1/
In 2019, @jared_w_magnani & I were invited to give @PittGIM Grand Rounds on the social determinants of #AFib.
Today, thanks to our incredible co-authors, we published some of those thoughts in Nature! 👇🏾
A 🧵 on gaps & opportunities for future work.
nature.com/articles/s4156….
In 2019, @jared_w_magnani & I were invited to give @PittGIM Grand Rounds on the social determinants of #AFib.
Today, thanks to our incredible co-authors, we published some of those thoughts in Nature! 👇🏾
A 🧵 on gaps & opportunities for future work.
nature.com/articles/s4156….
2/
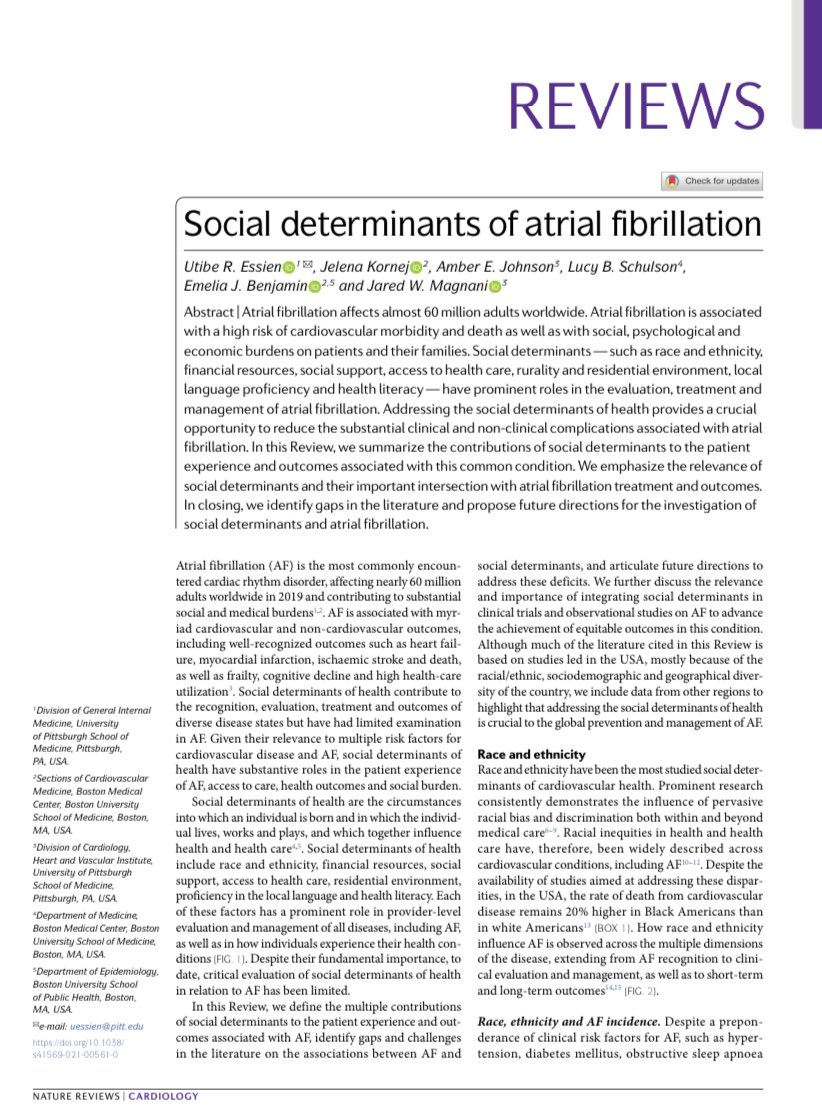
The pandemic has taught us so much about our health system, but it has especially shone a bright light on the social determinants as key drivers of #HealthEquity. Our review focused on:
🔸 race/ethnicity
🔸 finances
🔸 rurality/neighborhood
🔸 health literacy
🔸 social network
The pandemic has taught us so much about our health system, but it has especially shone a bright light on the social determinants as key drivers of #HealthEquity. Our review focused on:
🔸 race/ethnicity
🔸 finances
🔸 rurality/neighborhood
🔸 health literacy
🔸 social network

3/
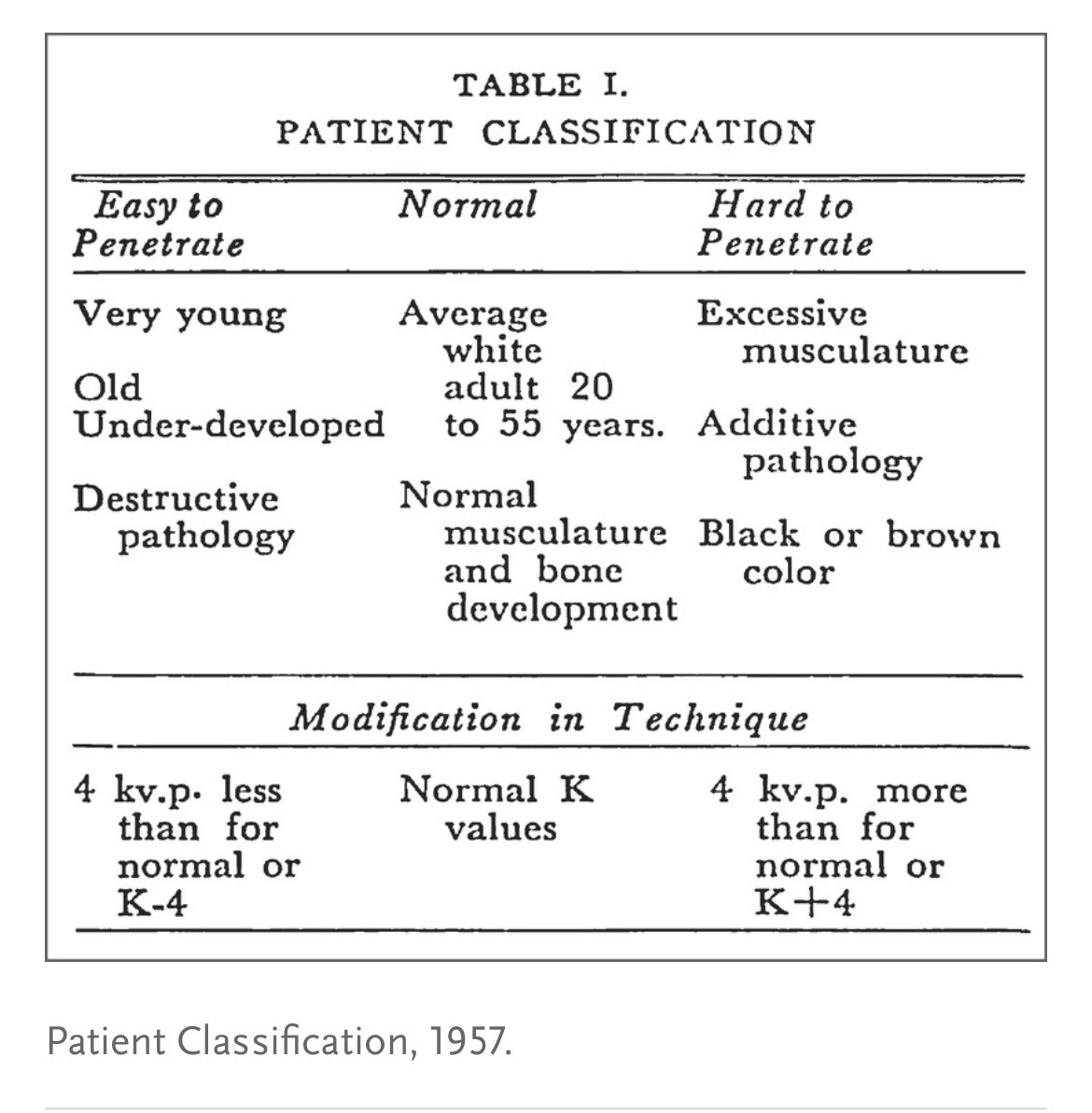
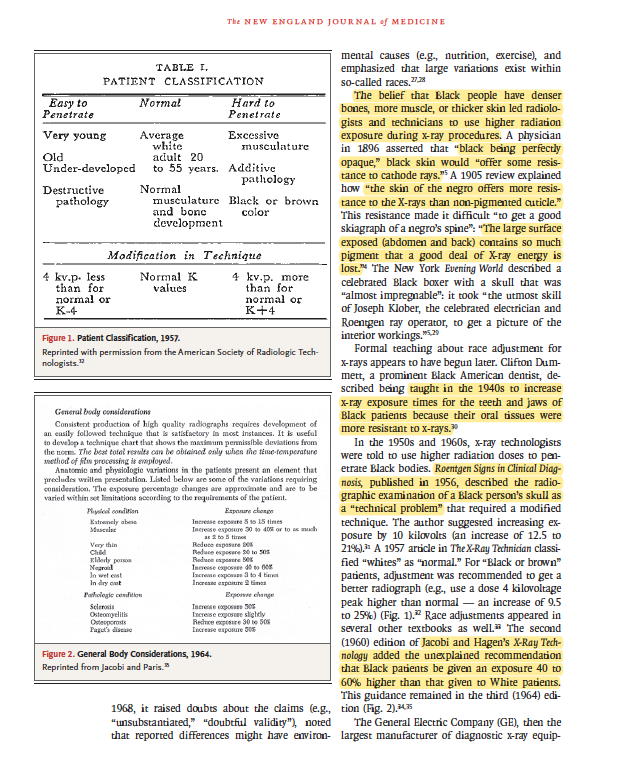
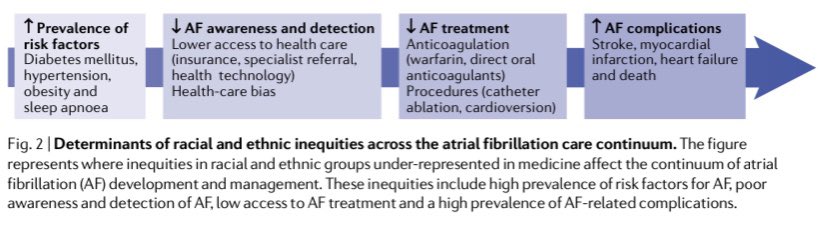
The social construct of race has been one of the most well-studied determinants of #AFib incidence, treatment (including our work in anticoagulation disparities), and outcomes. Here we discuss why such inequities exist across the AFib care continuum.
nature.com/articles/s4156….
The social construct of race has been one of the most well-studied determinants of #AFib incidence, treatment (including our work in anticoagulation disparities), and outcomes. Here we discuss why such inequities exist across the AFib care continuum.
nature.com/articles/s4156….
4/
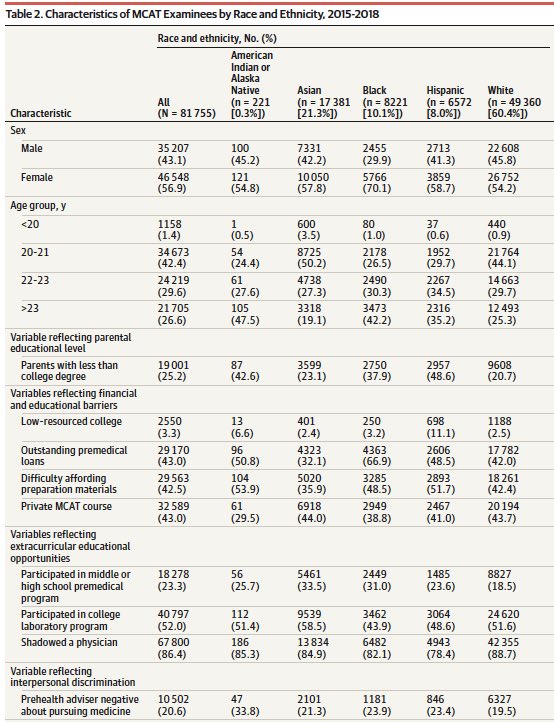
Our review also adds to a critical conversation on racial & ethnic representation in clinical trials, as well as observational & prospective cohort studies.
In the past decade, non-White racial/ethnic groups have been *very* underrepresented in #AFib studies. Room to improve!
Our review also adds to a critical conversation on racial & ethnic representation in clinical trials, as well as observational & prospective cohort studies.
In the past decade, non-White racial/ethnic groups have been *very* underrepresented in #AFib studies. Room to improve!

5/
⬆️ income & wealth is related to better healthcare access, provider decision-making and clinical outcomes in #AFib while ⬇️ income has been related to higher rates of cardiac risk factors, adverse events & death.
We also dive into some reasons why.
nature.com/articles/s4156….
⬆️ income & wealth is related to better healthcare access, provider decision-making and clinical outcomes in #AFib while ⬇️ income has been related to higher rates of cardiac risk factors, adverse events & death.
We also dive into some reasons why.
nature.com/articles/s4156….
6/
Prior work has shown differences in CV health b/w folks living in rural vs. urban settings but few have studied this in #AFib.
Similarly we discuss how more work is needed to study the complex intersection b/w neighborhood-level factors & AF outcomes.
nature.com/articles/s4156…
Prior work has shown differences in CV health b/w folks living in rural vs. urban settings but few have studied this in #AFib.
Similarly we discuss how more work is needed to study the complex intersection b/w neighborhood-level factors & AF outcomes.
nature.com/articles/s4156…
7/
Low health literacy (and limited English proficiency) is related to ⬇️ awareness of #AFib, its treatment (including poor warfarin control) and its outcomes.
We need to improve capture of health literacy & understand its role in shared decision-making.
nature.com/articles/s4156…
Low health literacy (and limited English proficiency) is related to ⬇️ awareness of #AFib, its treatment (including poor warfarin control) and its outcomes.
We need to improve capture of health literacy & understand its role in shared decision-making.
nature.com/articles/s4156…
8/
Little has been published on the relationship between social support (e.g., partners, caregivers) or social connectedness (or lack thereof) on #AFib.
We propose a pathway for the physical & psychological connection & highlight this area as another important future direction.
Little has been published on the relationship between social support (e.g., partners, caregivers) or social connectedness (or lack thereof) on #AFib.
We propose a pathway for the physical & psychological connection & highlight this area as another important future direction.

9/
In summary, we argue that #AFib offers an important opportunity to study the social determinants, including how they all overlap/interact at the patient, community, and policy level.
We also must acknowledge how structural racism drives many of the factors we discuss.
In summary, we argue that #AFib offers an important opportunity to study the social determinants, including how they all overlap/interact at the patient, community, and policy level.
We also must acknowledge how structural racism drives many of the factors we discuss.

10/
Also, we didn’t get to mention factors such as access to safe neighborhoods & healthy food, allostatic load, adverse childhood events, housing instability & homelessness, incarceration, or immigration status given the lack of #AFib literature.
Future grant idea anyone? 🤔
Also, we didn’t get to mention factors such as access to safe neighborhoods & healthy food, allostatic load, adverse childhood events, housing instability & homelessness, incarceration, or immigration status given the lack of #AFib literature.
Future grant idea anyone? 🤔

11/11
🙏🏾 to @JKornej @AmberJohnsonMD @LucySchulson @EmeliaBenjamin @jared_w_magnani for joining me on this project these past 18 months (in the middle of a whole pandemic and daily onslaughts of racism).
Look forward to yall’s thoughts and future collaboration in this work. 💪🏾
🙏🏾 to @JKornej @AmberJohnsonMD @LucySchulson @EmeliaBenjamin @jared_w_magnani for joining me on this project these past 18 months (in the middle of a whole pandemic and daily onslaughts of racism).
Look forward to yall’s thoughts and future collaboration in this work. 💪🏾

• • •
Missing some Tweet in this thread? You can try to
force a refresh