
1/ A SIMPLE WAY TO ESTIMATE THE RISK OF INDOOR SUPERSPREADING
Our preprint using the airborne transmission model
Captures the literature outbreaks well. So we can use it to see whether an activity is at risk of superspreading
Also to compare diseases
medrxiv.org/content/10.110…
Our preprint using the airborne transmission model
Captures the literature outbreaks well. So we can use it to see whether an activity is at risk of superspreading
Also to compare diseases
medrxiv.org/content/10.110…
2/ It can be very confusing to estimate how risky different activities are, depending of size of space, duration, number of people, vocalization, intensity of breathing, ventilation, air cleaning, masks + their quality + fit.
We combine it all into a single parameter, rigorously
We combine it all into a single parameter, rigorously
3/ We'll explain the parameter(s) later, but first let me convince you that it works.
The key is Fig. 1 b:
- X-axis is risk parameter in log. scale. MUCH riskier to right, MUCH less risky to left
- Y-axis is attack rate (% of people present infected in outbreaks)

The key is Fig. 1 b:
- X-axis is risk parameter in log. scale. MUCH riskier to right, MUCH less risky to left
- Y-axis is attack rate (% of people present infected in outbreaks)

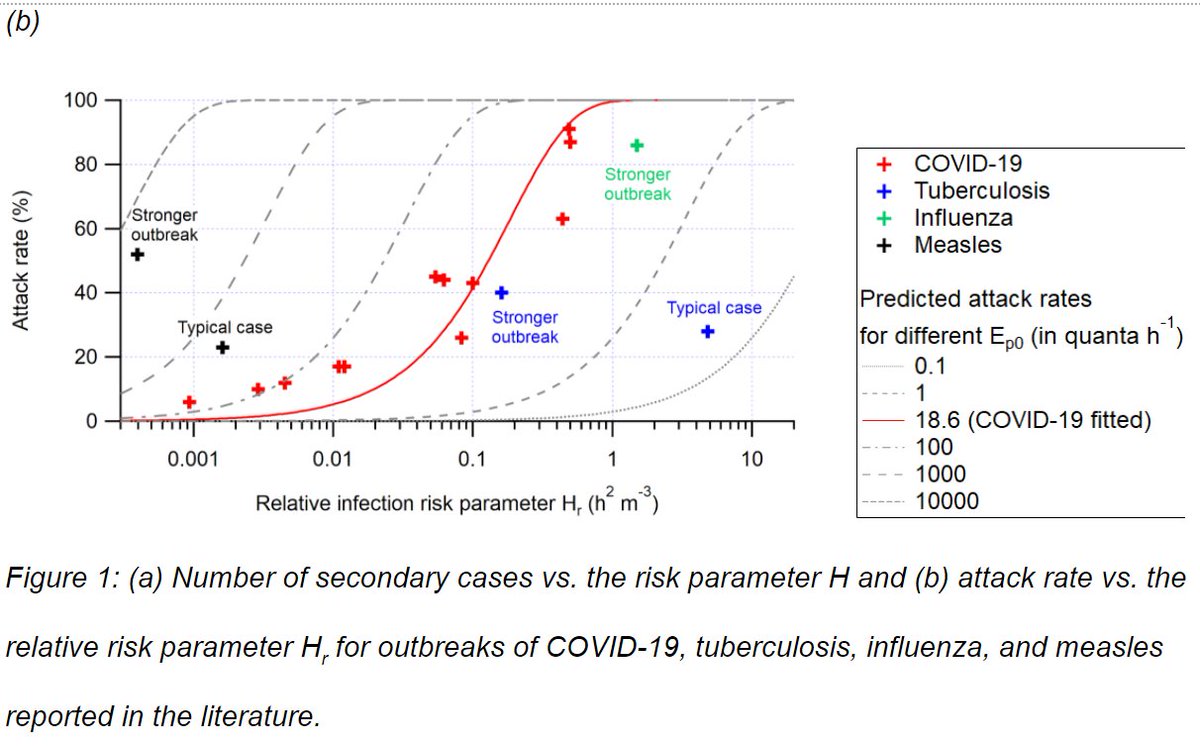
4/ Red points are COVID-19 outbreaks from the literature (e.g. Skagit choir, Berlin choir, Chinese restaurant and buses, in aircraft, slaughterhouse, schools etc.)
Red line is airborne transmission model.
The points follow the model ==> OUTBREAKS DOMINATED BY AIRBORNE
Red line is airborne transmission model.
The points follow the model ==> OUTBREAKS DOMINATED BY AIRBORNE

5/ If the outbreaks were dominated by fomites or large droplets, they would vary in different ways. No reason why they would correlated with airborne risk.
We used all the outbreaks we could find that had all the needed info. Ventilation and room size rarely reported!
We used all the outbreaks we could find that had all the needed info. Ventilation and room size rarely reported!

6/ At low values of the risk parameter Hr, the outbreaks tend to be above the model.
Most likely because we are only detecting the outlier events, otherwise we just wouldn't see them. Still they follow well.
Most likely because we are only detecting the outlier events, otherwise we just wouldn't see them. Still they follow well.

7/ Interestingly, there are a few outbreaks for measles (black), tuberculosis (blue) that can be added to the graph. Both airborne. COVID-19 clearly MORE TRANSMISSIBLE than TB and less than measles.
COVID-19 FITS WELL AMONG AIRBORNE DISEASES.
COVID-19 FITS WELL AMONG AIRBORNE DISEASES.

8/ Hopefully this will help stop the nonsense that COVID-19 can't be airborne because it is less contagious than measles.
It is. And it is more contagious than TB, which can ONLY transmit through airborne. Although strong TB outbreak can be similar to COVID-19.
It is. And it is more contagious than TB, which can ONLY transmit through airborne. Although strong TB outbreak can be similar to COVID-19.

9/ Also of interest: we added the Moser et al. (1979) influenza outbreak: in an airplane, 3 hrs stuck in tarmac w/o any ventilation, person coughing constantly.
A little less transmissible than COVID-19 in that case.
A little less transmissible than COVID-19 in that case.

10/ We see that when Hr < 0.001 h2 m-3, we don't see outbreaks. Therefore we should keep activities below that value during the pandemic. 

11/ This allows us to combine volume of space, duration, number of people, vocalization, intensity of breathing, ventilation, air cleaning, masks + their quality + fit rationally and quantitatively to estimate the risk of a situation. 

12/ If you want to calculate the risk parameter for your situation, you can do so with the COVID-19 Aerosol Transmission Estimator, freely available online.
(Modify sheet "Master-choir" -- will transplant to the others)
tinyurl.com/covid-estimator
(Modify sheet "Master-choir" -- will transplant to the others)
tinyurl.com/covid-estimator

13/ We also provide a quantitative version of the Table from Jones et al. BMJ (2020).
The table that they provided (below) was qualitative, and there was some debate about some of its corners.
bmj.com/content/370/bm…
The table that they provided (below) was qualitative, and there was some debate about some of its corners.
bmj.com/content/370/bm…
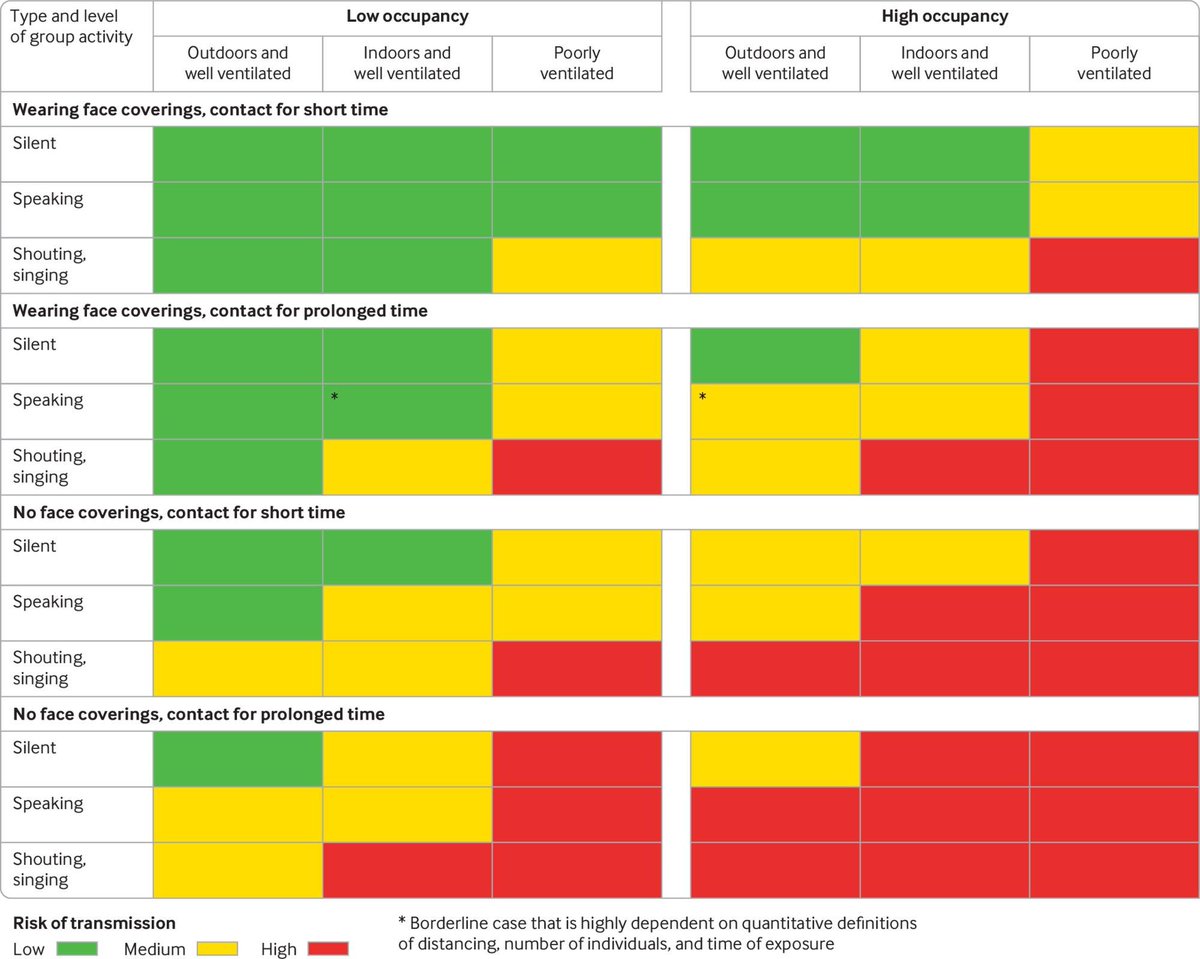
14/ We now provide a quantitative version of the table. We worked in collaboration with @trishgreenhalgh (@UniofOxford) and Lydia Bourouiba (@MIT) to update it.
Table in the paper is below. Parameters used shown in the Supp. Info. of the paper.
Table in the paper is below. Parameters used shown in the Supp. Info. of the paper.

15/ In addition, we provide an interactive table in the COVID-19 Aerosol Transmission Estimator (tinyurl.com/covid-estimator), so that people can modify the table for conditions of their interest (sheet "Risk Table") 

16/ We also show the effect of different mitigations of common activities (school, restaurant, choir)...
We see that the risk of superspreading is strongly reduced with mitigations. Big outbreaks needed to have several problems: low ventilation, strong vocalization, no masks...
We see that the risk of superspreading is strongly reduced with mitigations. Big outbreaks needed to have several problems: low ventilation, strong vocalization, no masks...
17/ But now we can finally quantify when mitigations are ENOUGH (or not enough, or perhaps too much).
Hard to make choirs safe, require A LOT of mitigations. But easy for a library (quiet) and not too difficult for a school.
Hard to make choirs safe, require A LOT of mitigations. But easy for a library (quiet) and not too difficult for a school.

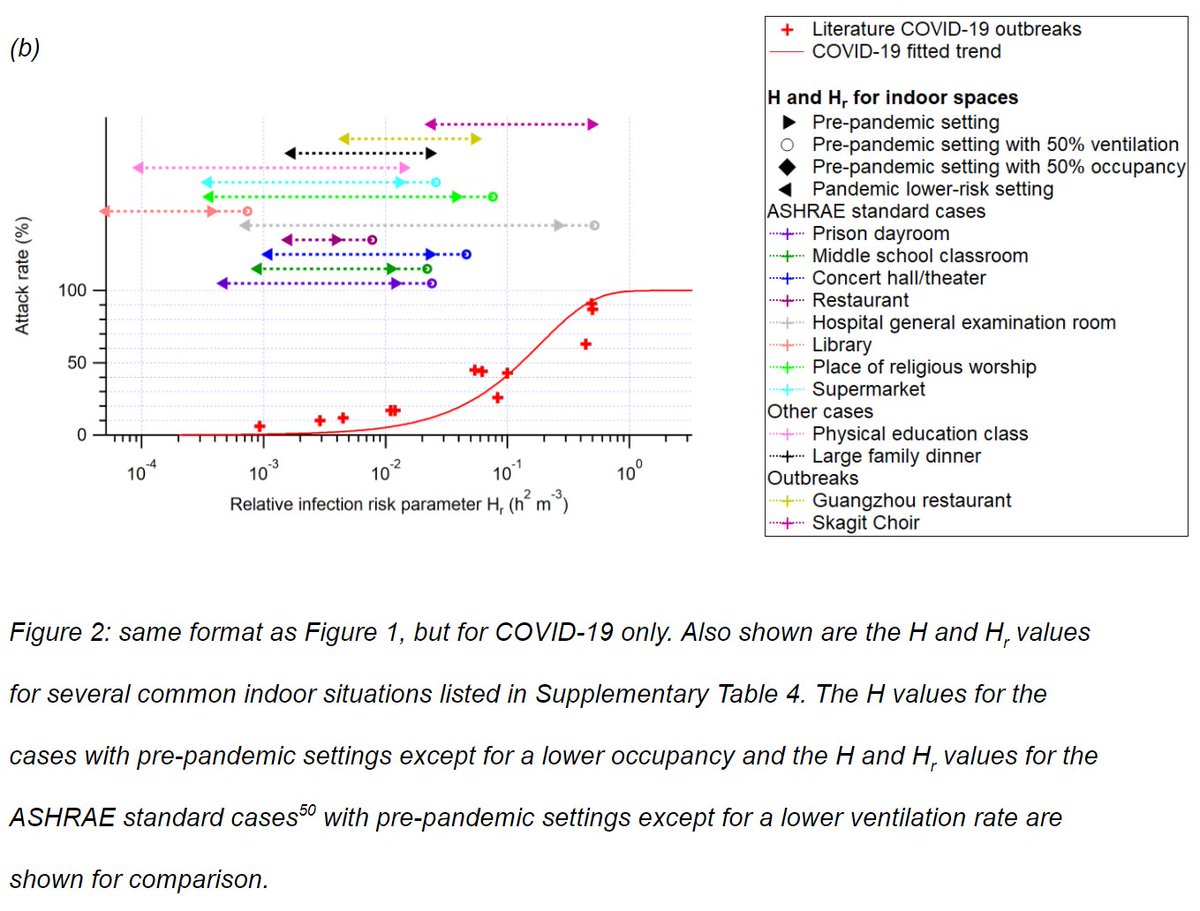
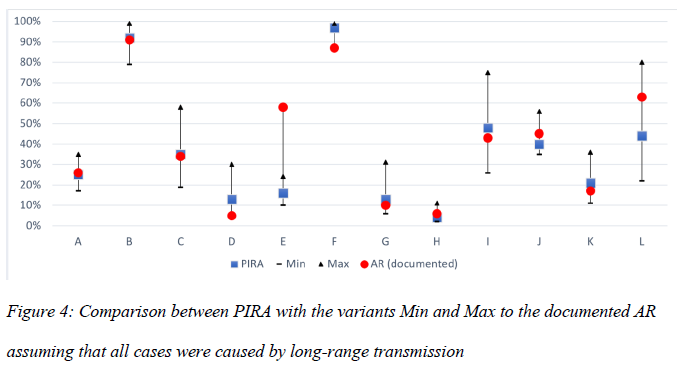
18/ There is related work in the literature, such as a preprint by @KriegelMartin of Germany (we use data for several of the outbreaks he reports).
Also shows that airborne model works (graph below). Does not derive a simple combined parameter.
medrxiv.org/content/10.110…
Also shows that airborne model works (graph below). Does not derive a simple combined parameter.
medrxiv.org/content/10.110…
19/ Also work by Bazant and Bush from MIT: pnas.org/content/118/17…
They calibrate a similar model to some outbreaks. Then express guideline as time, vs other parameters.
They calibrate a similar model to some outbreaks. Then express guideline as time, vs other parameters.

20/ If there are other papers I've missed that do similar things, please send them may way. Along with any suggestions, any mistakes you may find etc.
21/ Most important is that epidemiological reports should ALWAYS INCLUDE SIZE OF SPACE AND VENTILATION RATE.
Ventilation rate is easy to measure with a $200 CO2 meter, see here:
medium.com/@jjose_19945/h…
Ventilation rate is easy to measure with a $200 CO2 meter, see here:
medium.com/@jjose_19945/h…
22/ But yet with thousands of COVID-19 outbreaks that have been documented, and many investigated, not so many report ventilation rate and size of space, which are critical
I emailed authors of papers on several outbreaks, offered to help them measure ventilation. No one replied
I emailed authors of papers on several outbreaks, offered to help them measure ventilation. No one replied
23/ This work was an outgrowth of what I have learned working with the "Group of 36 Scientists" that Lidia Morawska assembled right after this enormous, historical error from @WHO :
https://twitter.com/who/status/1243972193169616898?lang=en
24/ We talked to @WHO, they didn't listen. But we've kept working on many papers (e.g. "letter of 239 scientists" last July: academic.oup.com/cid/article/71…)
25/ This paper on " How can airborne transmission of COVID-19 indoors be minimised?"
[TL-DR: ventilation, air cleaning with filters, air cleaning with UV in some cases. AVOID ionizers (and plasmas, photocatalysis, hydroxils) and foggers & ozonizers]
sciencedirect.com/science/articl…
[TL-DR: ventilation, air cleaning with filters, air cleaning with UV in some cases. AVOID ionizers (and plasmas, photocatalysis, hydroxils) and foggers & ozonizers]
sciencedirect.com/science/articl…
26/ This paper in @jhieditor Journal of Hospital Infection on "Dismantling myths on the airborne transmission of severe acute respiratory syndrome coronavirus (SARS-CoV-2)"
doi.org/10.1016/j.jhin…
doi.org/10.1016/j.jhin…

27/ This paper on the history of droplets and aerosols, and the origin of the ERROR of using 5 microns as the aerosol / droplet boundary, instead of the correct 100 microns.
[TDLR: someone confused deep penetration in lung for TB, with falling to ground]
papers.ssrn.com/sol3/papers.cf…
[TDLR: someone confused deep penetration in lung for TB, with falling to ground]
papers.ssrn.com/sol3/papers.cf…
28/ This paper in @TheLancet "Ten scientific reasons in support of airborne transmission of SARS-CoV-2" (thelancet.com/journals/lance…)
I was the only author from the group of 36 in this paper, but it contained much I learned from the group.
I was the only author from the group of 36 in this paper, but it contained much I learned from the group.
29/ The paper on the Skagit Choir outbreak, led by @ShellyMBoulder.
The clearest airborne transmission case of the early pandemic IMHO, and what set me on the hunt for simple ways to express infection risk, led to preprint that's focus of this thread.
doi.org/10.1111/ina.12…
The clearest airborne transmission case of the early pandemic IMHO, and what set me on the hunt for simple ways to express infection risk, led to preprint that's focus of this thread.
doi.org/10.1111/ina.12…
30/ The paper w/ @ZheP_AtmChem on using CO2 to estimate risks of indoor spaces.
Simpler to use for surveillance in the real world. But less accurate than the risk parameter here. Both use the same model
Can also calculate CO2 w/ tinyurl.com/covid-estimator
pubs.acs.org/doi/10.1021/ac…
Simpler to use for surveillance in the real world. But less accurate than the risk parameter here. Both use the same model
Can also calculate CO2 w/ tinyurl.com/covid-estimator
pubs.acs.org/doi/10.1021/ac…
31/ This latest preprint on the simple estimation or risk also has @ZheP_AtmChem as the first author. Zhe is a remarkable scientist, and was able to push this project fast and address all the tricky details.
medrxiv.org/content/10.110…
medrxiv.org/content/10.110…
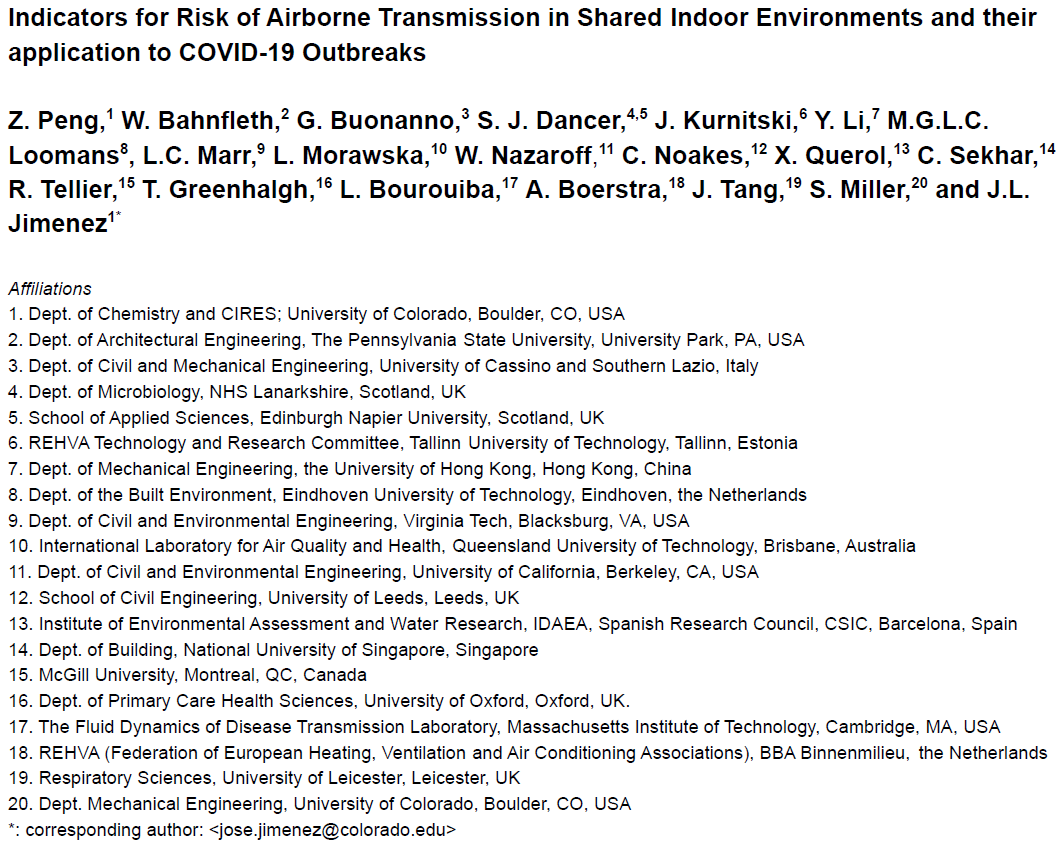
32/ Other authors, all members of the "group of 36 scientists" include @WBahnfleth @linseymarr @CathNoakes @xqcgeo @trishgreenhalgh @Atze_Boerstra @ShellyMBoulder + more not on Twitter (see pic) including Lidia Morawska, Julian Tang, Raymond Tellier, L. Bourouiba, S. Dancer... 
33/ Forgot to clarify at the start that this model is for airborne transmission in shared room air. So we assume that the distance is kept, so that short-range airborne transmission (sciencedirect.com/science/articl…) is not important
If distance not kept, risk is higher than we calculate
If distance not kept, risk is higher than we calculate
34/ Easier to read version:
Also one mistake, Trish G. and Lydia B. are not part of original group of 36, but we have collaborated on this and other projects.
https://twitter.com/threadreaderapp/status/1388974476226928642?s=19
Also one mistake, Trish G. and Lydia B. are not part of original group of 36, but we have collaborated on this and other projects.
• • •
Missing some Tweet in this thread? You can try to
force a refresh





