#FOAMrad #neurorad #radres #radmed #HUNSC #daybydaycases #radiology #MedEd
One patient/two sides……and two pathologies.
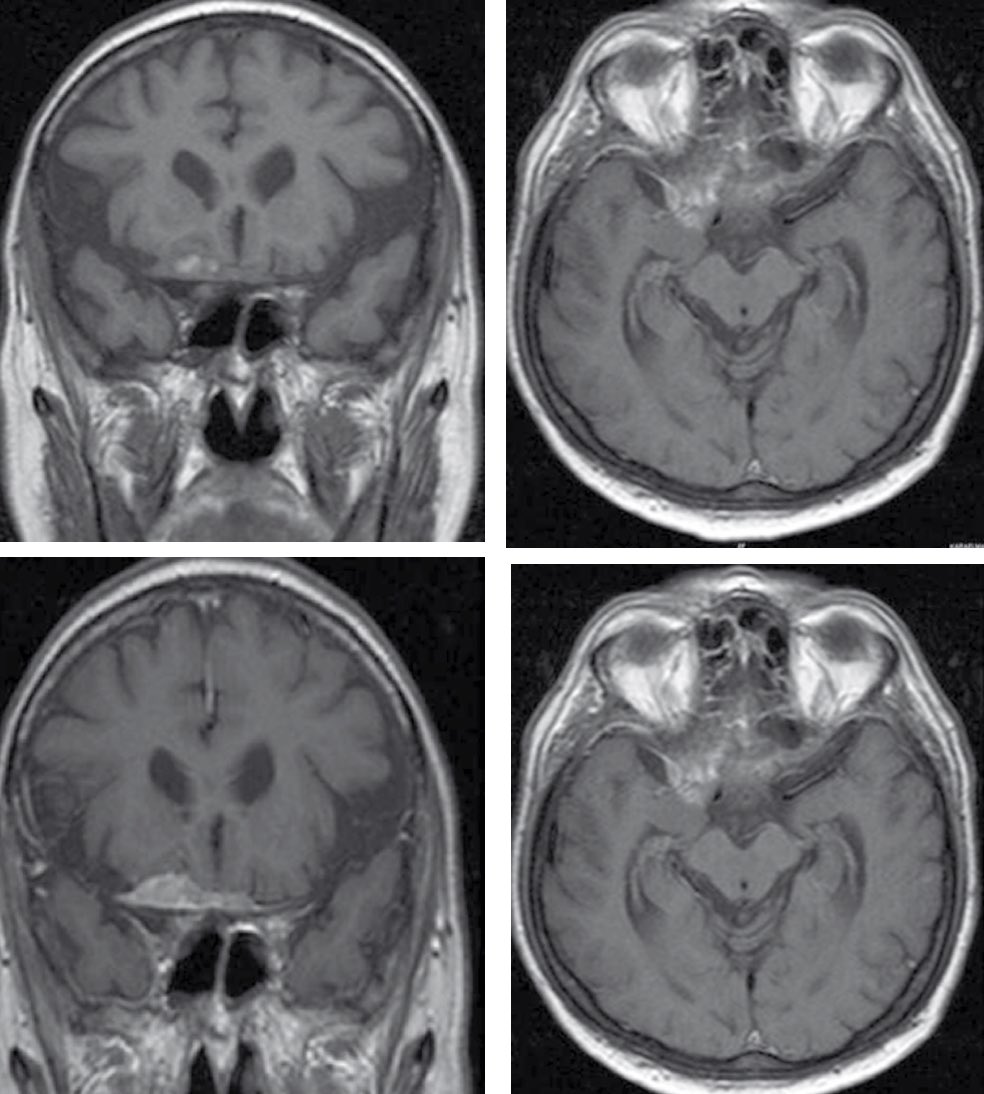
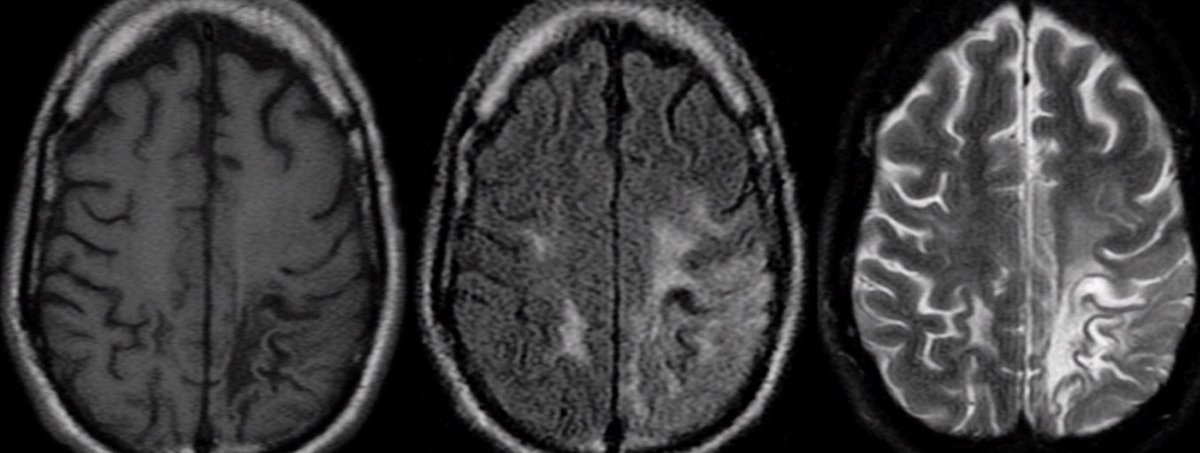
From left to right axial FLAIR, coronal T2 and axial T1 MRI
One patient/two sides……and two pathologies.
From left to right axial FLAIR, coronal T2 and axial T1 MRI
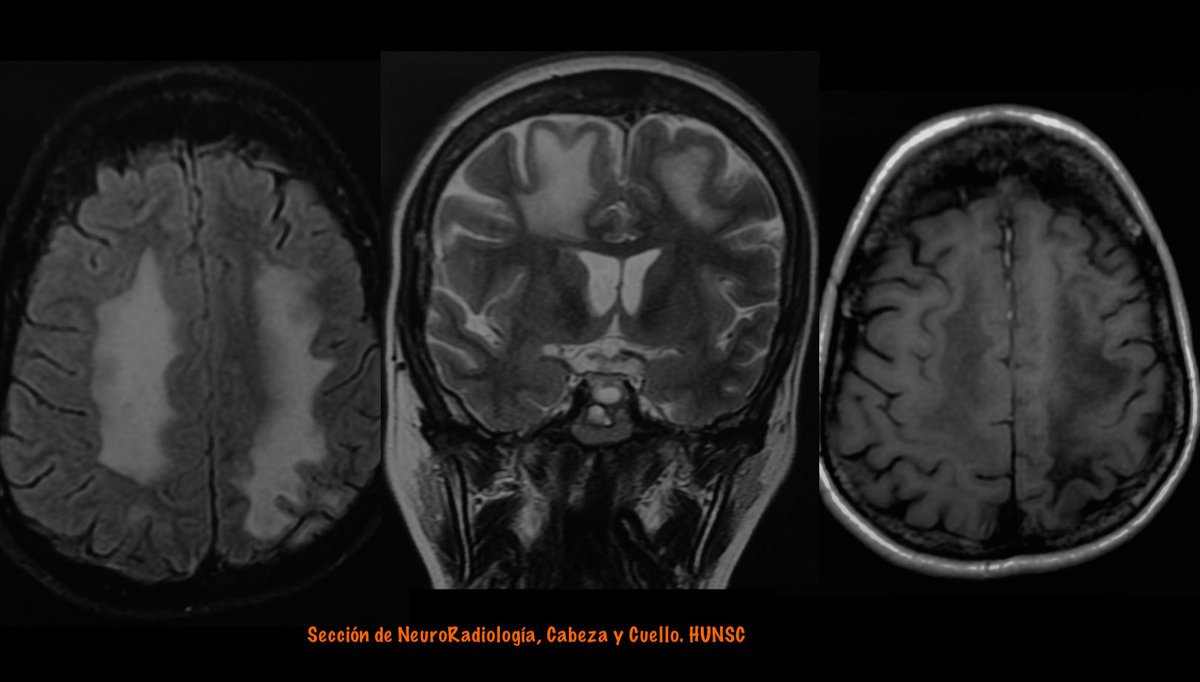
Right side:
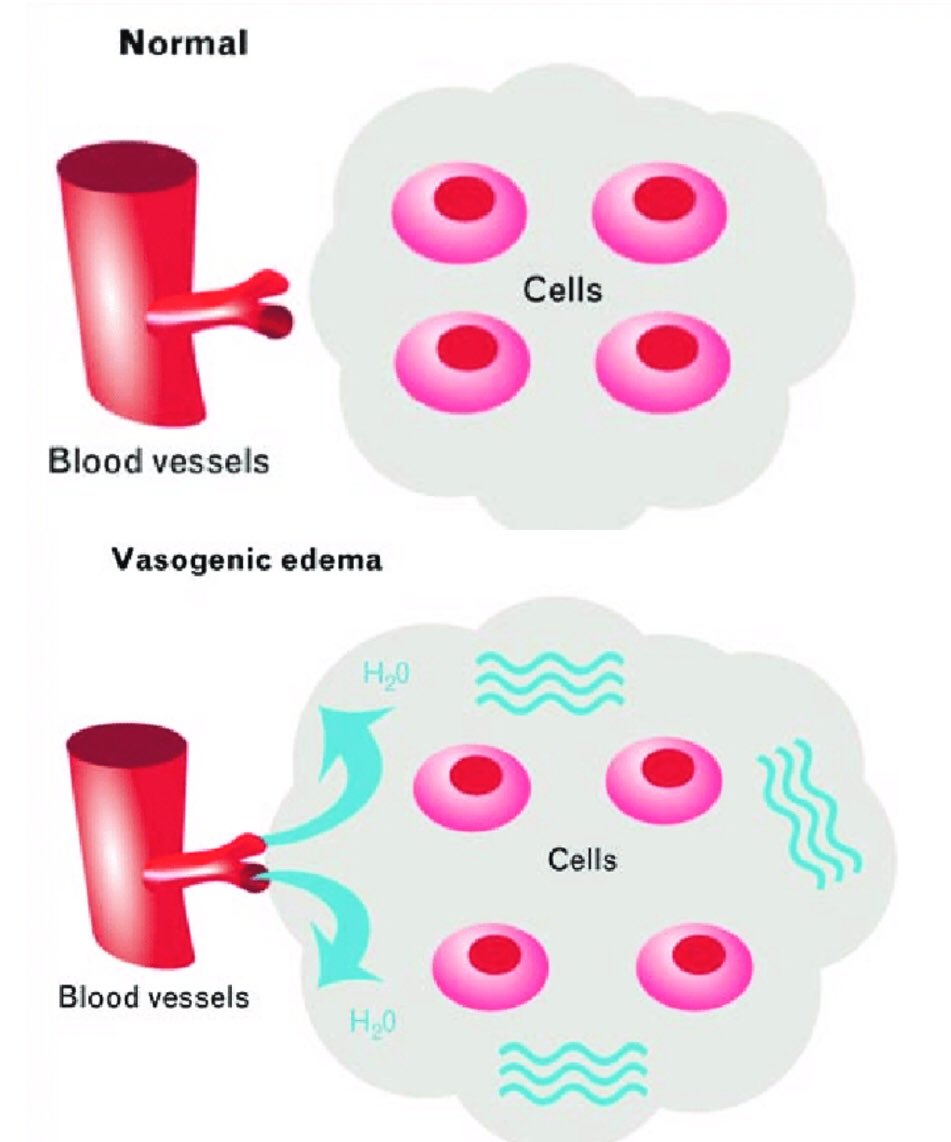
Parasagital meningioma with vasogenic edema
From left to right: coronal T2, enhanced T1 and DWI.
Parasagital meningioma with vasogenic edema
From left to right: coronal T2, enhanced T1 and DWI.

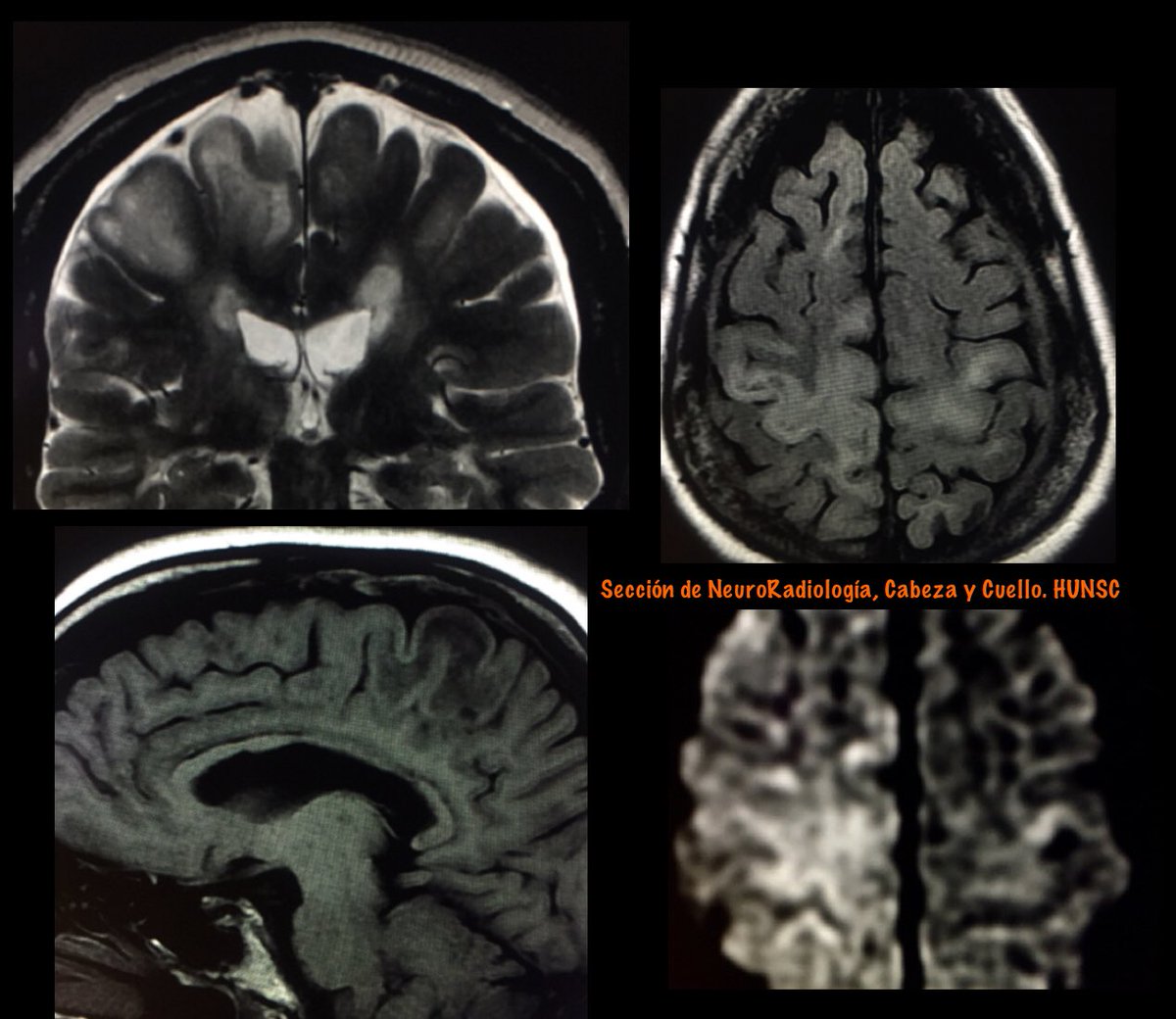
Left side :
Progressive Multifocal Leukoencephalopathy (PML)
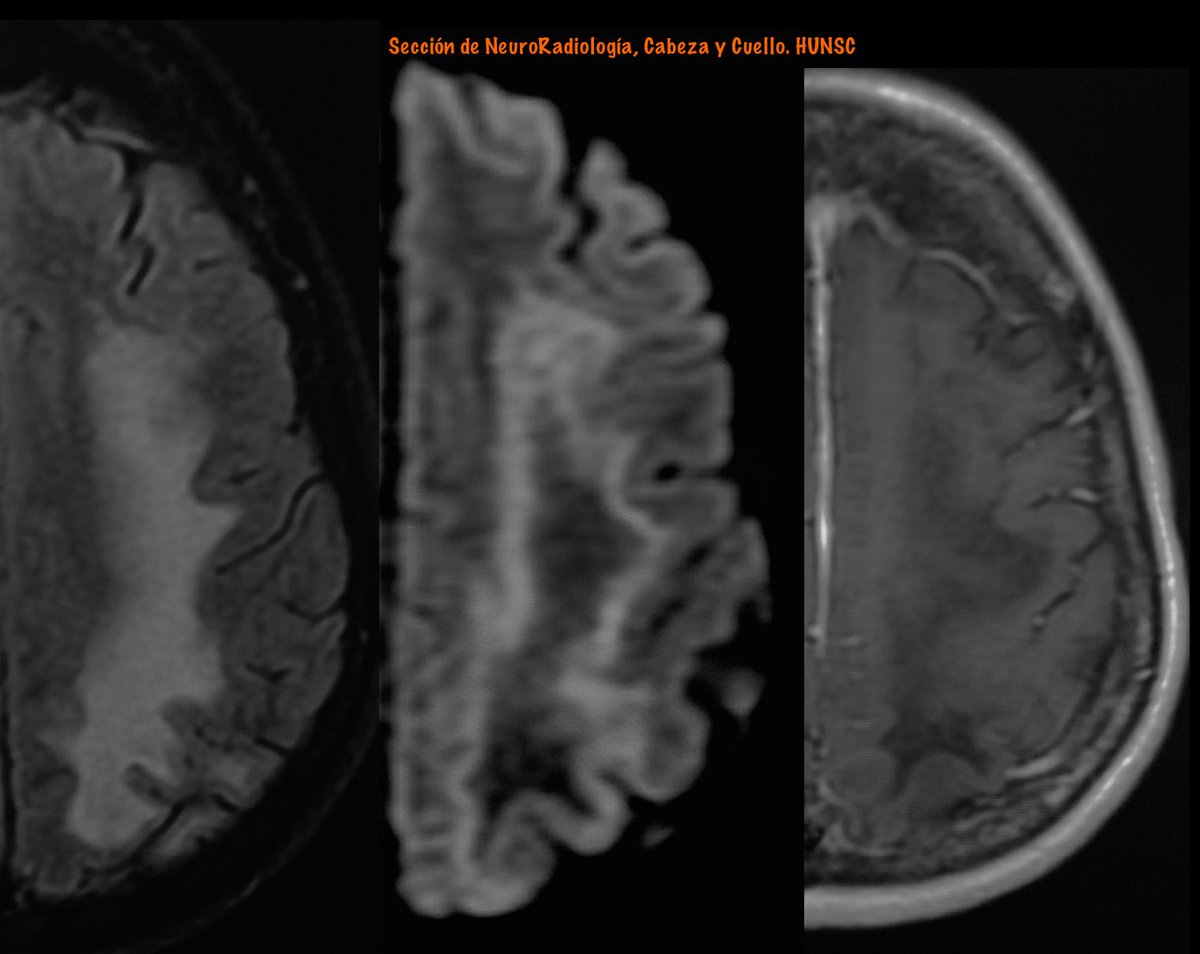
From Left: FLAIR, DWI and enhanced T1 MRI
Progressive Multifocal Leukoencephalopathy (PML)
From Left: FLAIR, DWI and enhanced T1 MRI

Diffusion Imaging In PML:
The appearance on DWI varies according to the disease stage.
In new active lesions, there is a rim of diffusion restriction at the advancing edge and a central core of facIlitated diffusion.
The rim is usually incomplete and signifies active infection.

The appearance on DWI varies according to the disease stage.
In new active lesions, there is a rim of diffusion restriction at the advancing edge and a central core of facIlitated diffusion.
The rim is usually incomplete and signifies active infection.
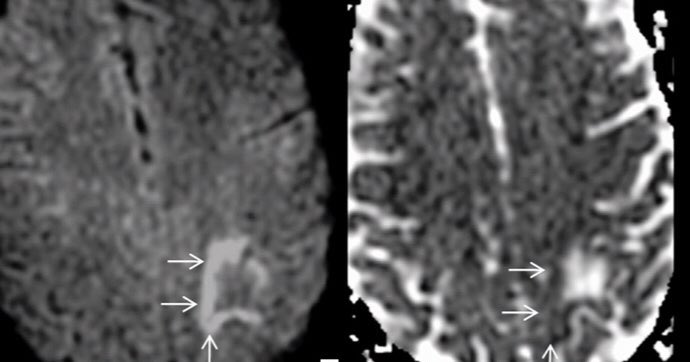
Histopathologically, this advancing edge correlates with large swollen oligodendrocytes, enlarged “bizarre astrocytes” with numerous large processes, and infiltration of foamy macrophages. This cellular enlargement constricts the extracellular space. 

AJNR 2010
DOI 10.3174/ajnr.A2035
10.1594/ecr2015/B-0300
Neurology 2016;86;1516-1523
DOI 10.1212/WNL.0000000000002586
AJNR 2015
dx.doi.org/10.3174/ajnr.A…
Curr Opin Neurol 2014, 27:260–270
DOI:10.1097/WCO.0000000000000099
DOI 10.3174/ajnr.A2035
10.1594/ecr2015/B-0300
Neurology 2016;86;1516-1523
DOI 10.1212/WNL.0000000000002586
AJNR 2015
dx.doi.org/10.3174/ajnr.A…
Curr Opin Neurol 2014, 27:260–270
DOI:10.1097/WCO.0000000000000099
https://twitter.com/vmargar/status/1139417172587896832?s=10
• • •
Missing some Tweet in this thread? You can try to
force a refresh