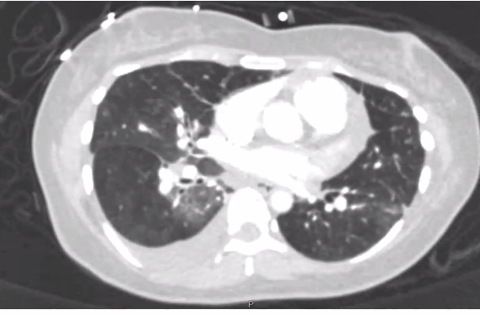
Lots of mosaic attenuation!
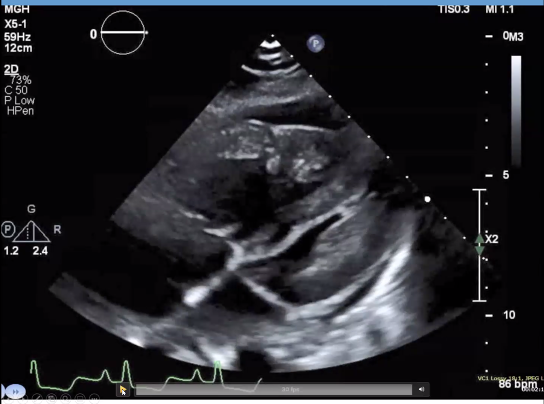
Both ventricles but RV in particular is hypertrophied and dilated, RVSP 91, + pericardial effusion.
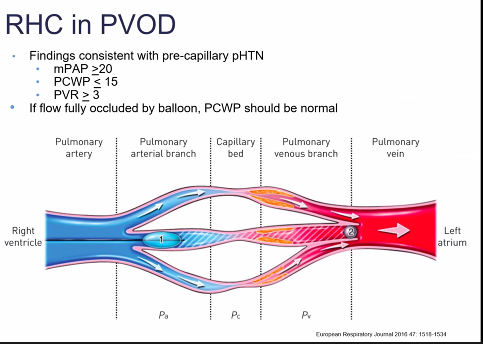
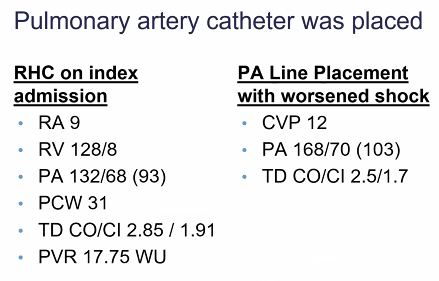
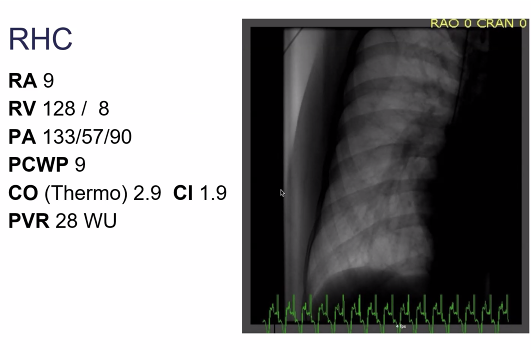
Undergoes a RHC as below and bilateral PAgram which shows normal vasculature - does NOT look like CTEPH! The plot thickens. 
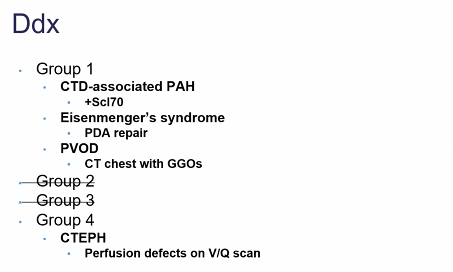
Thoughts? Differential diagnosis?
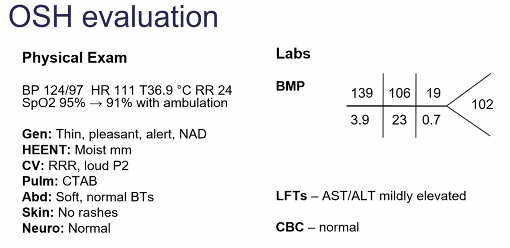
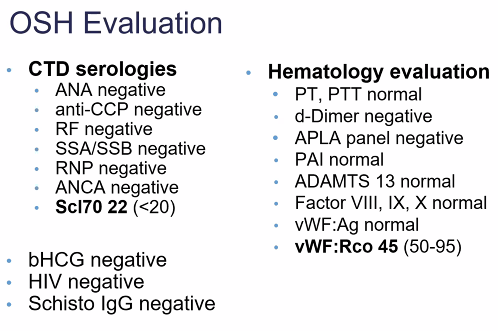
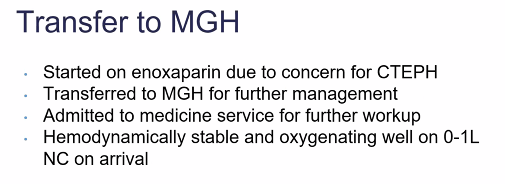
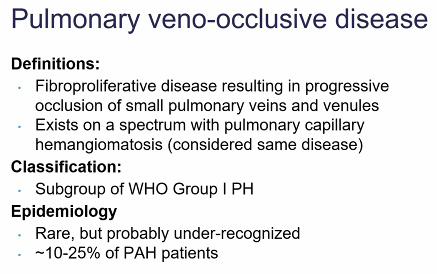
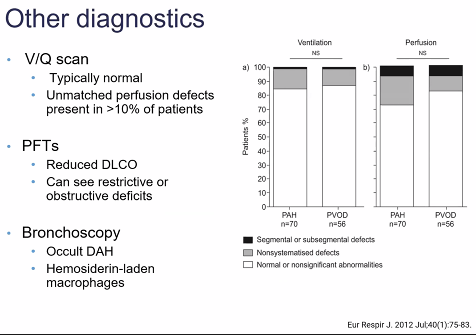
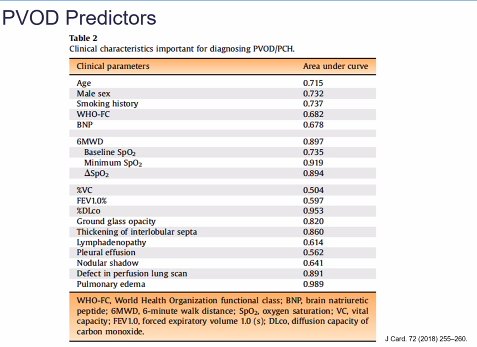
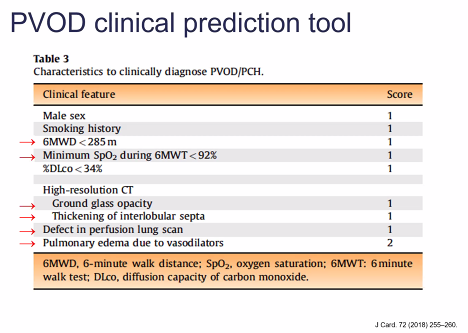
In summary: 36W with subacute worsening dyspnea on exertion, CT with mosaic attenuation, significant RV hypertrophy and dilation, VQ scan suspicious for CTEPH but PAgram negative, RHC with severe pre-capillary PH - mPA 90, PCWP 9, serology notable for slightly low vWF, weak + Scl
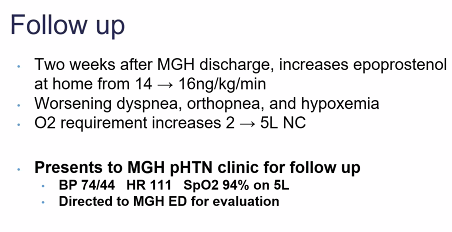
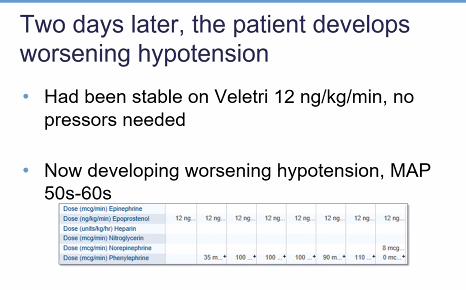
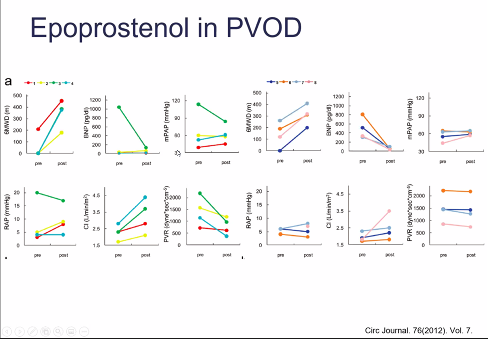
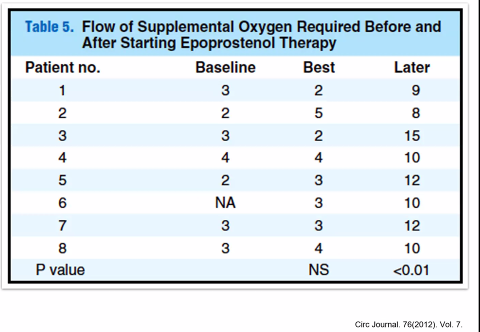
She's started on IV epo, sildenafil, ambrisentan. O2 requirement improves to 1-2L and is discharged on this triple therapy....but later returns.
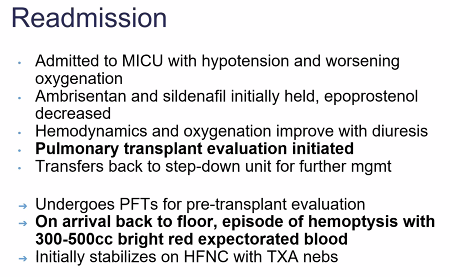
She goes to the ED and gets another CT... mosaicism is still there but now she has a new bilateral pleural effusions and interlobular septal thickening and atelectasis. 


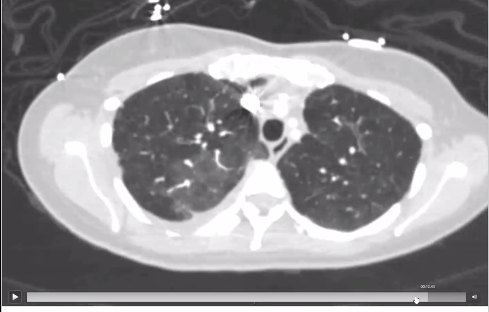
So both the plot, and the interlobular septa, have thickened.
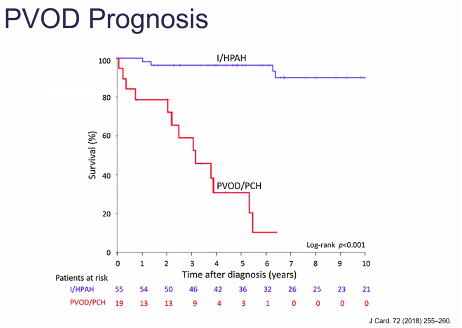
PVOD prognosis is poor... Median survival was 3.5 years from diagnosis, compared to > 25 years in other pulmonary hypertension. 
What can we do? Diurese, provide oxygen... and some evidence for immunosuppression and TKIs for some patients, refer for transplant. 
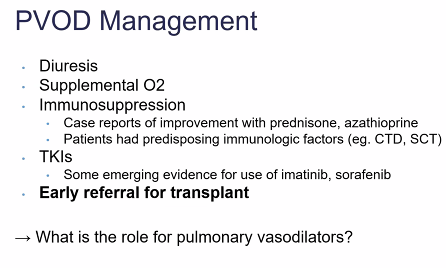
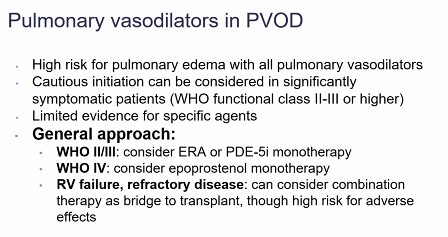
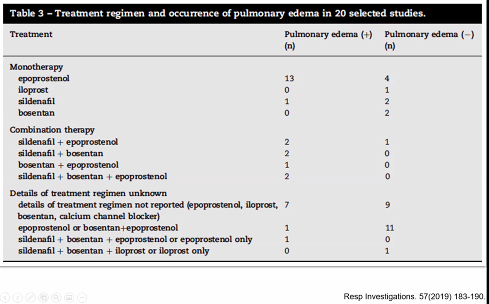
Pulmonary vasodilators? This patient had the classis pulmonary edema response to vasodilators. Can they ever be tried? Dr. Zetlen says, yes - sometimes can be considered and helps for some patients, but pulmonary edema is extremely likely. Not all patients are the same! 



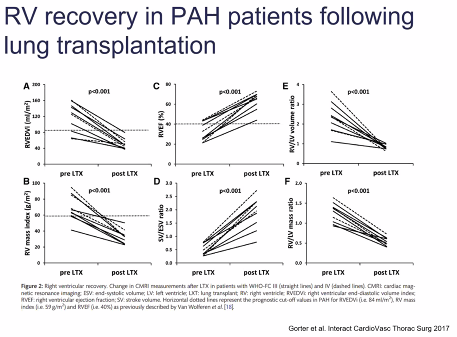
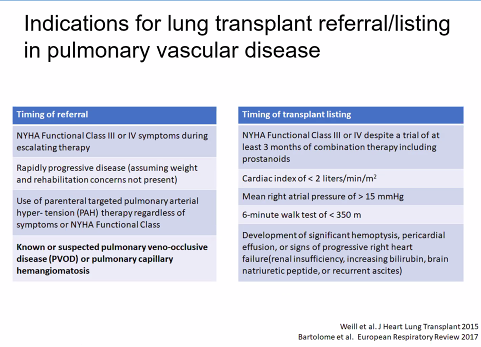
So when do you send for transplant? @tpeck_86 is taking us through this. Our patient's Lung Allocation Score was 63. the 90th percentile is 51.9. 
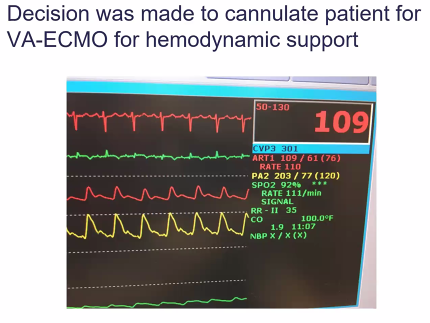
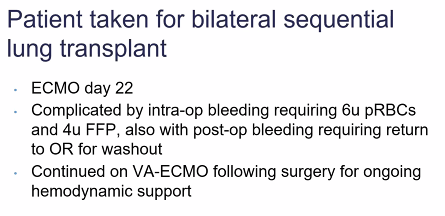
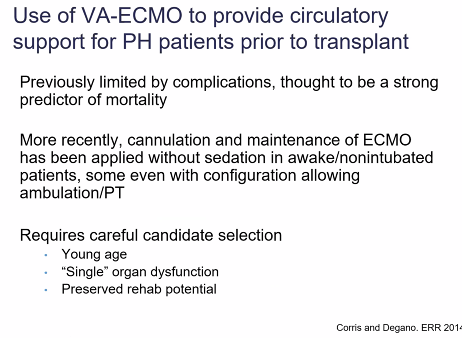
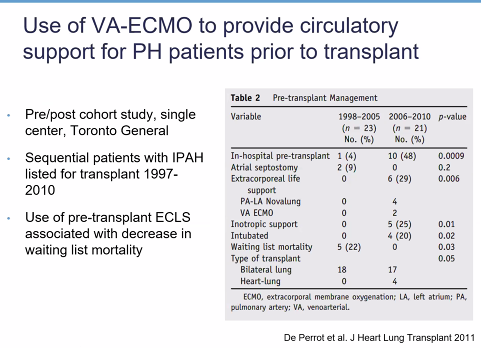
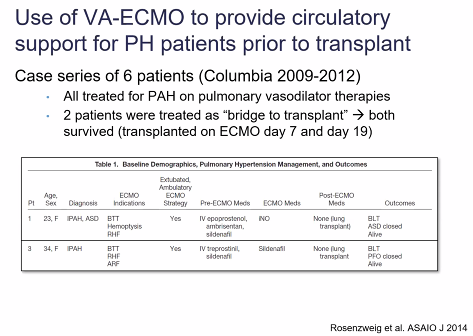
Wait... VA ECMO in PH? Yes, says Dr. Peck - with improved ECMO technology, pre-transplant has begun to improve mortality in the right patients. 


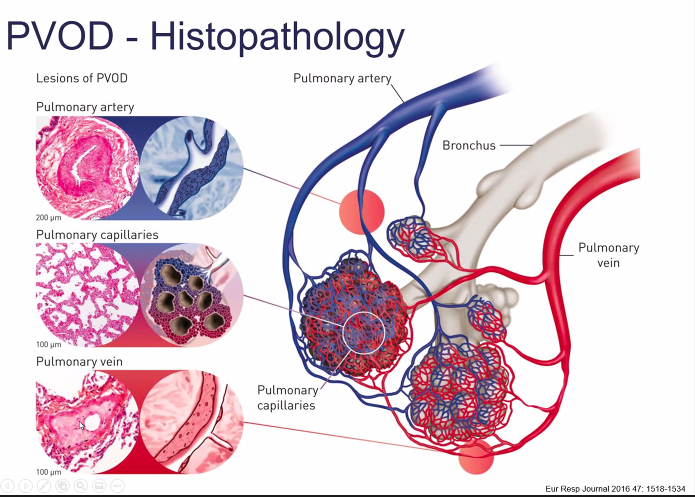
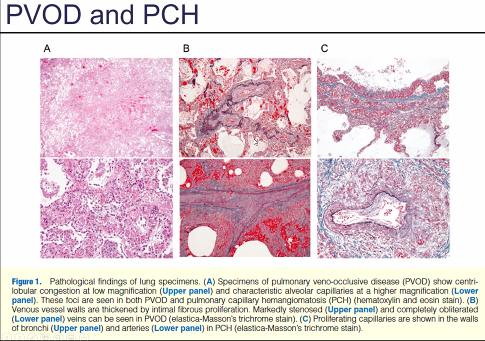
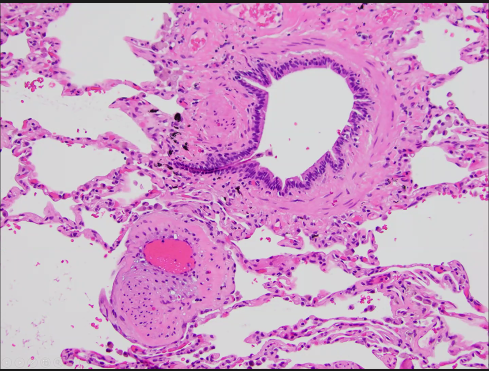
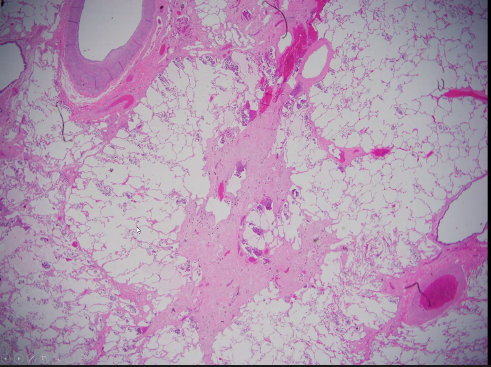
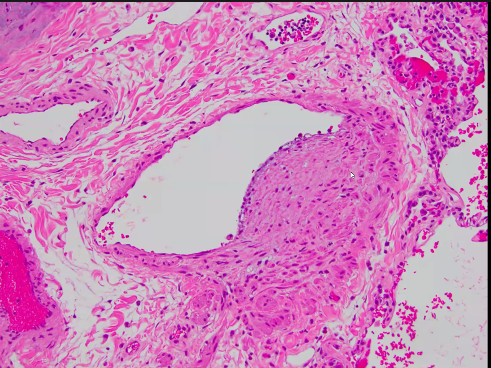
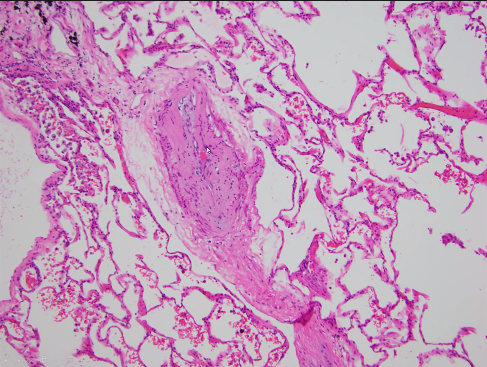
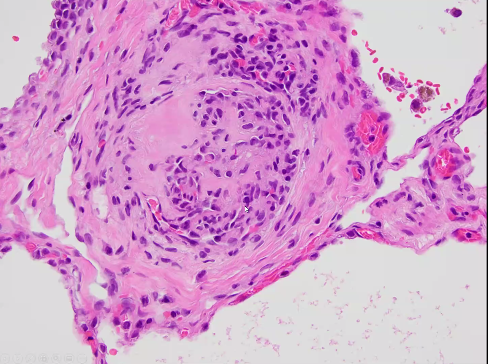
This of course means we now have pathology...Dr. Zetlen (with appreciation to our pathologist extraordinaire Dr. Lida Hariri) shows smooth muscle hypertrophy of pulmonary veins/venules, some completely occluded. 



Unfortunately post-transplant, the patient had hemorrhagic conversion of a known ischemic stroke, so was decannulated from VA ECMO on POD#4. 
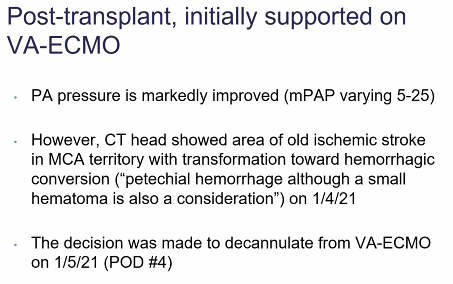
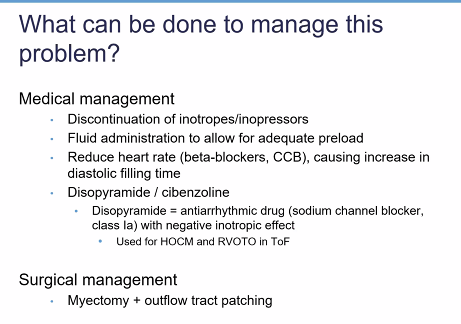
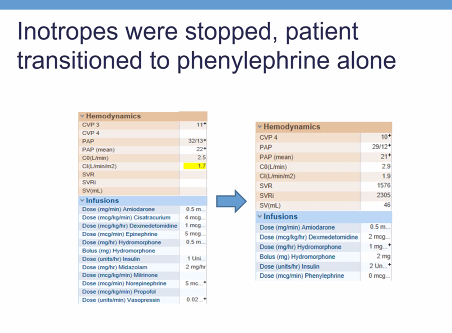
Post-decannulation, she went into high-grade shock. @RazYuval, both our ECMO and Lung Transplant expert, taking us through his approach to this emergency situation. 
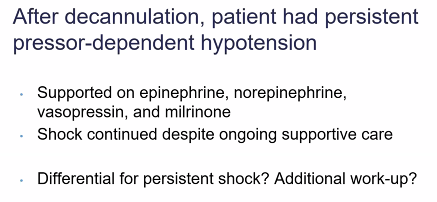
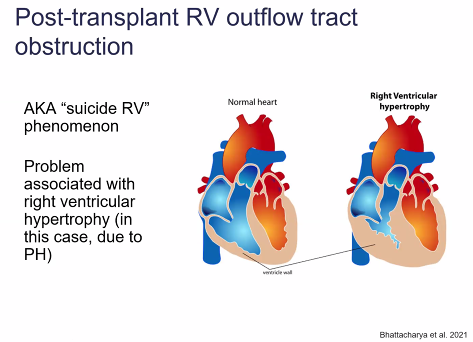
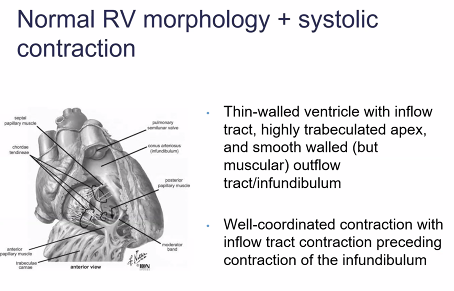
@RazYuval: Differential includes hemorrhage, sepsis, reperfusion injury, RV dysfunction or outflow obstruction given her severe RV disease, perioperative vasoplegia (out of window)
Back to the case: PA pressures as below, and TEE performed with concern for RV outflow tract obstruction 


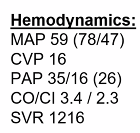
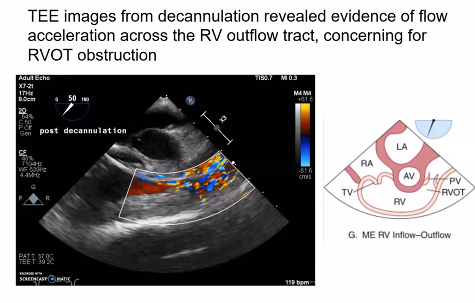
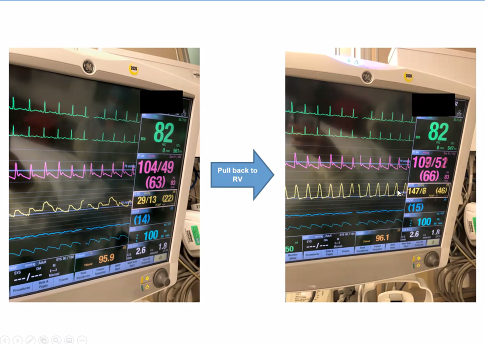
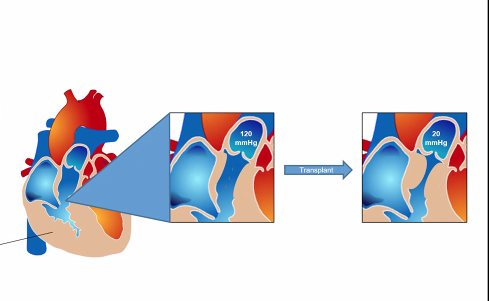
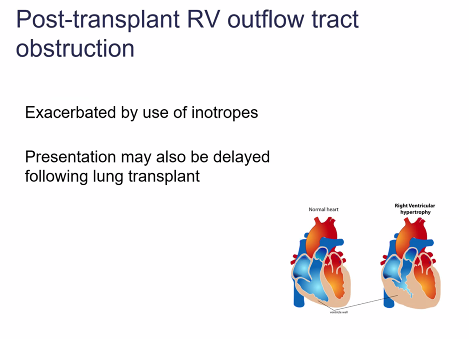
But in this patient, given her R heart disease, ended up with post transplant RVOT obstruction from relative reduction in PA pressures! 


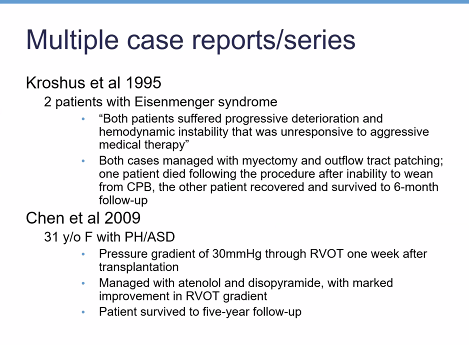
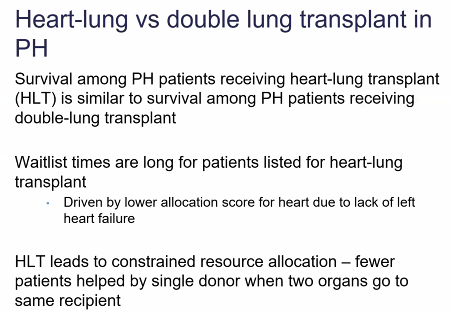
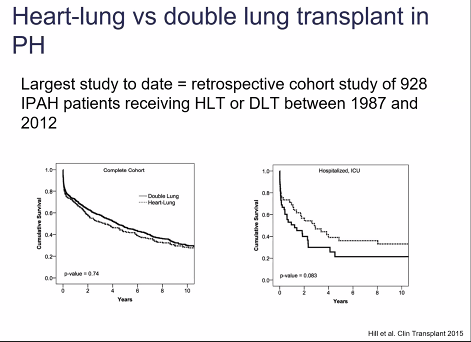
Should she have gotten a heart-lung transplant? May benefit some patients, but has its own host of issues to consider. 

That's a wrap. Such an incredible case, thank you Dr. Zetlen and Dr. Peck (@tpeck_86)! They also wish to credit PH & ECMO doc extraordinaire @AWitkin, aforementioned pathologist extraordinaire Dr. Lida Hariri, and @harvardpulm Program Director extraordinaire Dr. Asha Anandaiah
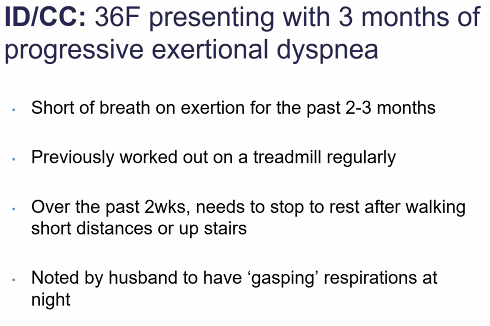
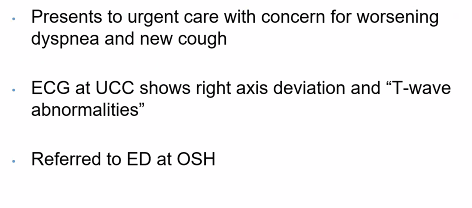
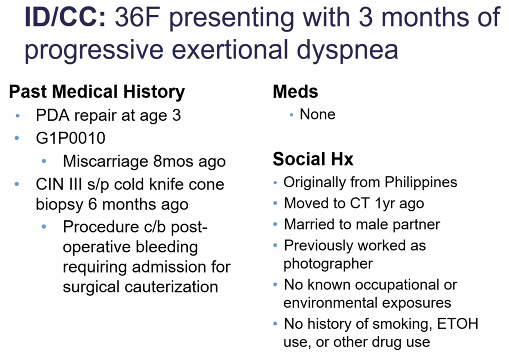
Whoops - seem to have accidentally started a new thread for the rest of the case. Case continues with the remainder of the HPI in image below, followed by CT scan here:

https://twitter.com/JonahRubinMD/status/1369807054903316482?s=20
• • •
Missing some Tweet in this thread? You can try to
force a refresh