1/ Welcome back to #TweetorialTuesday with the #MedEdTwagTeam!
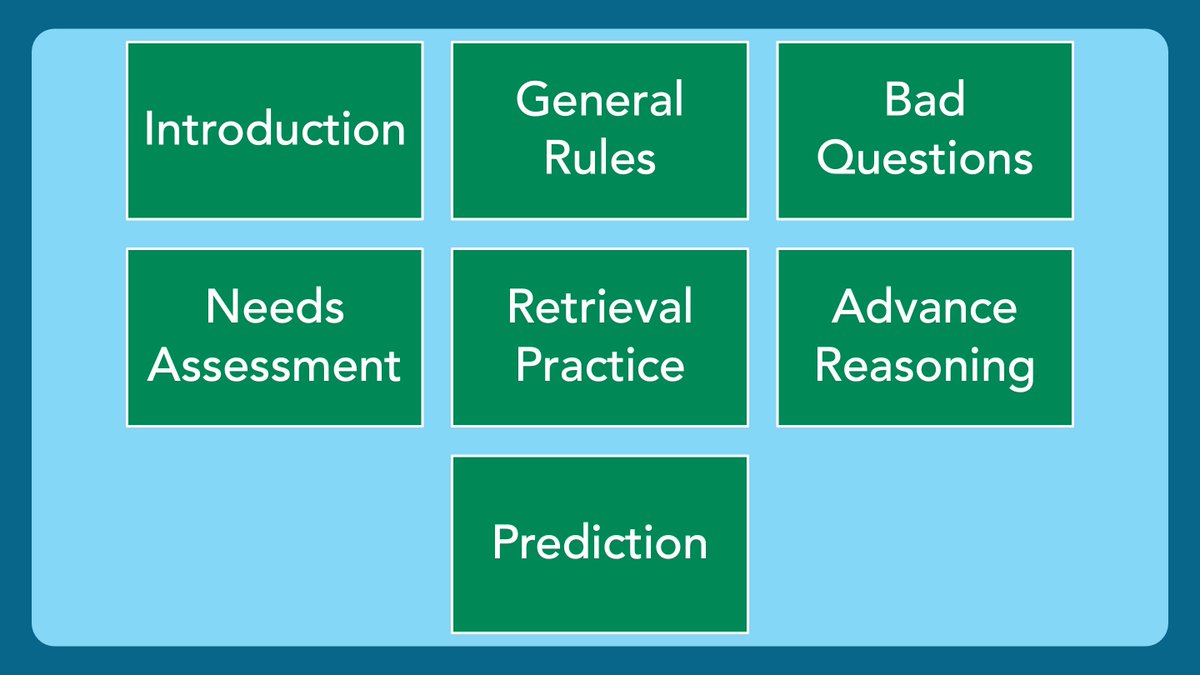
We are in our #EffectiveQuestions series.
Thanks for joining us, #MedTwitter, #MedEd, & #MedStudentTwitter Friends!
We are in our #EffectiveQuestions series.
Thanks for joining us, #MedTwitter, #MedEd, & #MedStudentTwitter Friends!

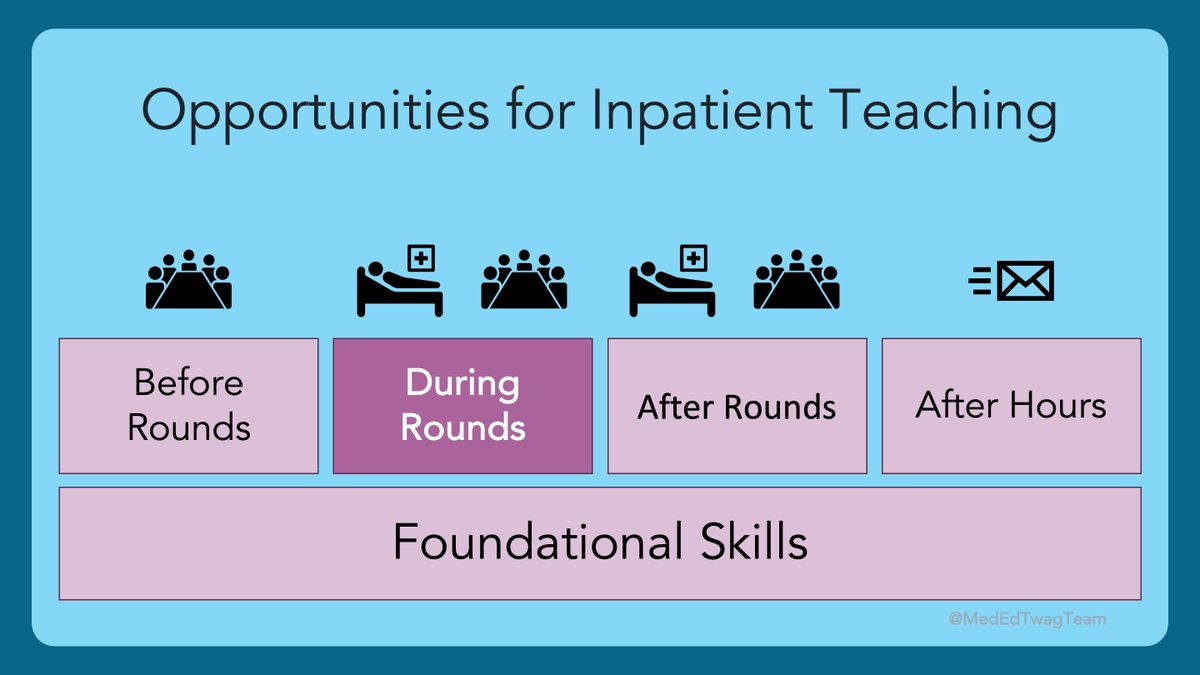
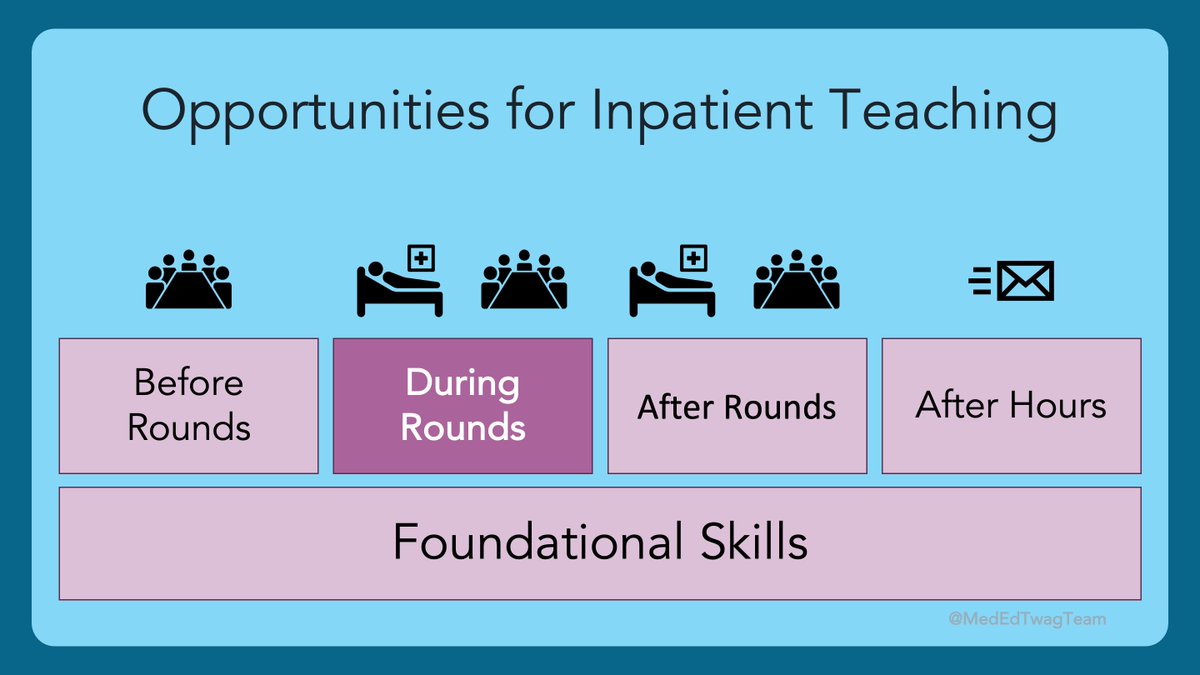
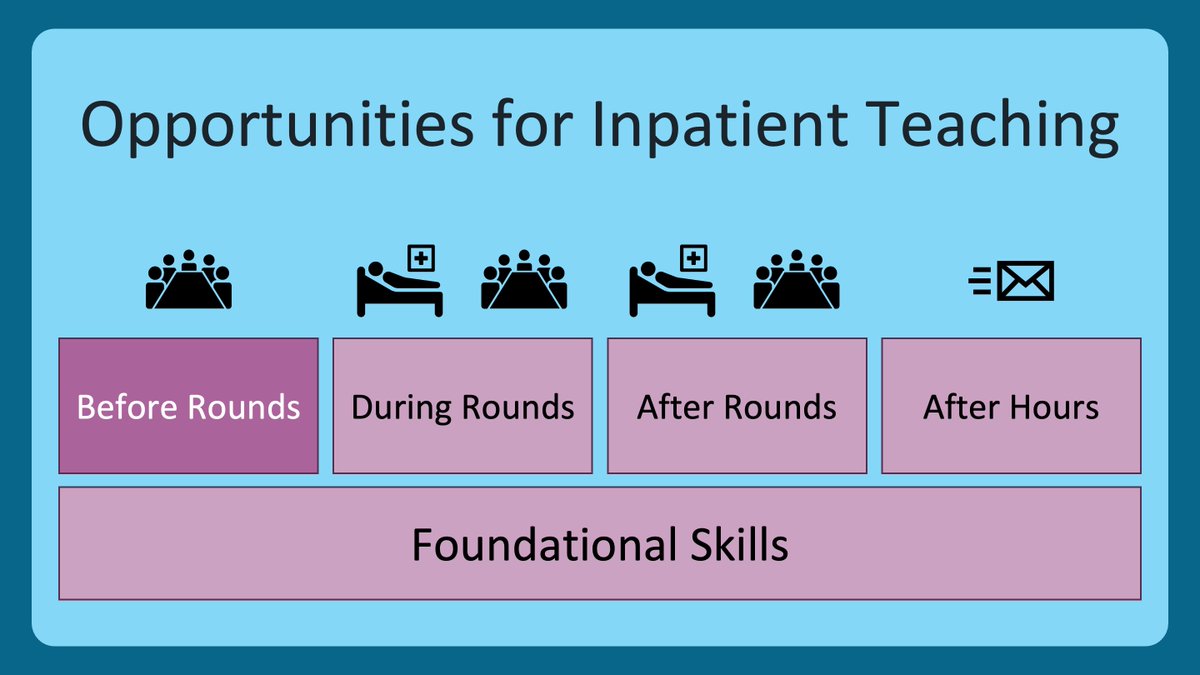
2/ This week we start talking about my favorite uses of questions in the clinical learning environment.
First up is, questions as a needs assessment.
First up is, questions as a needs assessment.

3/ I was schooled in #MedEdScholarship by @posucsf, Dave Irby, and @bobrien_15 @UCSF.
Like most educators of #HPE, they framed curriculum development for me through the lens of “Kern’s Six Steps”.
Like most educators of #HPE, they framed curriculum development for me through the lens of “Kern’s Six Steps”.

4/ @jackpenner and @timdyster from @UCSF/@UCSFIMChiefs are doing some really cool work under the handle @MedEdModels.
If you haven’t heard of #Kern’s, or want a refresher, especially on the needs assessment, check out their awesome visual description:
If you haven’t heard of #Kern’s, or want a refresher, especially on the needs assessment, check out their awesome visual description:
https://twitter.com/MedEdModels/status/1355725572844867586
5/ I mention this because Kern’s approach has rented a room in my brain. I use a modified version for all my teaching efforts. From a pearl on rounds, to a chalk talk, to a 4-hour workshop. The intensity of my approach increases in concordance with the intensity of the teaching. 

6/ As you can see, the first step in all my teaching is identifying a learning need. What is a learning need?
Kern presents an equation that is helpful for me to think about, because I like math. 🤓
Kern presents an equation that is helpful for me to think about, because I like math. 🤓

7/ There are many ways to identify learning needs in the clinical setting. Here are some:
1⃣Listening to presentations – my favorite way
2⃣Learner-initiated questions – they identify the bounds of their knowledge
3⃣Teacher-initiated inquiry – you probe to find those bounds
1⃣Listening to presentations – my favorite way
2⃣Learner-initiated questions – they identify the bounds of their knowledge
3⃣Teacher-initiated inquiry – you probe to find those bounds
8/ When asking questions as a needs assessment, your goal is to find the gap so that you can fill it in. You must state this as your intention & make clear that their responses will not be used as part of evaluation.
Remember back in the General Rules?
Remember back in the General Rules?
https://twitter.com/GStetsonMD/status/1389637218080329730
9/ The best way to perform a needs assessment is through BROAD & OPEN-ENDED inquiry.
💡Broad – An invitation for learners to share the knowledge they possess, ideally up to their limits.
💡Open-Ended – It would be difficult to answer the question with any single word.
💡Broad – An invitation for learners to share the knowledge they possess, ideally up to their limits.
💡Open-Ended – It would be difficult to answer the question with any single word.
10/ There are hundreds of questions that could fit these similar BROAD and OPEN-ENDED principles. Here are some examples in some specific categories: 

11/ Notice the question words.
“How” and “why” are excellent, as they naturally lead to broad and open-ended questions.
“What” is good too, but you need to be careful that you are not looking for an answer that is too specific.
“How” and “why” are excellent, as they naturally lead to broad and open-ended questions.
“What” is good too, but you need to be careful that you are not looking for an answer that is too specific.

12/ Another key piece to a good needs assessment question is the word ”you”. Why?
Because you are assessing the needs of the specific learner. Your goal is to find out how they, specifically, think about & approach various clinical scenarios.
Because you are assessing the needs of the specific learner. Your goal is to find out how they, specifically, think about & approach various clinical scenarios.

13/ What happens when we don't use "you"? Notice how some subtle changes can alter the intention of the question?
🔑Omitting the word “you” can imply a "right" answer.
🔑Using us/we/our language can lead the learner to guess what “we” are thinking.
🔑Omitting the word “you” can imply a "right" answer.
🔑Using us/we/our language can lead the learner to guess what “we” are thinking.

14/ Today I presented some big ideas and some more subtle things that can make a big difference in identifying the needs of your learners, thus helping you to be a more targeted and effective teacher.
The main takeaways are:
The main takeaways are:

15/ Thanks for joining us!
Please, join us again next week as we dive into questions to facilitate retrieval practice.
To not miss out, make sure to follow: @MedEdTwagTeam, @JenniferSpcier4, and me
Tweet you then.
Please, join us again next week as we dive into questions to facilitate retrieval practice.
To not miss out, make sure to follow: @MedEdTwagTeam, @JenniferSpcier4, and me
Tweet you then.

• • •
Missing some Tweet in this thread? You can try to
force a refresh