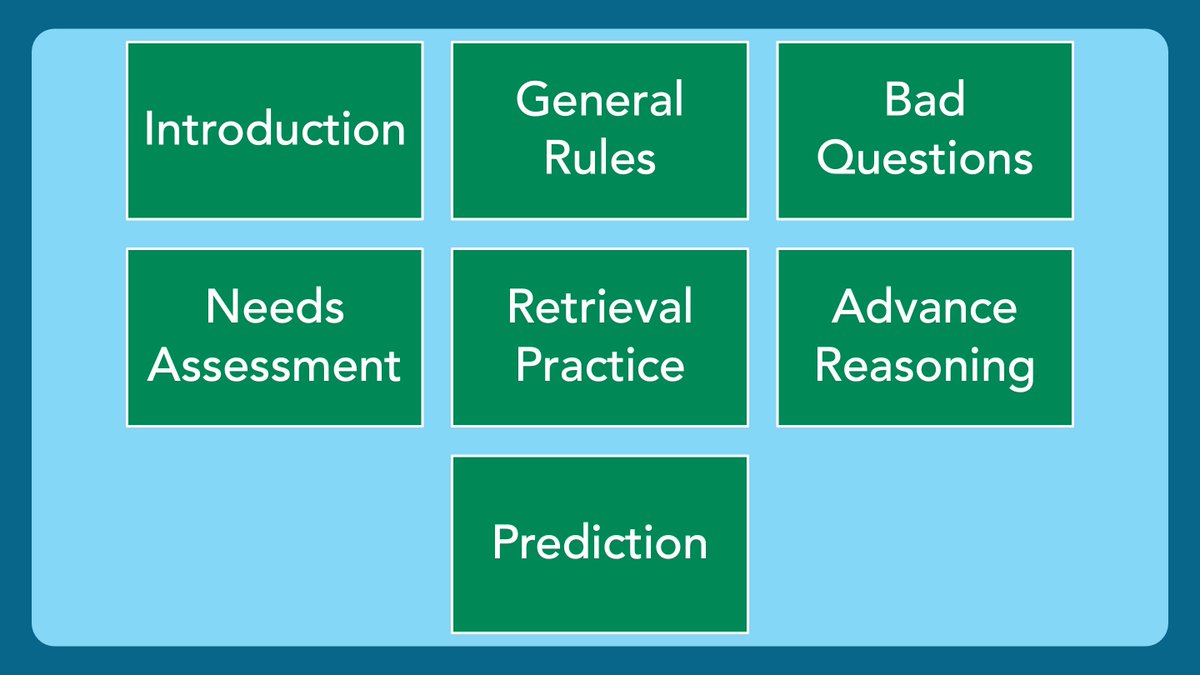
1/ Welcome back to #TweetorialTuesday with the #MedEdTwagTeam!
We are in our #EffectiveQuestions series.
Thanks for joining us, #MedTwitter, #MedEd, & #MedStudentTwitter Friends!
We are in our #EffectiveQuestions series.
Thanks for joining us, #MedTwitter, #MedEd, & #MedStudentTwitter Friends!
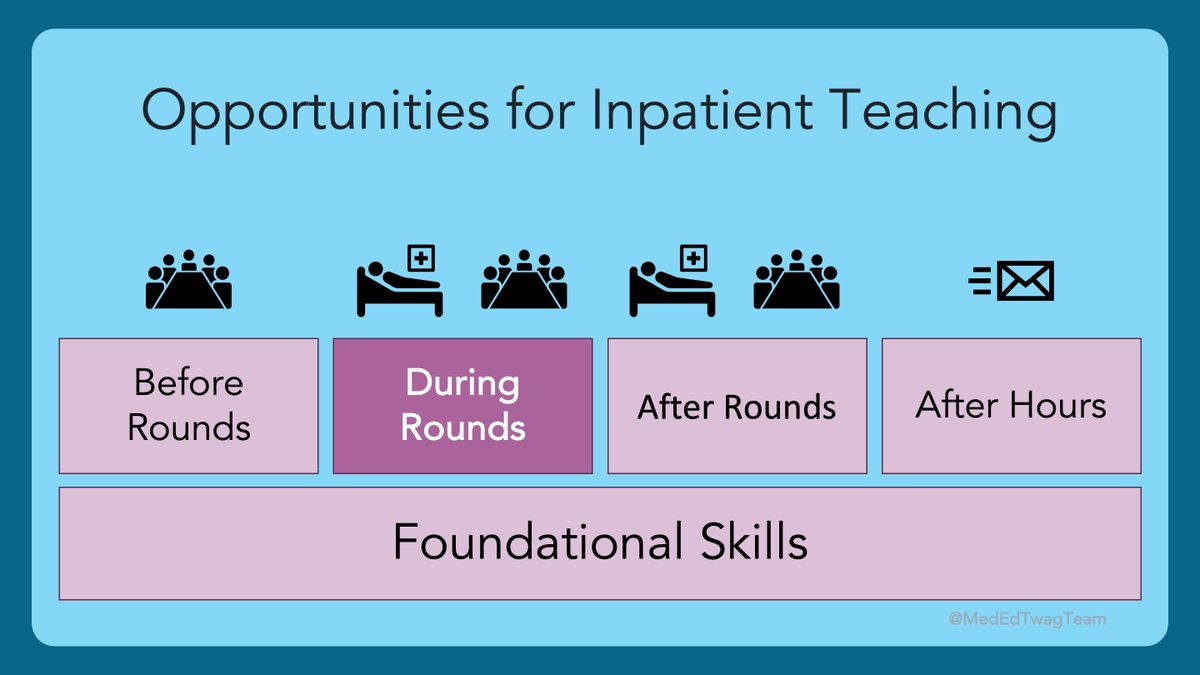
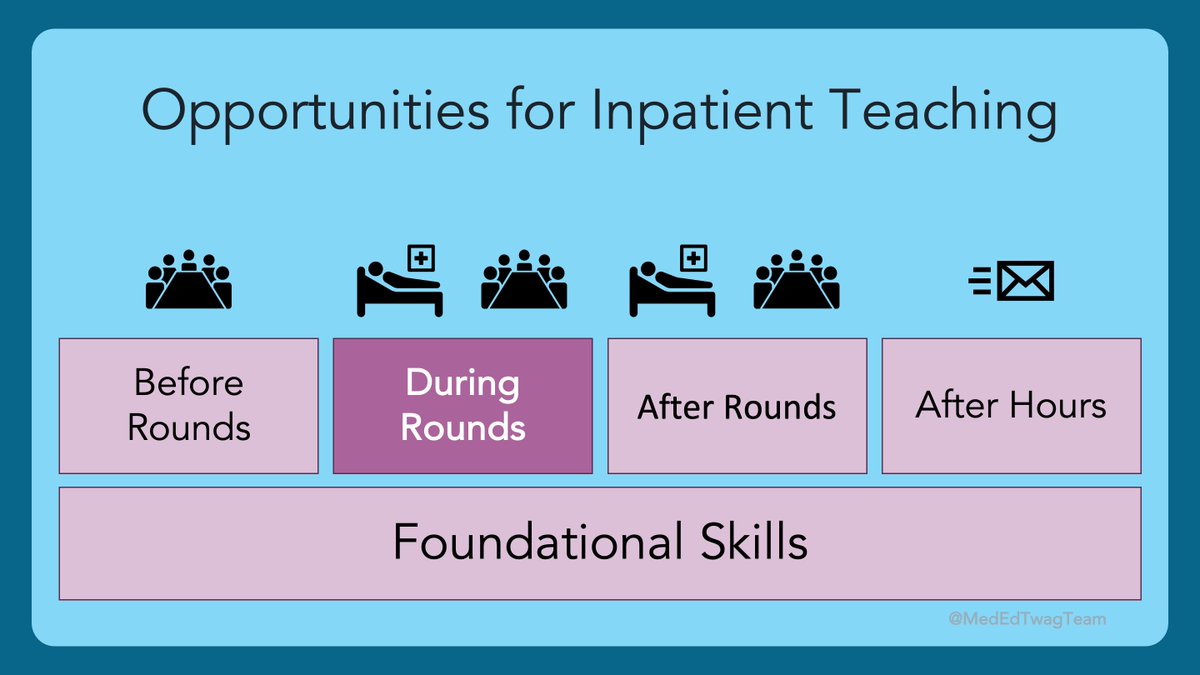
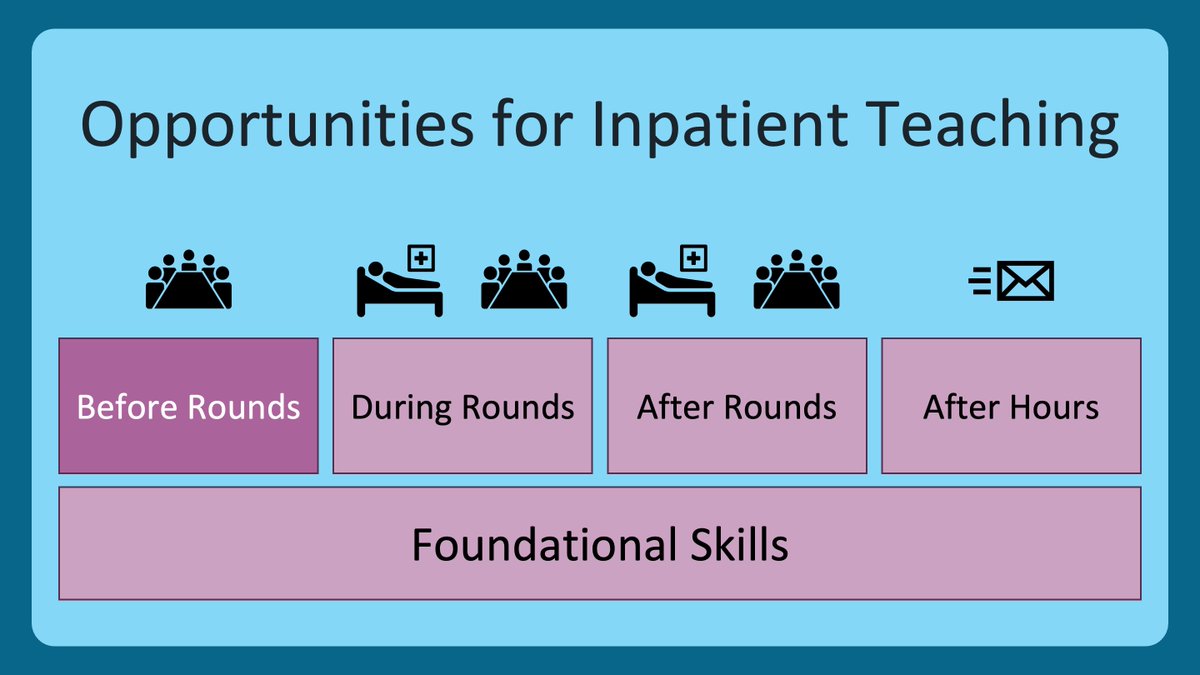
2/ This week we continue talking about my favorite uses of questions in the clinical learning environment.
Last week was questions as a needs assessment. Go back and check that out if you missed it.
This week is questions for retrieval practice.
Last week was questions as a needs assessment. Go back and check that out if you missed it.
This week is questions for retrieval practice.

3/ Much of today’s thread is derived from a favorite book...Make It Stick: The Science of Successful Learning.
It is very approachable and has super useful content. Today, we will talk about retrieval practice, and briefly touch on spaced learning and interleaving.
It is very approachable and has super useful content. Today, we will talk about retrieval practice, and briefly touch on spaced learning and interleaving.

5/ Some might read the above quote and think I am advocating for ”pimping”, which is a reasonable interpretation of the text. To be clear, I am not.
One can promote retrieval practice by using the same broad & open-ended questions we discussed last week.
One can promote retrieval practice by using the same broad & open-ended questions we discussed last week.
https://twitter.com/GStetsonMD/status/1394757163881488384
6/ A better way to use retrieval practice in the clinical setting is as a tool to consolidate learning that my team and I have done together.
This is material I know they have been exposed to, as opposed to information I am assuming they learned during their pre-clinical years.
This is material I know they have been exposed to, as opposed to information I am assuming they learned during their pre-clinical years.
7/ When retrieval practice is framed as a tool for solidifying memories (as opposed to evaluation), it can be a lot of fun! 🥳🎉
In this case, asking questions that have specific answers is the correct approach.
In this case, asking questions that have specific answers is the correct approach.
8/ To use retrieval practice, each day, make note of 3-5 specific things you have learned with your team, or taught to your team. Below are some examples, but the list is endless! 

9/ Then, make time for a recall exercise. This is a great use of your teaching time or “attending rounds”.
Set the expectation that this is a fun, team-based activity, for the sole purpose of learning. Like a Jeopardy-style game. #RIPTrebek
Set the expectation that this is a fun, team-based activity, for the sole purpose of learning. Like a Jeopardy-style game. #RIPTrebek
10/ Then, pose your questions, one at a time.
🔑A key to what I do is I make everyone write down their answer to each question before anyone takes a stab at answering it for the group. Struggling to remember is the most important part of this exercise.
🔑A key to what I do is I make everyone write down their answer to each question before anyone takes a stab at answering it for the group. Struggling to remember is the most important part of this exercise.

11/ If you teach primarily in the outpatient or emergency setting, start off each precepting session recalling learning points from the previous week or two with each preceptee. Again, frame it as a fun game, for you & the trainee, all for the sake of learning.
12/ Two other important ideas from Make it Stick are spaced learning and interleaving. Here is an explanation: 

13/ My takeaways on spaced learning & interleaving:
Give your learners enough time to start forgetting information before testing it. A few days should suffice.
Interleaving is inherent in clinical training given its complexity. Your questions should reflect the varied learning.
Give your learners enough time to start forgetting information before testing it. A few days should suffice.
Interleaving is inherent in clinical training given its complexity. Your questions should reflect the varied learning.
14/ I hope this presents you all with a new tool to solidify learning for your trainees. It is backed by science & can be a lot of fun.
Have you done something like this before? How’d it go? What have you learned?
If you haven’t, try it out! Please, share your experience.
Have you done something like this before? How’d it go? What have you learned?
If you haven’t, try it out! Please, share your experience.

15/ Thanks for joining us!
Please, join us again next week as we dive into questions to advance clinical reasoning.
To not miss out, make sure to follow: @MedEdTwagTeam, @JenniferSpicer4, and me
Tweet you then.
Please, join us again next week as we dive into questions to advance clinical reasoning.
To not miss out, make sure to follow: @MedEdTwagTeam, @JenniferSpicer4, and me
Tweet you then.

• • •
Missing some Tweet in this thread? You can try to
force a refresh