1/
Why do we use NAC (n-acetylcysteine) for tylenol overdose?
A #tweetorial
tylenol is also known as paracetamol, acetaminophen, APAP
#livertwitter #meded #medtwitter
Why do we use NAC (n-acetylcysteine) for tylenol overdose?
A #tweetorial
tylenol is also known as paracetamol, acetaminophen, APAP
#livertwitter #meded #medtwitter
2/
Every year in the US alone, >50,000 acetaminophen overdoses are reported to poison centers, causing >110 deaths. Overdose can be intentional, though often accidental, always tragic.
There's an antidote: NAC. It saves lives.
Want to know how it was discovered?
Every year in the US alone, >50,000 acetaminophen overdoses are reported to poison centers, causing >110 deaths. Overdose can be intentional, though often accidental, always tragic.
There's an antidote: NAC. It saves lives.
Want to know how it was discovered?

3/
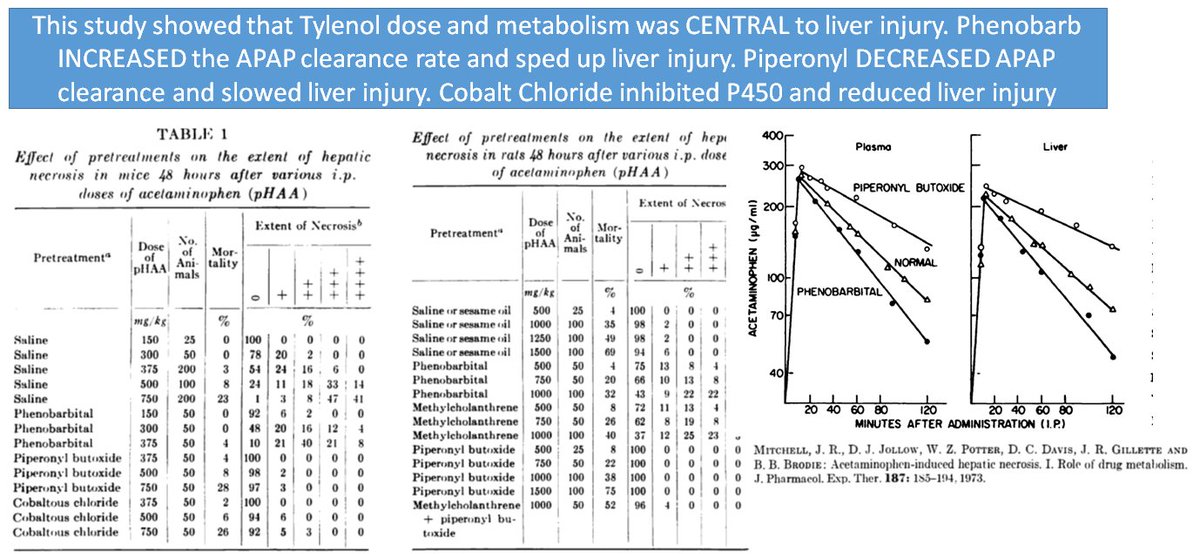
In the 1970's, Drs. Laurie Prescott & Roger Williams showed people were dying of APAP overdose in the UK
Then Mitchell et al released 6 papers showing why & what to do. Their 1st paper confirmed APAP dosing was key & showed that liver injury was due to p450 metabolism
In the 1970's, Drs. Laurie Prescott & Roger Williams showed people were dying of APAP overdose in the UK
Then Mitchell et al released 6 papers showing why & what to do. Their 1st paper confirmed APAP dosing was key & showed that liver injury was due to p450 metabolism
4/
The 2nd Mitchell paper showed:
1⃣Liver damage is directly proportion to covalent binding of an unknown toxic metabolite
2⃣The binding happens in centrilobular liver
3⃣Treatments that reduce the toxin's covalent binding lead to reduced liver injury
The 2nd Mitchell paper showed:
1⃣Liver damage is directly proportion to covalent binding of an unknown toxic metabolite
2⃣The binding happens in centrilobular liver
3⃣Treatments that reduce the toxin's covalent binding lead to reduced liver injury

5/
The 3rd Mitchell paper showed APAP liver damage is caused by a P450 metabolite, happening:
1⃣When NADPH is available
2⃣By oxidation
It's prevented by glutathione/cysteine, showing that glutathione’s role is to protect cellular proteins from attack by toxic metabolites
The 3rd Mitchell paper showed APAP liver damage is caused by a P450 metabolite, happening:
1⃣When NADPH is available
2⃣By oxidation
It's prevented by glutathione/cysteine, showing that glutathione’s role is to protect cellular proteins from attack by toxic metabolites

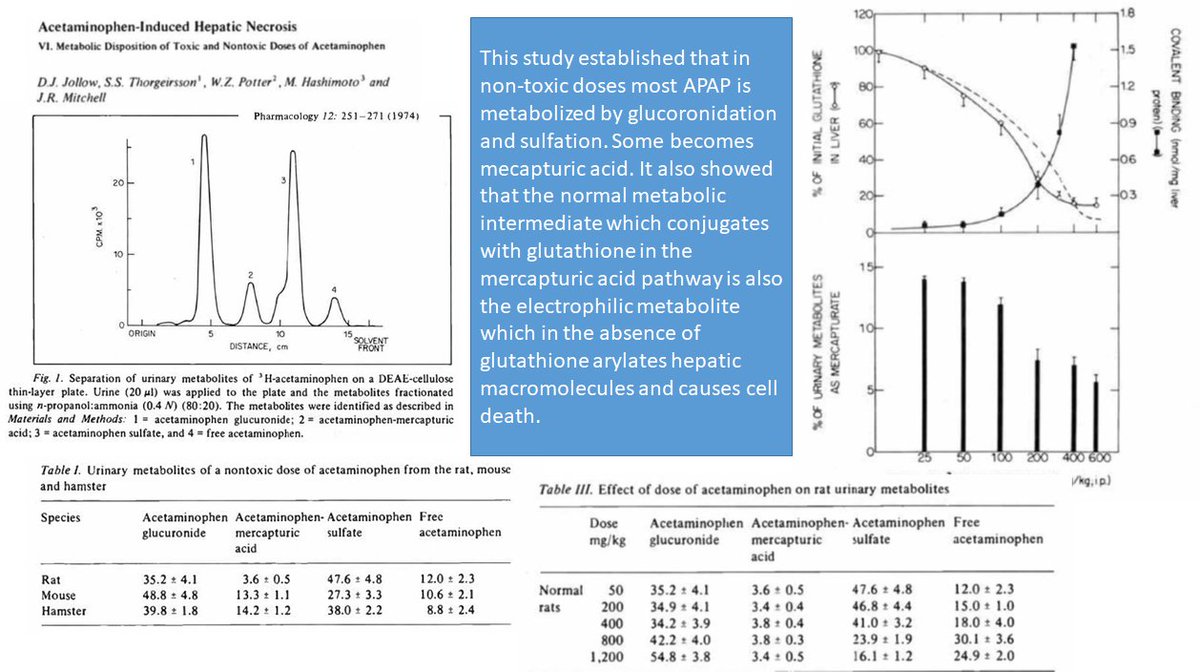
6/
The 70% rule for glutathione:
The 4th Mitchell paper showed liver damage, caused by covalent binding of the toxic metabolic to liver proteins, happens when 70% of the liver's glutathione is depleted (the 5th paper repeated experiments in a hamster model)
The 70% rule for glutathione:
The 4th Mitchell paper showed liver damage, caused by covalent binding of the toxic metabolic to liver proteins, happens when 70% of the liver's glutathione is depleted (the 5th paper repeated experiments in a hamster model)

7/
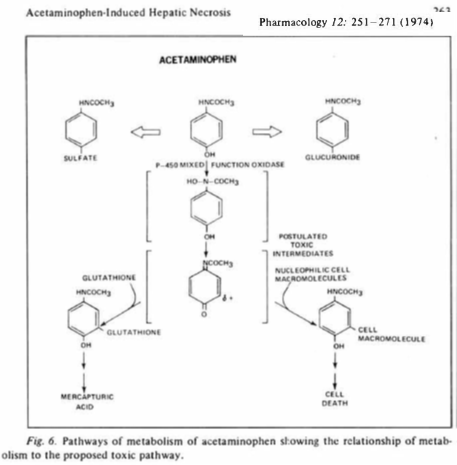
The full picture:
Then Mitchell showed that most APAP is metabolized by glucoronidation, some by sulfation, and that liver injury happens when these pathways are overwhelmed by overdose and glutathione stores are 70% depleted leading to the p450 oxidative pathway
The full picture:
Then Mitchell showed that most APAP is metabolized by glucoronidation, some by sulfation, and that liver injury happens when these pathways are overwhelmed by overdose and glutathione stores are 70% depleted leading to the p450 oxidative pathway
8/
Based on these landmark studies, the authors summarized their work with this diagram - which we all learn today. It has been modified slightly as we learn more about the specific p450s involved
Based on these landmark studies, the authors summarized their work with this diagram - which we all learn today. It has been modified slightly as we learn more about the specific p450s involved

9/
From bench to bedside:
Mitchell gave 🐁 Cysteamine to replete glutathione. It worked. While waiting for his paper to publish, he told Laurie Prescott about it. She gave it to 5 patients with APAP overdose. It WORKED. But it made ppl feel🤮🤮. We needed something else

From bench to bedside:
Mitchell gave 🐁 Cysteamine to replete glutathione. It worked. While waiting for his paper to publish, he told Laurie Prescott about it. She gave it to 5 patients with APAP overdose. It WORKED. But it made ppl feel🤮🤮. We needed something else


10/
Concerns were raised about Cysteamine. It made people feel like garbage. It wasnt commercially available. But Dr. Laurie Prescott suggested NAC would prob work just as well
So Piperno, in the US, tried it out (in mice). Prescott was right. NAC worked better!
Concerns were raised about Cysteamine. It made people feel like garbage. It wasnt commercially available. But Dr. Laurie Prescott suggested NAC would prob work just as well
So Piperno, in the US, tried it out (in mice). Prescott was right. NAC worked better!

11/
NAC, unlike cysteamine, was available as mucomyst, an oral medication with no safety concerns, even if it smelled like rotten eggs!
So a pediatrician named Barry Rumack got approval from the FDA for a multicenter trial
NAC, unlike cysteamine, was available as mucomyst, an oral medication with no safety concerns, even if it smelled like rotten eggs!
So a pediatrician named Barry Rumack got approval from the FDA for a multicenter trial
12/
Why no RCT?
Originally an RCT was planned but was scrapped after advocacy from Dr. Prescott in the Lancet and others questioning the ethics of with-holding treatment. A multicenter study (with central lab) was launched instead
Why no RCT?
Originally an RCT was planned but was scrapped after advocacy from Dr. Prescott in the Lancet and others questioning the ethics of with-holding treatment. A multicenter study (with central lab) was launched instead
13/
The nomogram
The trial would analyze the data for people at high risk of liver injury. Using Prescott's data, Rumack drew a line separating high from low risk based on the APAP level and time from ingestion. The FDA required a 25% fudge factor. And history was made.
The nomogram
The trial would analyze the data for people at high risk of liver injury. Using Prescott's data, Rumack drew a line separating high from low risk based on the APAP level and time from ingestion. The FDA required a 25% fudge factor. And history was made.

14/
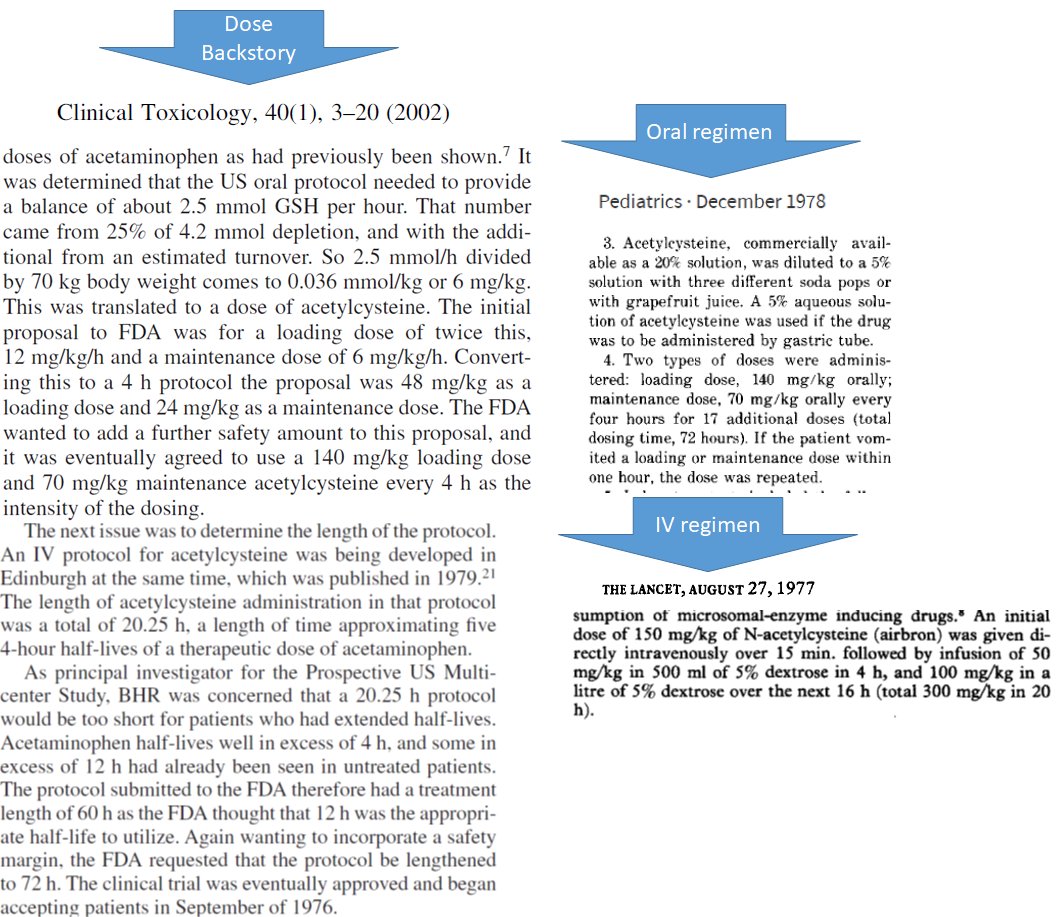
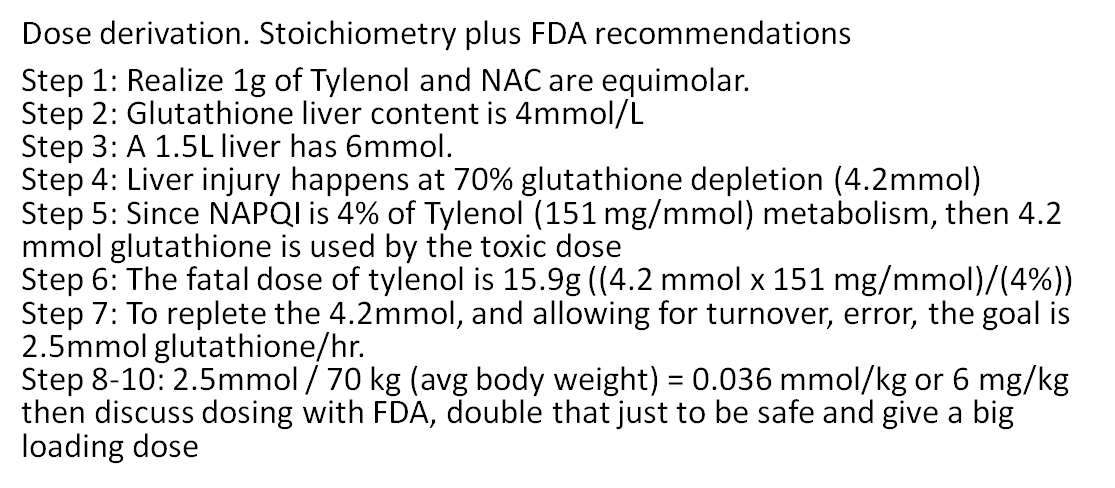
NAC dosing protocol
The dose and duration of oral NAC was derived stoichiometrically, matching NAC to glutathione molecule for molecule over 4 APAP half-lives based on the Mitchell experiments. The UK’s IV protocol was likely taken from the oral protocol

NAC dosing protocol
The dose and duration of oral NAC was derived stoichiometrically, matching NAC to glutathione molecule for molecule over 4 APAP half-lives based on the Mitchell experiments. The UK’s IV protocol was likely taken from the oral protocol
15/
NAC WORKS
Here's the data:
1⃣The earlier the better!
2⃣Overall Mortality was 0.43%, 1.3% for high risk, 3.1% for high risk patients outside 16 hours
Oral was approved in 1985, IV in 2004. PO & IV are prob equivalent. But IV is def easier to give. So, IV it is!

NAC WORKS
Here's the data:
1⃣The earlier the better!
2⃣Overall Mortality was 0.43%, 1.3% for high risk, 3.1% for high risk patients outside 16 hours
Oral was approved in 1985, IV in 2004. PO & IV are prob equivalent. But IV is def easier to give. So, IV it is!


16/
Did I say no RCTs of NAC?
Actually, there's one – small but important
In patients with established acute liver failure - beyond the treatment window, Roger Williams showed improved survival.
Did I say no RCTs of NAC?
Actually, there's one – small but important
In patients with established acute liver failure - beyond the treatment window, Roger Williams showed improved survival.

17/
Summary:
1⃣Tylenol/APAP overdose has an antidote, NAC
2⃣The discovery of NAC came from understanding the physiology of APAP metabolism
3⃣When the liver's glutathione stores are 70% depleted, injury occurs
4⃣NAC replaces glutathione
Summary:
1⃣Tylenol/APAP overdose has an antidote, NAC
2⃣The discovery of NAC came from understanding the physiology of APAP metabolism
3⃣When the liver's glutathione stores are 70% depleted, injury occurs
4⃣NAC replaces glutathione
end/
Thank you for reading this #tweetorial on the discovery and use of NAC - a true life saver. I hope you enjoyed. I would like to thank Barry Rumack (who helped me with background research for this), Laurie Prescott, and Roger Williams for their work that I apply on the wards
Thank you for reading this #tweetorial on the discovery and use of NAC - a true life saver. I hope you enjoyed. I would like to thank Barry Rumack (who helped me with background research for this), Laurie Prescott, and Roger Williams for their work that I apply on the wards
• • •
Missing some Tweet in this thread? You can try to
force a refresh













