Excited to have @siddharth_dugar from @ClevelandClinic give the #MetroEUS Ultrasound Lecture today about Critical Care ECHO. #POCUS #FOAMed #FOAMus #EchoFirst @MetroHealth_EM @metrohealthCLE @RJonesSonoEM @mtabbut @SLWerner_EM @DianeGramer 

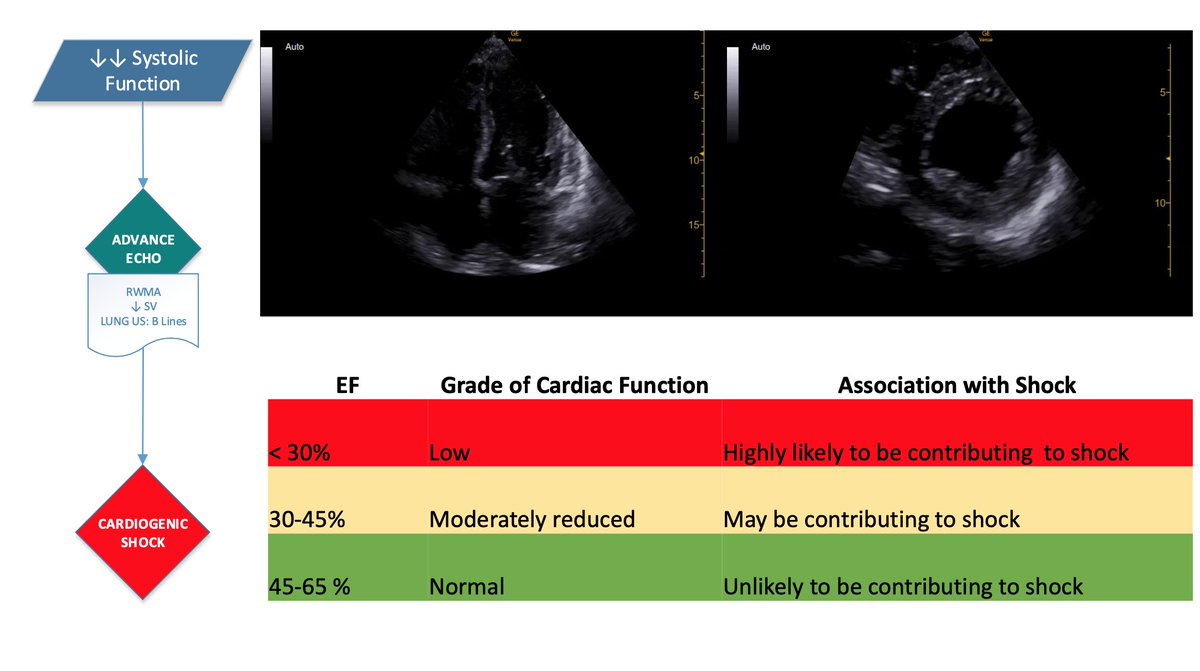
Goal and benefit of POCUS is to rapidly narrow the differential diagnosis through asking and answering defined clinical questions. 

Start looking for an effusion. Differentiate pericardial vs pleural effusion. Key: look for the descending thoracic aorta in the PSLA view. Fluid above = pericardial (blue), fluid up to and below = pleural (green) 



Does the patient have tamponade? Look at the IVC. If small, then likely no tamponade. If enlarged, need to look for other factors. 

RA/RV collapse to assess for tamponade is limited in patients with advanced pulmonary hypertension due to high RA/RV pressures. Teaching Pearl: look at the LA free wall as this is the lowest pressure chamber. #MicDrop @siddharth_dugar #FOAMus 

Look for other signs of RV strain: Plethoric IVC, Flattened septum (D sign). If you find DVT or see McConnell's sign (remember patient in shock), then PE is your major concern. 



Still can't find the cause of shock? Look for severe valvular regurgitation, LVOT obstruction, aortic dissections. 

• • •
Missing some Tweet in this thread? You can try to
force a refresh