fresh RCT on the effects of a continuous infusion of hypertonic saline for traumatic brain injury (#1/6)
jamanetwork.com/journals/jama/…
jamanetwork.com/journals/jama/…

patients were randomized to an infusion of 20% NaCl for 48 hours. as shown here, the infusion was successful at pushing sodium levels to the mid-150s, with nice separation between groups (#2/6) 
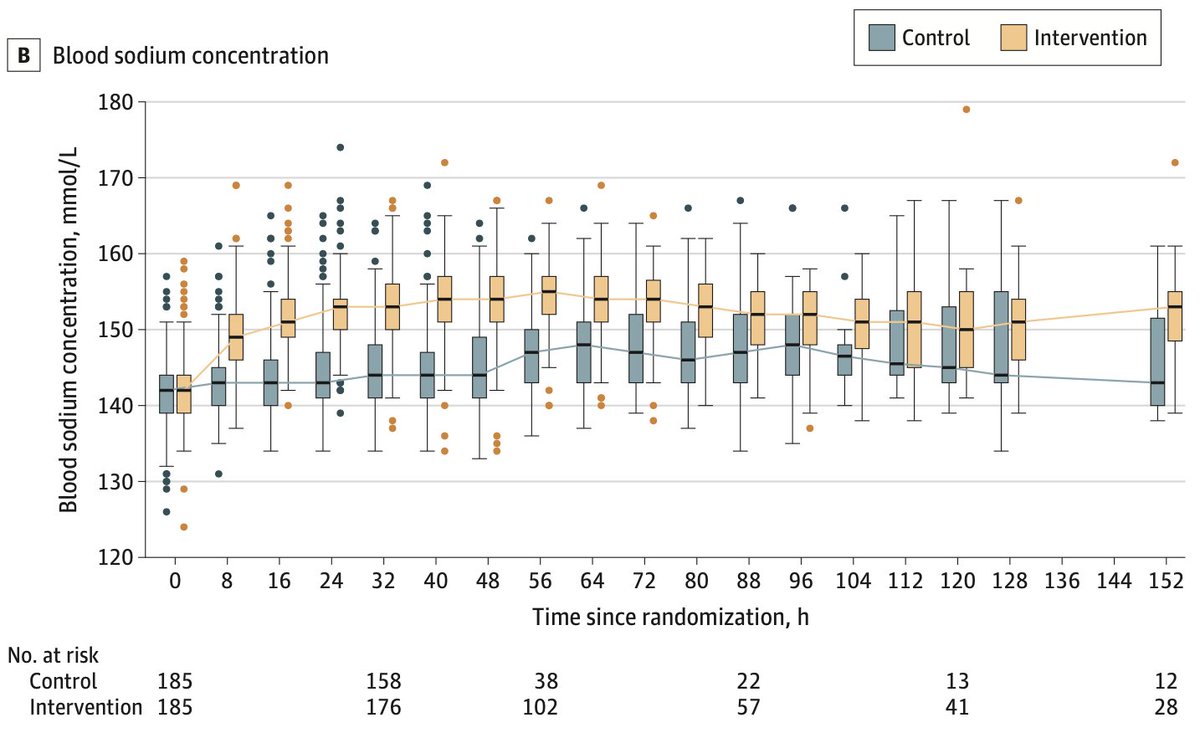
initially, patients receiving hypertonic infusions had fewer episodes of ICP elevation. however, their brain cells adapted rapidly to the higher tonicity... so when the hypertonic was stopped they had *rebound* elevation of ICP (#3/6) 

ultimately patients treated w/ hypertonic infusions needed *more* rescue therapies for ICP:
😬 trend towards more boluses of hypertonic therapy
😬 significantly greater use of hyperventilation
so routine induction of abnormal physiology probably caused more harm than good
😬 trend towards more boluses of hypertonic therapy
😬 significantly greater use of hyperventilation
so routine induction of abnormal physiology probably caused more harm than good
there was no difference in the primary endpoint (functional outcome after six months). not surprising, given the number of factors affecting this endpoint. and also, the fact that ICP was monitored and *corrected* when things were really going sideways. (#5/6) 

the negative results of this study were predicted & explained further in this blog from 2014. bottom line:
🤯 giving everybody hypertonic infusions like Oprah isn't good
🤯better to use boluses when truly needed, as a temporary bridge to another treatment
emcrit.org/pulmcrit/hyper…
🤯 giving everybody hypertonic infusions like Oprah isn't good
🤯better to use boluses when truly needed, as a temporary bridge to another treatment
emcrit.org/pulmcrit/hyper…
• • •
Missing some Tweet in this thread? You can try to
force a refresh