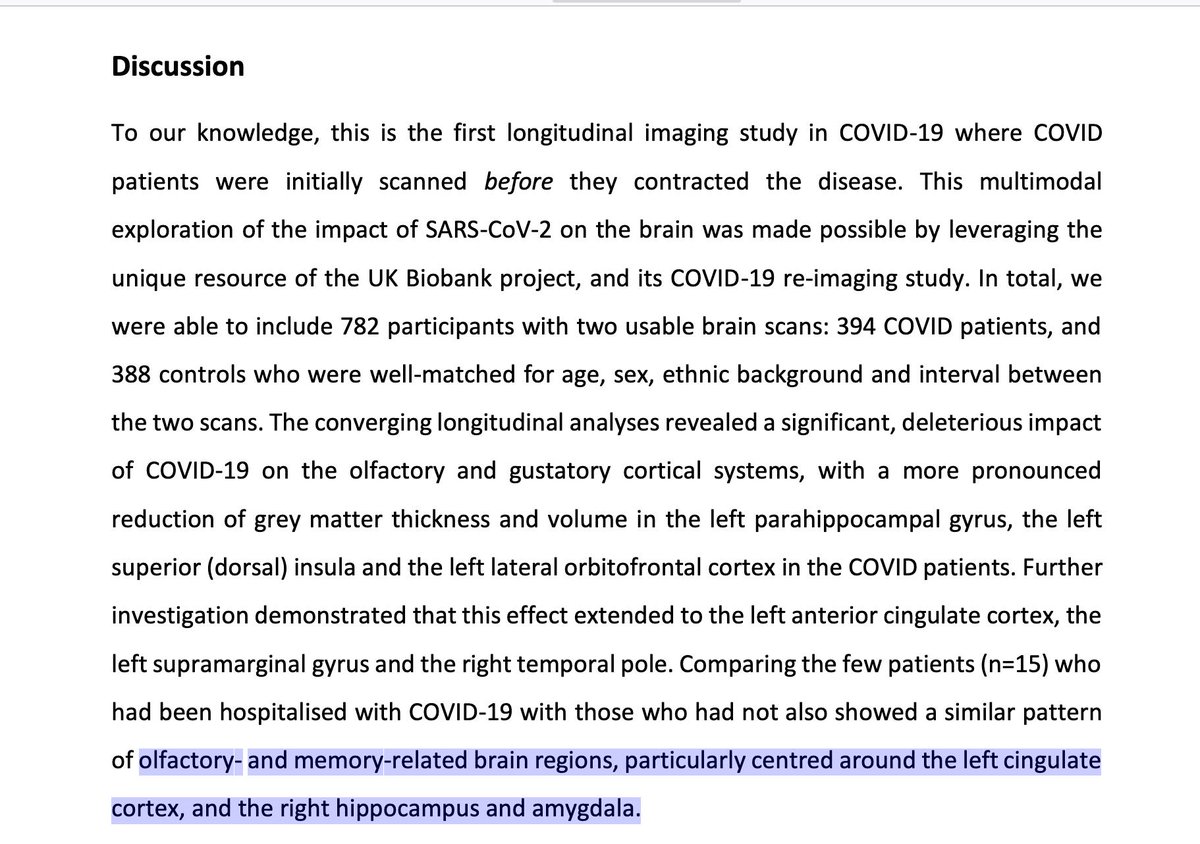
“...first longitudinal imaging study in #COVID19 where patients initially scanned before contracted the disease.” An incredibly important @uk_biobank study… 'Brain imaging before and after COVID-19 in UK Biobank’ by an esteemed group. medrxiv.org/content/10.110… @medrxivpreprint 

@uk_biobank @medrxivpreprint "significant, deleterious impact of COVID-19 on olfactory & gustatory cortical systems, w/more pronounced reduction of grey matter thickness & volume in L parahippocampal gyrus, L superior (dorsal) insula andL lateral orbitofrontal cortex in COVID patients.” #LongCovid 

@uk_biobank @medrxivpreprint Here is the kicker… of the people w/COVID for whom there are records, very few had been hospitalized. These brain effects occurred largely in largely in people not sick enough to be hospitalized. Time to re-think how benign this is in people w/o severe symptoms. Time will tell. 

@uk_biobank @medrxivpreprint Quite concerning… "The 3 main regions showing significant loss of grey matter (thickness, volume) between the 2 timepoints specifically for the COVID patients are the parahippocampal gyrus, lateral orbitofrontal cortex, and superior insula." medrxiv.org/content/10.110… #longcovid 

@uk_biobank @medrxivpreprint So this imp study is also showing that anyone who dismisses cognitive & neurological issues w/COVID, needs to think differently. This is an outstanding scientific study, by leading experts using a fantastic resource. #LongCovid @medrxivpreprint Kudos @uk_biobank & Rory Collins
@uk_biobank @medrxivpreprint And see below… "The top 10 results showing where 394 COVID patients and 388 controls differed over time are presented.” There is potential for long-term effects. An imperative to prevent the virus. And again, most of these COVID patients were not sick enough to be hospitalized. 
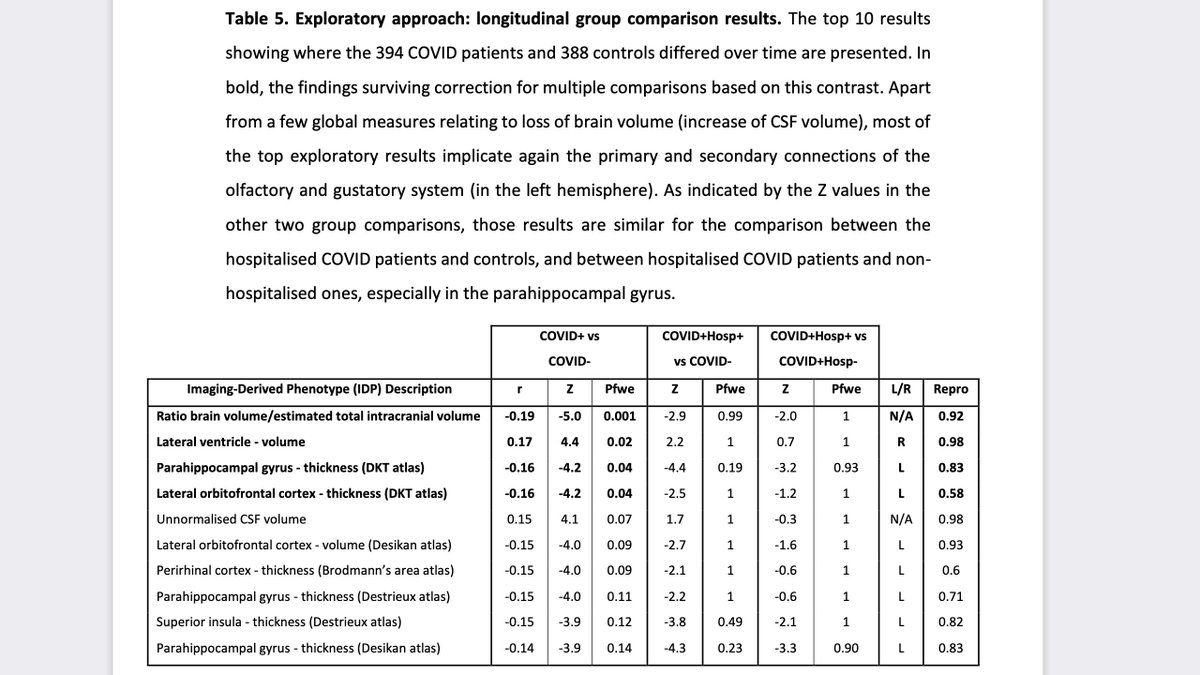
@uk_biobank @medrxivpreprint To be clear, this excellent study is showing brain efforts of COVID in people largely not hospitalized; albeit imaging changes. And the areas affected: olfactory- & memory-related brain regions” And I have seen people who seemingly have long-term memory effects. #LongCovid 
@uk_biobank @medrxivpreprint There are caveats to the study… and the changes associated with COVID are based on imaging… and there are many questions remaining. But this study is providing very useful information. And the @uk_biobank study is on-going.
@uk_biobank @medrxivpreprint And this was the most striking (concerning) figure to me...Histograms of group comparison Z statistics of longitudinal change in cortical thickness. The longitudinal effects were localized, but the effects could be seen across the entire cortical surface. Yikes. 

@uk_biobank @medrxivpreprint And it is perplexing that the strongest effects of COVID seem to have been in the left brain hemisphere… though this finding needs further validation. Is it because it is more involved in the ‘emotional aspect of olfactory memory’, as the authors opine?
@uk_biobank @medrxivpreprint And for a dark implication of the study… the authors question whether the physical proximity of the brain loss to the hippocampus might have implications for future risk of Alzheimer’s or other forms of dementia. This should give even more fuel to prevention efforts. #LongCovid
@uk_biobank @medrxivpreprint This UK study also indicates to me the importance of ever greater investment into science of COVID & #longCOVID as we seek to mitigate its consequences. Is any of it reversible? By what means? Meanwhile, folks, get your vaccinations. It's not just about averting hospitalization.
• • •
Missing some Tweet in this thread? You can try to
force a refresh