Is 6' of space required to keep kids safe in schools, or is 3' enough?
One of the most important questions for re-opening schools safely.
Thread
tl;dr New paper suggests 3' is enough, but paper is fraught with issues & is unconvincing, even though I really wanted it to be right.
One of the most important questions for re-opening schools safely.
Thread
tl;dr New paper suggests 3' is enough, but paper is fraught with issues & is unconvincing, even though I really wanted it to be right.
Background
SARS-COV-2 transmission in children has been one of the most contentious issues of the pandemic. Schools were closed in most of the world in early 2020 b/c kids play a big role in influenza transmission & without info, same was assumed for SARS-COV-2.
SARS-COV-2 transmission in children has been one of the most contentious issues of the pandemic. Schools were closed in most of the world in early 2020 b/c kids play a big role in influenza transmission & without info, same was assumed for SARS-COV-2.
A mountain of evidence now shows that cases/infections in children (especially <10yr) are often (but not always) less likely to be detected than in adults & kids transmit less often. There's many issues w/ these data, but no time for that here (need to write big review thread).
A few threads I've written on this:
https://twitter.com/DiseaseEcology/status/1264958546367483914
https://twitter.com/DiseaseEcology/status/1274803608836399104
https://twitter.com/DiseaseEcology/status/1288733577274744832
https://twitter.com/DiseaseEcology/status/1297940479640629248
https://twitter.com/DiseaseEcology/status/1286826597916401666
https://twitter.com/DiseaseEcology/status/1287528401134223360
https://twitter.com/DiseaseEcology/status/1289018229516460032
https://twitter.com/DiseaseEcology/status/1283849558246617088
https://twitter.com/DiseaseEcology/status/1333113400570781696
Evidence also shows that kids of all ages CAN become infected & transmit - key Q is whether they do it at equal rates as adults?
There have also been many outbreaks of COVID-19 in schools globally. Follow @DrZoeHyde to see a never ending stream of these reports.
There have also been many outbreaks of COVID-19 in schools globally. Follow @DrZoeHyde to see a never ending stream of these reports.
This has led to even the most strident proponents of kids playing minor role in transmission (e.g. @apsmunro) acknowledging that kids can get infected & transmit if no precautions are taken. I'd venture a guess (a hope?) that all reasonable scientists would admit this.
Thus, the CDC, in trying to offer guidance on school re-opening (cdc.gov/coronavirus/20…) has suggested that schools focus on 2 things: masks & 6' distance. They list 3 other (mostly useless) things & neglect ventilation (@jljcolorado @linseymarr @zeynep). But I digress... 

The biggest, most important thing CDC recommended was 6'. Why? Because all public schools can require masks but most (nearly all) CANNOT provide in-person schooling at normal capacity & provide 6' space b/w students. There simply isn't building space.
This has led to a lose-lose set of options including hybrid classes, double-day classes, every other day classes, etc., which have been tough for students, teachers & parents w/ possibly no benefit in terms of reduced risk due to cohort switching. A bit of a disaster, really.
A big ongoing Q has been, is 6' needed? Would 3' be enough if students were all wearing masks? What does "enough" mean?
New paper compares COVID-19 incidence in school district w/ 3'+ & 6'+ rules.
@vdbPolly @BranchWestyn @ProfEmilyOster
academic.oup.com/cid/advance-ar…
New paper compares COVID-19 incidence in school district w/ 3'+ & 6'+ rules.
@vdbPolly @BranchWestyn @ProfEmilyOster
academic.oup.com/cid/advance-ar…
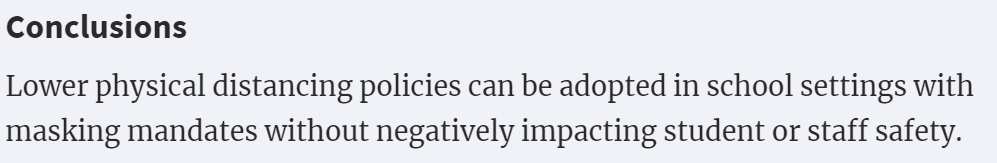
What did it find? Conclusions are bold: 3' is "enough"; 6' not needed.
NY times @RoniNYTimes did a story on it (nytimes.com/2021/03/14/hea…).
I *really* wanted this paper to be convincing. It would help so many children to be able to return to school. But...
NY times @RoniNYTimes did a story on it (nytimes.com/2021/03/14/hea…).
I *really* wanted this paper to be convincing. It would help so many children to be able to return to school. But...
There are some really big issues:
1) Authors implicitly define "safe enough" to mean: if incidence isn't statistically significantly higher in school districts w/ 3'+ rule than 6'+ then no need for 6'+. But a lack of a significant difference can arise from many things. @bolkerb
1) Authors implicitly define "safe enough" to mean: if incidence isn't statistically significantly higher in school districts w/ 3'+ rule than 6'+ then no need for 6'+. But a lack of a significant difference can arise from many things. @bolkerb
Biggest issue is lots of "noise" in data can lead to no "significant" effect even if one exists. How big is that issue here? Big.
Instead of asking if diff is significant, one can simply look at key estimated effect. Incidence in 6'+ districts was 0.789 (0.528-1.179) that in 3'+.
Instead of asking if diff is significant, one can simply look at key estimated effect. Incidence in 6'+ districts was 0.789 (0.528-1.179) that in 3'+.
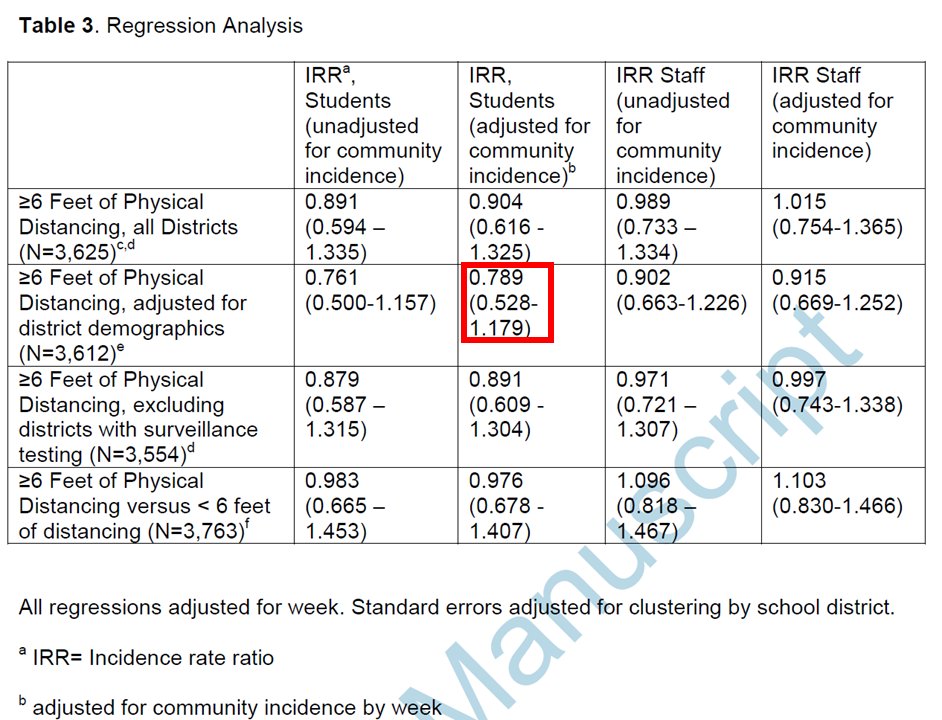
What does that mean? It means incidence was estimated to be 21% lower in districts w/ 6'+ rule than 3'+ rule. This difference wasn't "significant" b/c the uncertainty in the estimate was big. In fact, data suggests incidence ratio could be 47% lower to 18% higher (95% CI limits).
In other words, 6' might make schools MUCH safer than 3'-incidence might be twice as high!- or it might make no difference at all (or paradoxically, slightly riskier). Data are too noisy for us to be confident in comparison. Analyses also have many issues (too technical for twit)
Big issue #2) Focal metric in study is incidence (# of COVID-19 cases reported to state). That's not what we actually care about. We care about # of transmission events in class rooms that have 3' or 6' of space b/w students. Study has 0 data on where infections occurred. 
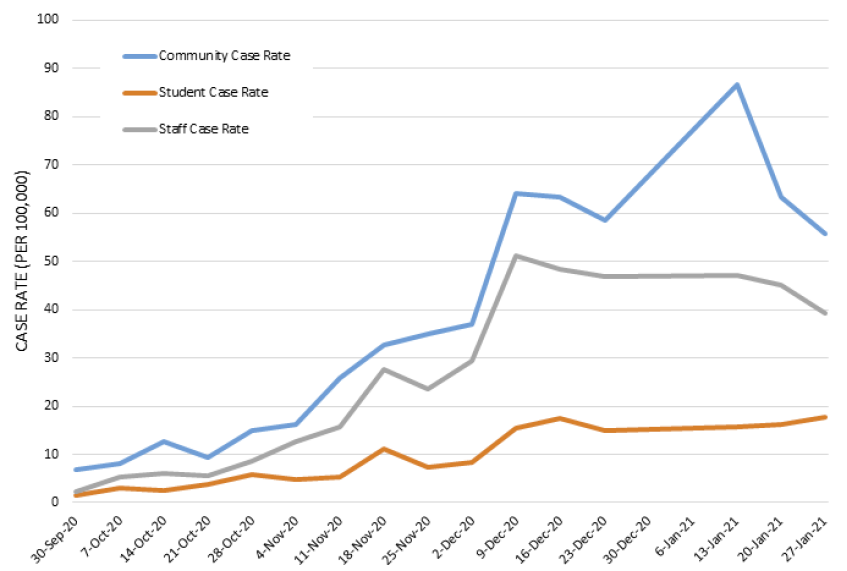
Incidence in staff are highly correlated w/ community incidence; incidence in students is more weakly correlated w/ comm. incid. Strangely, both flatten as community incidence spikes. More precautions? Closures?
Overall, can't tell how much transmission at school.
Overall, can't tell how much transmission at school.
Many other questions/issues
-Incidence is based on cases reported to state, which, presumably are mostly symptomatic cases. Cases in children are often mild & most are missed, so incidence is small fraction of infections. This omission adds noise to comparison.
-Incidence is based on cases reported to state, which, presumably are mostly symptomatic cases. Cases in children are often mild & most are missed, so incidence is small fraction of infections. This omission adds noise to comparison.
-Comparison is of school districts, not schools. Incidence is based on County level data, not from individual schools or districts.
-No data on actual distance (6',3') used; just school plans
-Schools were included even if attendance was extremely low (anything >5% was included).

-No data on actual distance (6',3') used; just school plans
-Schools were included even if attendance was extremely low (anything >5% was included).
Given these (& MANY other issues), what should we make of the results?
-If we want to get schools open at full capacity, ignore issues & use 3' & say it's supported by "peer reviewed science" (this paper is published). I'm certain many people/districts/states will do this.
-If we want to get schools open at full capacity, ignore issues & use 3' & say it's supported by "peer reviewed science" (this paper is published). I'm certain many people/districts/states will do this.
-If we want to actually know if risk/transmission is higher w/ 3' than 6', do a more careful study:
-Get data from case investigations
-Find out how many actual transmission events occurred at schools w/ 3' & 6'
-Analyze the data properly; look at effect sizes, not significance
-Get data from case investigations
-Find out how many actual transmission events occurred at schools w/ 3' & 6'
-Analyze the data properly; look at effect sizes, not significance
So, while I appreciate authors' attempts to address this VERY IMPORTANT issue, evidence in this study gives me essentially no confidence in boldly stated conclusions & makes me doubt authors' judgement & basic understanding of statistics. Study seems more propaganda than science.
This is despite me very much wanting to believe the conclusions of the paper.
I'll note that the conclusions may, in fact, be correct (i.e. 3' may be no more risky than 6'). But the evidence here simply doesn't measure up to a very basic level of scrutiny.
I'll note that the conclusions may, in fact, be correct (i.e. 3' may be no more risky than 6'). But the evidence here simply doesn't measure up to a very basic level of scrutiny.
Apparently Dr. Fauci found it more convincing than I did (but I doubt he's actually read the paper).
https://twitter.com/CNNSotu/status/1371150011073978372
Just for clarification, overall, evidence I've seen suggests that schools are relatively safe as long as key measures are in place (masks & ventilation being most important; distance helps too; hygiene less so). I'd open schools under most circumstances, including most of US now.
However, I wouldn't shrink 6' to 3' based on the evidence in this paper. I'd use 3' based on the overall levels of transmission seen in schools that have used masks & ventilation but couldn't do 6'.
In addition, I'd argue having in-person classes is worth some additional risk. But how much is too much? Difficult question. Paper suggests non-significant 10-20% higher risk (& CI includes 50% & -33%). Is that too much? Not to me but I'd want any decision made to reflect that.
• • •
Missing some Tweet in this thread? You can try to
force a refresh