How does increasing dietary potassium improve blood pressure?
I’ve heard this, even recommended it. But how does this really work? Grab some prunes and follow along this Tuesday morning tweetorial.
#Nephtwitter #cardstwitter @MedTweetorials
I’ve heard this, even recommended it. But how does this really work? Grab some prunes and follow along this Tuesday morning tweetorial.
#Nephtwitter #cardstwitter @MedTweetorials
Let’s establish that potassium does appear to have an inverse relationship with BP
In a meta-analysis of 22 RCTs ⬆️ K+ intake⬇️BP by an average of 5.3/3.1 mmHg
💥greatest benefit seen in hypertensive patients who ⬆️potassium intake to 90-120mEq/d
👉pubmed.ncbi.nlm.nih.gov/23558164/
In a meta-analysis of 22 RCTs ⬆️ K+ intake⬇️BP by an average of 5.3/3.1 mmHg
💥greatest benefit seen in hypertensive patients who ⬆️potassium intake to 90-120mEq/d
👉pubmed.ncbi.nlm.nih.gov/23558164/
This study showed a ⬇️need for antihypertensives if dietary K+ was ⬆️
💥RCT 47 pts w/ htn
💥⬆️ K+ vs usual K+ diet
💥45% ⬆️ in dietary K+ in ⬆️ K+ group
🔥Hypertensive therapy ⬇️by at least 50% in 81% of intervention group v 29% in control group at 1 yr
👉pubmed.ncbi.nlm.nih.gov/1929022/
💥RCT 47 pts w/ htn
💥⬆️ K+ vs usual K+ diet
💥45% ⬆️ in dietary K+ in ⬆️ K+ group
🔥Hypertensive therapy ⬇️by at least 50% in 81% of intervention group v 29% in control group at 1 yr
👉pubmed.ncbi.nlm.nih.gov/1929022/

The opposite is also true: Interesting randomized crossover study
💥10 normotensive men
💥⬇️(10mmol) vs nml (90mmol) K+ diet x 10 days
💥“normal” sodium intake of 120-200mmol
🔥⬇️ K+ intake = ⬆️SBP and DBP by 7 and 6mmHg relative to the ⬆️ K+ diet
👉pubmed.ncbi.nlm.nih.gov/2624617/
💥10 normotensive men
💥⬇️(10mmol) vs nml (90mmol) K+ diet x 10 days
💥“normal” sodium intake of 120-200mmol
🔥⬇️ K+ intake = ⬆️SBP and DBP by 7 and 6mmHg relative to the ⬆️ K+ diet
👉pubmed.ncbi.nlm.nih.gov/2624617/

In the above study sodium excretion was also significantly decreased with potassium restriction. A saline infusion further increased BP with a K+ restricted but not normal K+ diet. 



In the Dallas Heart Study SBP ⬆️ by 1.6 and diastolic by 1 for each 3 unit ⬆️ in UNa/K ratio
👉pubmed.ncbi.nlm.nih.gov/22114147/
Data from INTERSALT suggests a UNa/K ratio <1 may be a useful indicator, providing rapid feedback and🚫need for a 24h urine collection
👉pubmed.ncbi.nlm.nih.gov/30996260/
👉pubmed.ncbi.nlm.nih.gov/22114147/
Data from INTERSALT suggests a UNa/K ratio <1 may be a useful indicator, providing rapid feedback and🚫need for a 24h urine collection
👉pubmed.ncbi.nlm.nih.gov/30996260/

This also translates to hard outcomes. Potassium intake is significantly, inversely associated, with the incidence of CVD or IHD mortality. Higher sodium-potassium ratios are significantly associated with risk of CVD and IHD mortality
pubmed.ncbi.nlm.nih.gov/21747015/
pubmed.ncbi.nlm.nih.gov/21747015/

Ok, it works. But how?
We showed👆that sodium excretion ⬇️ with a low K+ diet
This👇study from 1985 demonstrated that a very low K+ diet (K 2mEq) caused Na+ and H20 retention
ncbi.nlm.nih.gov/pmc/articles/P…
We showed👆that sodium excretion ⬇️ with a low K+ diet
This👇study from 1985 demonstrated that a very low K+ diet (K 2mEq) caused Na+ and H20 retention
ncbi.nlm.nih.gov/pmc/articles/P…

Mechanism
💥⬇️K+➡️K+ exit from cells
💥counterbalanced by protons in = intracellular acidosis, which stimulates the NA-H exchanger (NHE3) in the proximal tubule to restore normal pH = sodium retention
👉Significant⬆️in NHE3 expression in hypokalemic rats pubmed.ncbi.nlm.nih.gov/12388387/
💥⬇️K+➡️K+ exit from cells
💥counterbalanced by protons in = intracellular acidosis, which stimulates the NA-H exchanger (NHE3) in the proximal tubule to restore normal pH = sodium retention
👉Significant⬆️in NHE3 expression in hypokalemic rats pubmed.ncbi.nlm.nih.gov/12388387/

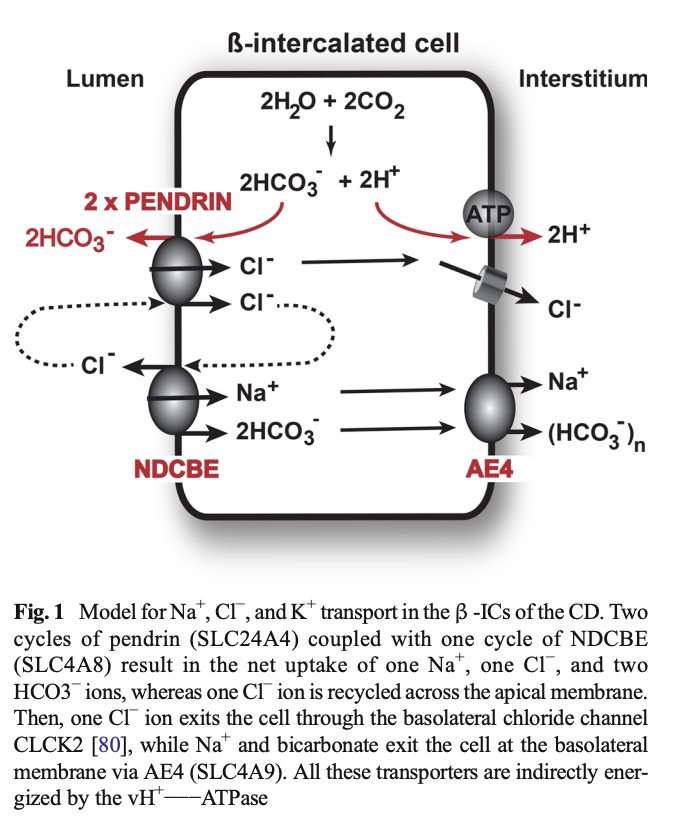
Mechanism
Hypokalemia also increases NCC activity (by modulating intracellular chloride (another example of the physiologic importance of Cl-!)
💥This decreases sodium excretion and increases MAP (at least in mice)
👇ncbi.nlm.nih.gov/pmc/articles/P…

Hypokalemia also increases NCC activity (by modulating intracellular chloride (another example of the physiologic importance of Cl-!)
💥This decreases sodium excretion and increases MAP (at least in mice)
👇ncbi.nlm.nih.gov/pmc/articles/P…


BUT did you know that K+ also appears to vasodilate blood vessels?
When K+ was infused into the brachial artery of dogs blood flow ⬆️ and pressure ⬇️ both by direct action, as well as by attenuating the sensitivity of the arteriole to natural vasopressors, like norepinephrine
When K+ was infused into the brachial artery of dogs blood flow ⬆️ and pressure ⬇️ both by direct action, as well as by attenuating the sensitivity of the arteriole to natural vasopressors, like norepinephrine

In another study when potassium chloride was infused in renal veins, resistance decreased and urine flow increased
Read both these studies
👇journals.physiology.org/doi/pdf/10.115…
👇
journals.physiology.org/doi/pdf/10.115…

Read both these studies
👇journals.physiology.org/doi/pdf/10.115…
👇
journals.physiology.org/doi/pdf/10.115…


Finally, in salt sensitive rats fed a 1% NaCl diet x 8 months, ⬇️ dietary K+ ⬆️ MAP, CO and cerebral + renal vascular resistance, while increasing K+ (to a degree) decreased all of these parameters
Therefore, dietary K+ influences resistance to blood flow through vascular beds
Therefore, dietary K+ influences resistance to blood flow through vascular beds

This effect appears to be due to stimulation of the Na/K ATPase as 👇 study showed that oubain (a potent inhibitor of the Na/K pump) attenuated the vasodilatory effects of potassium
pubmed.ncbi.nlm.nih.gov/4256887/
pubmed.ncbi.nlm.nih.gov/4256887/
Conclusion
💥⬆️dietary K+ can ⬇️ BP
💥Secondary to decreasing sodium reabsorption AND direct vasodilation
💥Monitoring spot UNa/K ratios MAY be a useful indicator of dietary adherence
In case you were wondering the WHO recommends daily potassium intake of at least 90mmol/d
💥⬆️dietary K+ can ⬇️ BP
💥Secondary to decreasing sodium reabsorption AND direct vasodilation
💥Monitoring spot UNa/K ratios MAY be a useful indicator of dietary adherence
In case you were wondering the WHO recommends daily potassium intake of at least 90mmol/d
• • •
Missing some Tweet in this thread? You can try to
force a refresh