
New study by @MHitchingsEpi et al shows that an inactivated vaccine CoronaVac is effective against COVID-19 in a setting of epidemic P.1 variant transmission in Brazil 🇧🇷. A thread. (1/n)
medrxiv.org/content/10.110…
medrxiv.org/content/10.110…
The authors conducted a matched test-negative case-control study to estimate the effectiveness of an
inactivated vaccine, CoronaVac, in healthcare workers in Manaus, where P.1 accounted for ~75% of the circulating virus.(2/n)
inactivated vaccine, CoronaVac, in healthcare workers in Manaus, where P.1 accounted for ~75% of the circulating virus.(2/n)

Vaccination with at least one dose was associated with an adjusted vaccine effectiveness of 49.6% (95% CI, 11.3 - 71.4) against symptomatic SARSCoV-2 infection >14 days after receiving the first dose. (3/n)
Estimated vaccine effectiveness of at least one dose against any SARS-CoV-2 infection (asymptomatic +symptomatic) was 35.1% (95% CI, -6.6 - 60.5) >14 days after receiving the first dose of CoronaVac (4/n).
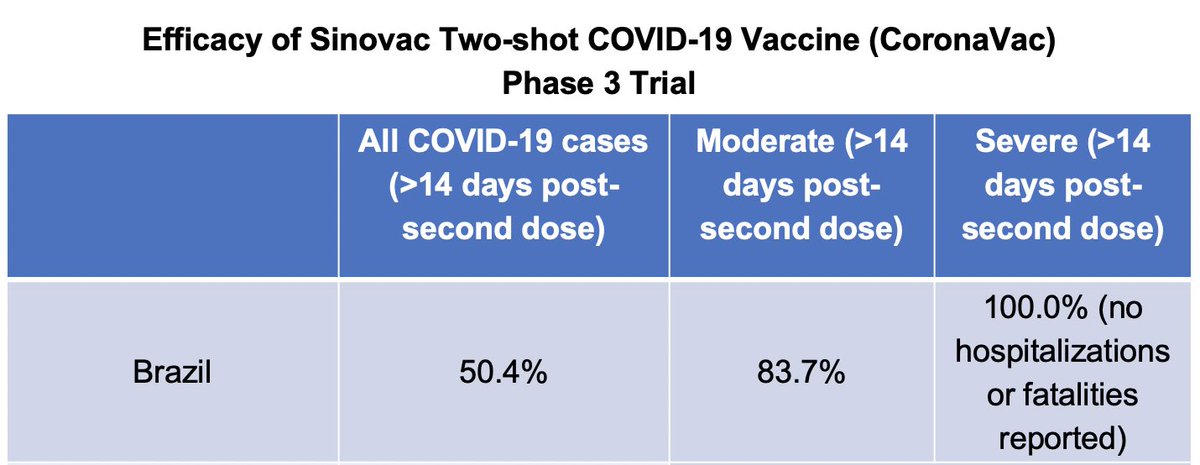
It is difficult to compare these real world effectiveness data (>14 days after at least 1 dose with 75% P.1) to the phase 3 trial efficacy data (only reporting >14 days after 2 doses, pre-P.1 emergence).
(Data courtesy of #SpikeSupport @YaleMed) (5/n)
(Data courtesy of #SpikeSupport @YaleMed) (5/n)
Good news is that Coronavac, even after one dose, is able to reduce symptomatic infection significantly in a region of Brazil where P.1 dominates. The devastation of the situation and the warning to the rest of the world is described here. (6/n)
scientificamerican.com/article/a-city…
scientificamerican.com/article/a-city…
Researchers from Brazil, @YaleSPH @YaleMed @juliocroda @datcummings @otavio_ranzani and international partners are continuing the study to evaluate the full 2 dose schedule. So much hard work went into this amidst the devastating COVID surge. These authors are truly heroic. (7/n)
These early findings provide good support to securing vaccine supply and ramping up vaccination. This needs to happen ASAP to combat the devastating crisis in Brazil - where P.1 has spread throughout the country. (End)
• • •
Missing some Tweet in this thread? You can try to
force a refresh









