Empezando charla + preguntas en 2 horas (5 pm España; 12 Argentina; 11 Chile; 10 Mexico DF - otros: time.is)
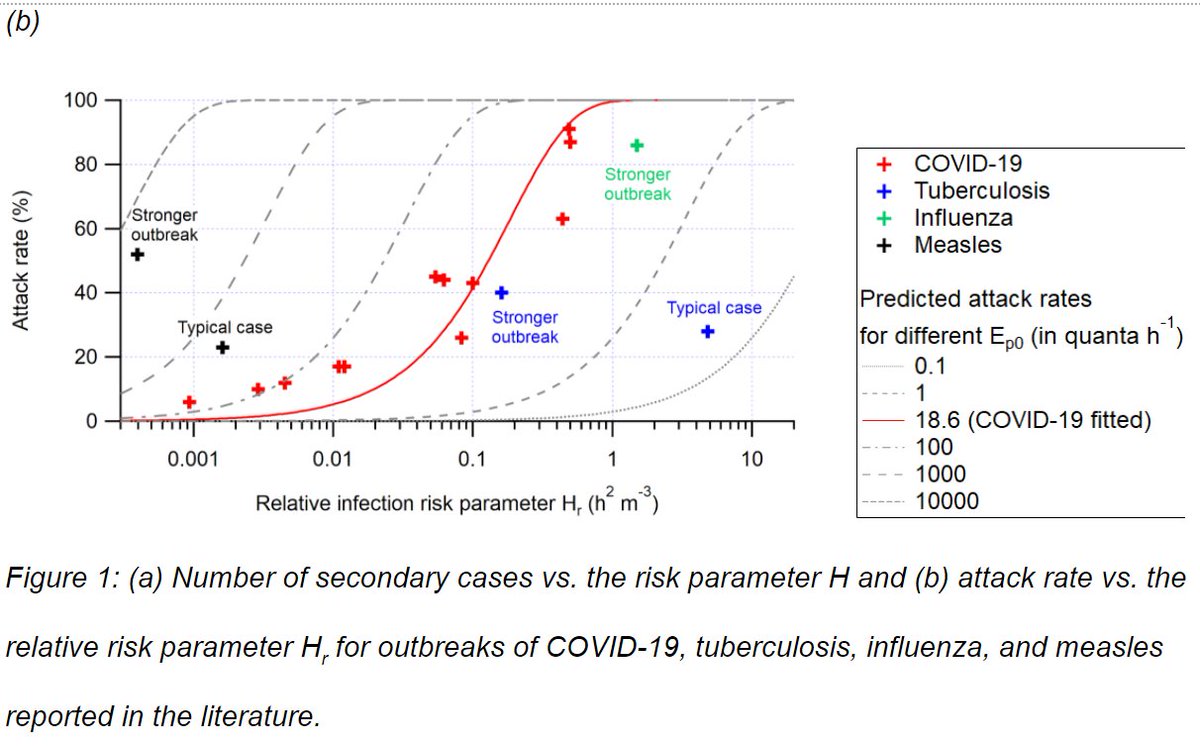
"Métodos prácticos para estimar y monitorear el riesgo de contagio de COVID-19 cuando se comparte aire en interiores"
Registro: bit.ly/aireamoswebinar
"Métodos prácticos para estimar y monitorear el riesgo de contagio de COVID-19 cuando se comparte aire en interiores"
Registro: bit.ly/aireamoswebinar
https://twitter.com/aireamos/status/1389865436624326659
El video de la charla de hoy (30 min + 1 hr de preguntas) sobre "Métodos prácticos para estimar y monitorear el riesgo de contagio de COVID-19 cuando se comparte aire en interiores" se puede ver en YouTube:
- Diapositivas webinar de hoy "Métodos prácticos para estimar y monitorear el riesgo de contagio de COVID-19 cuando se comparte aire en interiores": drive.google.com/file/d/1BNX28I…
- Diapositivas mas generales: Bit.ly/COVID-aerosols2
- Estimador de contagio: tinyurl.com/covid-estimator
- Diapositivas mas generales: Bit.ly/COVID-aerosols2
- Estimador de contagio: tinyurl.com/covid-estimator
- Preguntas frecuentes: tinyurl.com/preguntas-espa…
• • •
Missing some Tweet in this thread? You can try to
force a refresh