Watch here tomorrow for the launch of a new accredited tweetorial on use of P2Y12 inhibitor monotherapy after PCI! Earn 0.5 CE/CME credits: physicians, nurses, pharmacists! Expert faculty @SVRaoMD. #medtwitter @academiccme #cardiotwitter
1) Welcome to a tweetorial on the use of P2Y12 inhibitor monotherapy after PCI! Accredited for 0.50 credits by @academiccme: physicians, nurses, pharmacists! I am @SVRaoMD. 
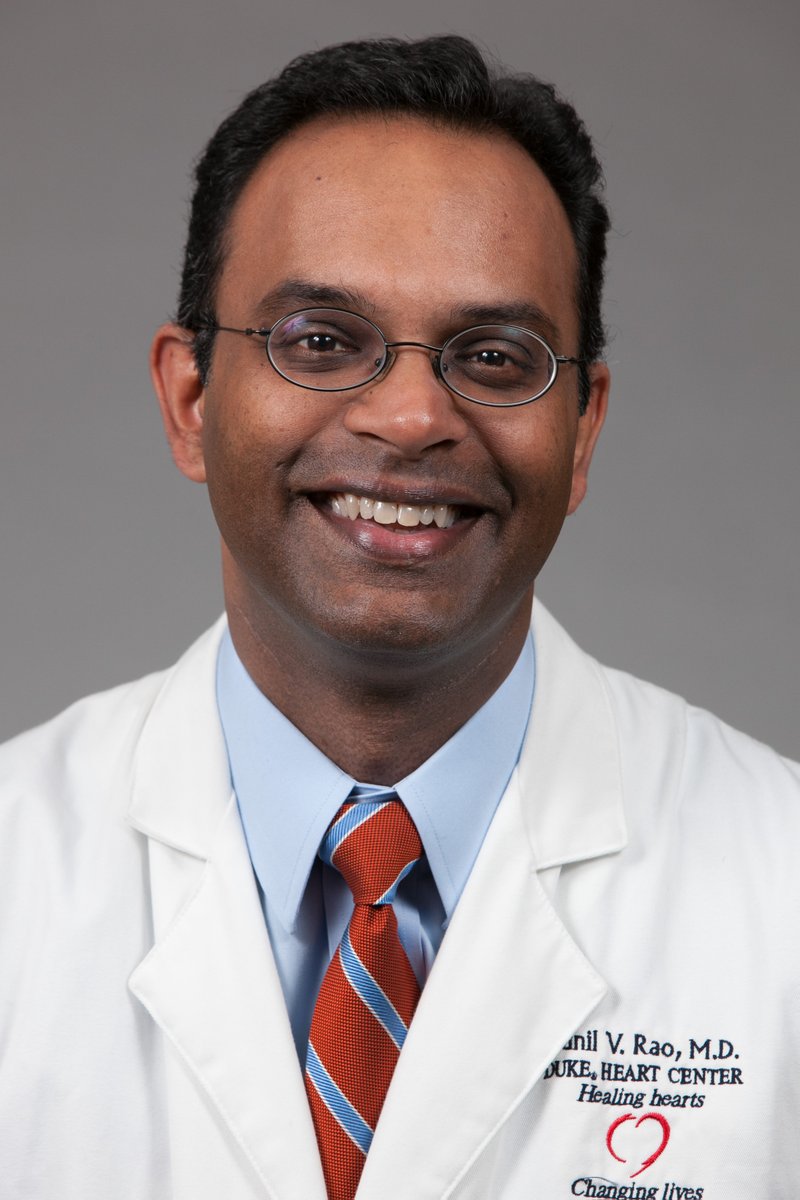
2) This series is supported by educational grant funding from Abbott, AstraZeneca, Bayer, Chiesi, and NovoNordisk. Follow this thread for credit. And here is a case …
3) 75 yo female presents to the emergency department with 3 days of stuttering angina that was persistent at rest today. PMHx significant for HTN, dyslipidemia, & Type 2 DM.
4) … Afebrile, HR: 105 bpm regular, BP: 185/90 mmHg, SpO2: 98%, Hs-TnI 592 ng/l, Cr 0.8 mg/dl, Hb 11 g/dl. ECG: NSR, non-specific T-wave changes in II, III, & aVF.
5) … The patient is admitted for NSTE-ACS. What is your initial antiplatelet strategy prior to diagnostic angiography?
6) This patient is at high risk for adverse outcomes and is loaded with ticagrelor, and while there is debate over “upstream” loading in NSTEMI, it was felt that her ischemic risk was high and pre-cath loading was an acceptable risk.
7) The PLATO trial (N Engl J Med 2009; 361:1045-1057), with upstream ticag loading, showed a 16% reduction in 1-year death, MI, or stroke with ASA + ticag vs. ASA+ Clopi. Non-CABG related major bleeding in PLATO was higher with ASA + ticag vs. ASA + Clopi (4.5% vs. 3.8%, p=0.03).
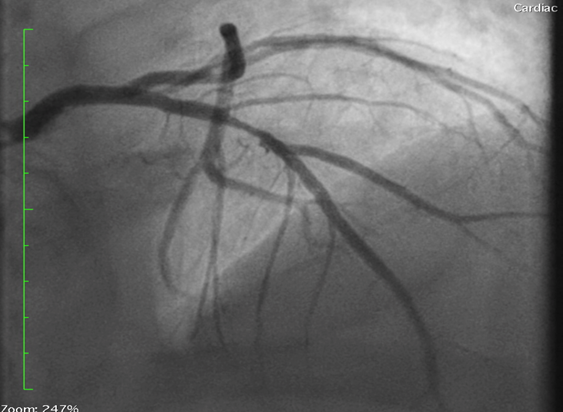
8) She undergoes #RadialFirst coronary angiography the next day. Is found to have an 80% lesion mid LAD, Angiographically non-significant disease in the LCx and RCA. Receives a 22 mm DES to mid LAD using IVUS guidance with a good result.
9) What is the minimum duration for #DAPT for this patient?
10) Provide your response and return tomorrow for more education! @ACCinTouch @SCAI @Drroxmehran @CMichaelGibson @DrMauricioCohen @DLBHATTMD @rajivxgulati @AJuradoRoman @Felipediezhoyo @sbrugaletta @foroic @gabrielsteg @SJGreene_md @MichaelGNanna @jaygirimd @mmamas1973
11) Welcome back! I am @SVRaoMD. Choice C is correct. ACC/AHA guidelines give a Class I recommendation to 12 mos of #DAPT for ACS pts who undergo PCI regardless of stent type. They also give a Class IIa to ticagrelor over clopidogrel.
12) Your patient recovers from DES placement and is discharged home on DAPT and GDMT for CAD. You see her in follow-up at one month.
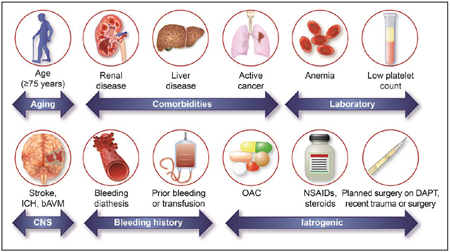
13) She has been active and feeling well. She wants to know whether she is at high risk for bleeding complications from DAPT. Based on the recent #ARC#HBR criteria (Urban P, et al. Circulation 2019), she has only one criterion for HBR (age): 
14) She is worried about the risks of bleeding with #DAPT and wants to know if she can stop either ASA or ticagrelor. She asks you what the data show with respect to antiplatelet monotherapy. There are several trials that have studied this issue.
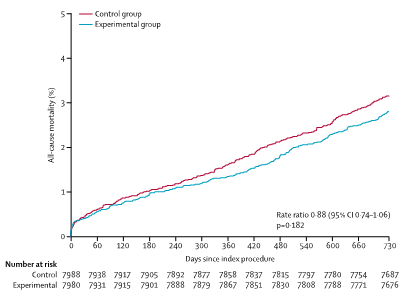
15) The #GLOBAL-LEADERS trial (DOI:doi.org/10.1016/S0140-…) studied ticag w/ ASA for 1m followed by ticag alone for 23m in 15,968 pts post PCI. Ticag alone was not superior to 12m of DAPT followed by 12m of ASA alone at preventing death or MI. But… 
16) The #STOPDAPT-2 trial (doi:10.1001/jama.2019.8145) that studied 1m #DAPT followed by clopidogrel monotherapy vs. 12m #DAPT in 3,045 pts who underwent #PCI showed noninferiority and superiority for net adverse clinical events (ischemia + bleeding) compared with 12m #DAPT. 
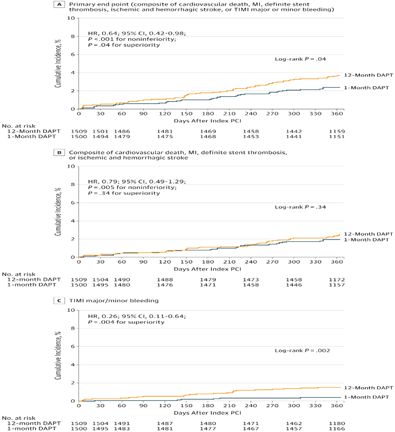
17) The #SMART-CHOICE trial (doi:10.1001/jama.2019.8146) randomized 2993 pts who underwent PCI to P2Y12 inhibitor monotherapy after 3m of DAPT vs. 12 m of DAPT. P2Y12 mono was non-inferior with respect to death/MI/stroke compared with 12m DAPT. Bleeding was lower with monotherapy
18) The #TICO trial (doi:10.1001/jama.2020.7580) randomized 3056 pts ACS who underwent PCI w/DES to ticag monotherapy after 3m of DAPT vs. 12 m DAPT. Ticag monoRx reduced 1y net adverse events, driven by a 44% reduction in major bleeding
19) Finally the #TWILIGHT trial (DOI: 10.1056/NEJMoa1908419) led by @Drroxmehran randomized 7119 high-risk pts undergoing PCI to ticagrelor monotherapy after 3m of DAPT vs. 12 m DAPT. Ticag monoRx resulted in less bleeding and similar rates of ischemic events.
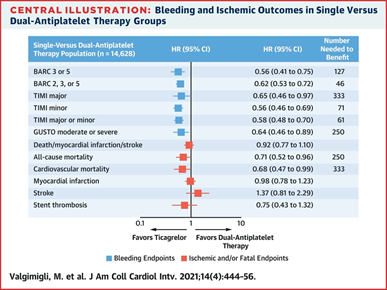
20) The #SIDNEY meta-analysis (J Am Coll Cardiol Intv. 2021 Feb, 14 (4) 444–456) combined #GLASSY (doi: 10.1016/j.jacc.2019.08.1038.) and #TWILIGHT trials for combined dataset of 14628 pts: 
21) Based on the available randomized trials, you can counsel the pt that which of the following strategies will reduce bleed risk without compromising ischemic benefit?
a)ASA+Ticag for 12m
b)ASA+Clopidogrel for 12m
c)Stop ASA at 3m, continue ticag
d)ASA+Prasugrel for 12m
a)ASA+Ticag for 12m
b)ASA+Clopidogrel for 12m
c)Stop ASA at 3m, continue ticag
d)ASA+Prasugrel for 12m
22) Answer the poll and return tomorrow to claim your free CE credit! #medtwittter #cardiotwitter @djc795 @cpgale3 @esbrilakis @JSillerMatula @thiele_holger @mirvatalasnag @pabeda1 @hect2701 @PerwaizMeraj @mwkrucoff @duanepinto @rcstoler @vass_vassiliou @ESC_Lavinia @JGrapsa
• • •
Missing some Tweet in this thread? You can try to
force a refresh