1/
WHY are steroids used for alcoholic hepatitis?
SHOULD we?
WHAT is the deal with prednisolone vs prednisone?
WHERE did the discriminant function come from?
ARE you ready for a #tweetorial
#livertwitter #medtwitter #meded #cirrhosis
WHY are steroids used for alcoholic hepatitis?
SHOULD we?
WHAT is the deal with prednisolone vs prednisone?
WHERE did the discriminant function come from?
ARE you ready for a #tweetorial
#livertwitter #medtwitter #meded #cirrhosis
2/
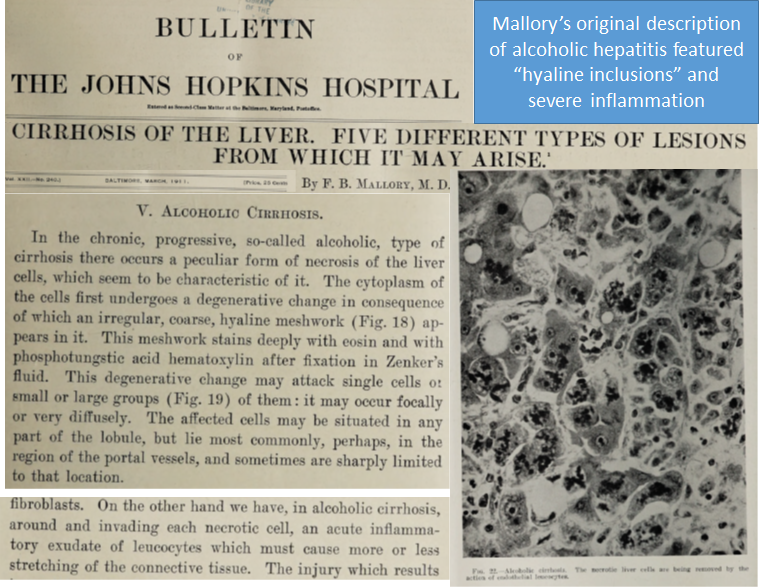
Alcoholic hepatitis is a life-threatening acute liver injury featuring a liver full of necrotic cells, "Mallory bodies" of cellular junk, & severe inflammation (neutrophils)
Fig1: Mallory's original description
Fig2: Alc hep Mortality in 1966 according to bilirubin

Alcoholic hepatitis is a life-threatening acute liver injury featuring a liver full of necrotic cells, "Mallory bodies" of cellular junk, & severe inflammation (neutrophils)
Fig1: Mallory's original description
Fig2: Alc hep Mortality in 1966 according to bilirubin

3/
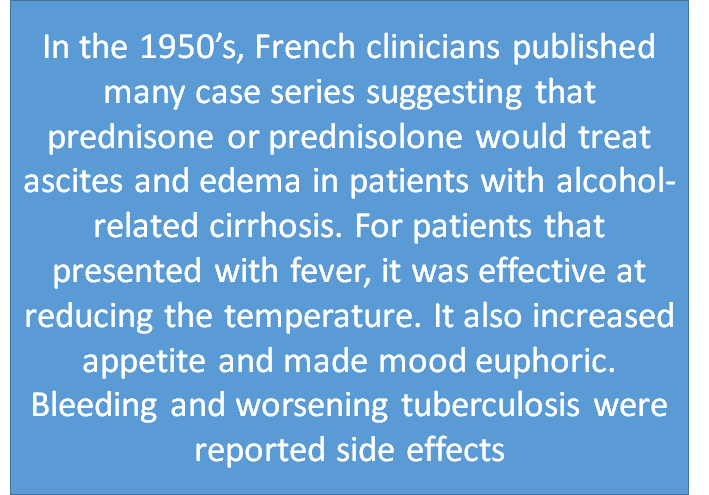
Where did we get the idea for steroids in alc hep?
Everyone in 1950's France was using steroids to treat #cirrhosis. As in the examples below, Prednisone/prednisolone were said to resolve ascites, edema, jaundice, and fevers. They made patients hungry and happy too


Where did we get the idea for steroids in alc hep?
Everyone in 1950's France was using steroids to treat #cirrhosis. As in the examples below, Prednisone/prednisolone were said to resolve ascites, edema, jaundice, and fevers. They made patients hungry and happy too


4/
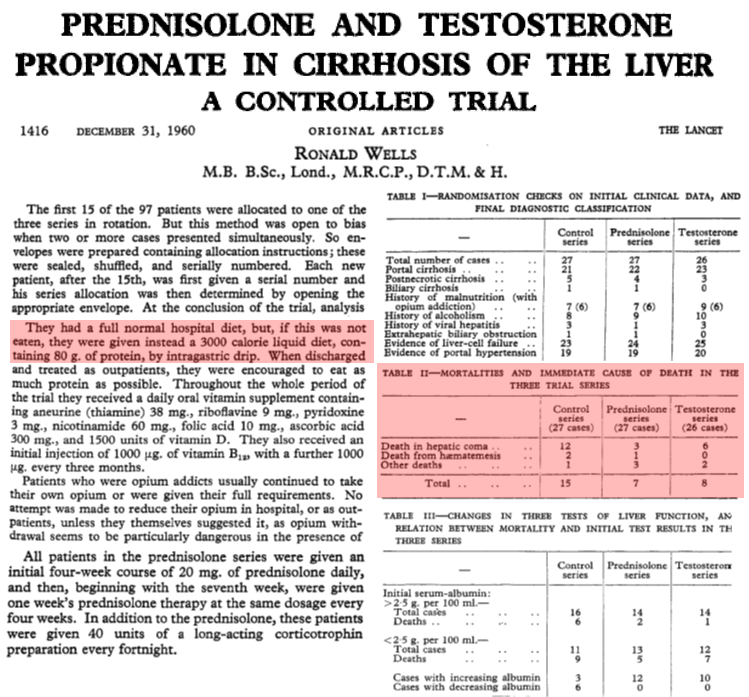
The 1st RCT
Based on the French experience, Wells published in @TheLancet an RCT of Prednisolone+Corticotrophin, Testosterone, or control for all-comers with #cirrhosis at one hospital
Corticosteroids did not⬇️ascites but they did⬇️mortality.
Steroids for all?
The 1st RCT
Based on the French experience, Wells published in @TheLancet an RCT of Prednisolone+Corticotrophin, Testosterone, or control for all-comers with #cirrhosis at one hospital
Corticosteroids did not⬇️ascites but they did⬇️mortality.
Steroids for all?
5/
Were Wells' results legit?
1⃣Helman gave prednisolone or control for #cirrhosis stratified by hepatic encephalopathy (HE). For the 14 with high bili & HE, prednisolone⬇️mortality
2⃣Porter enrolled 20 patients with biopsy-proven alc hep with a 'trend' favoring prednisolone

Were Wells' results legit?
1⃣Helman gave prednisolone or control for #cirrhosis stratified by hepatic encephalopathy (HE). For the 14 with high bili & HE, prednisolone⬇️mortality
2⃣Porter enrolled 20 patients with biopsy-proven alc hep with a 'trend' favoring prednisolone


6/
These underpowered studies got people excited about improving outcomes for alcoholic hepatitis. This field was about to take off after Willis Maddrey published his RCTs of prednisolone
But! Before we get to Maddrey, we have to ask:
why prednisolone and not prednisone?
These underpowered studies got people excited about improving outcomes for alcoholic hepatitis. This field was about to take off after Willis Maddrey published his RCTs of prednisolone
But! Before we get to Maddrey, we have to ask:
why prednisolone and not prednisone?
7/
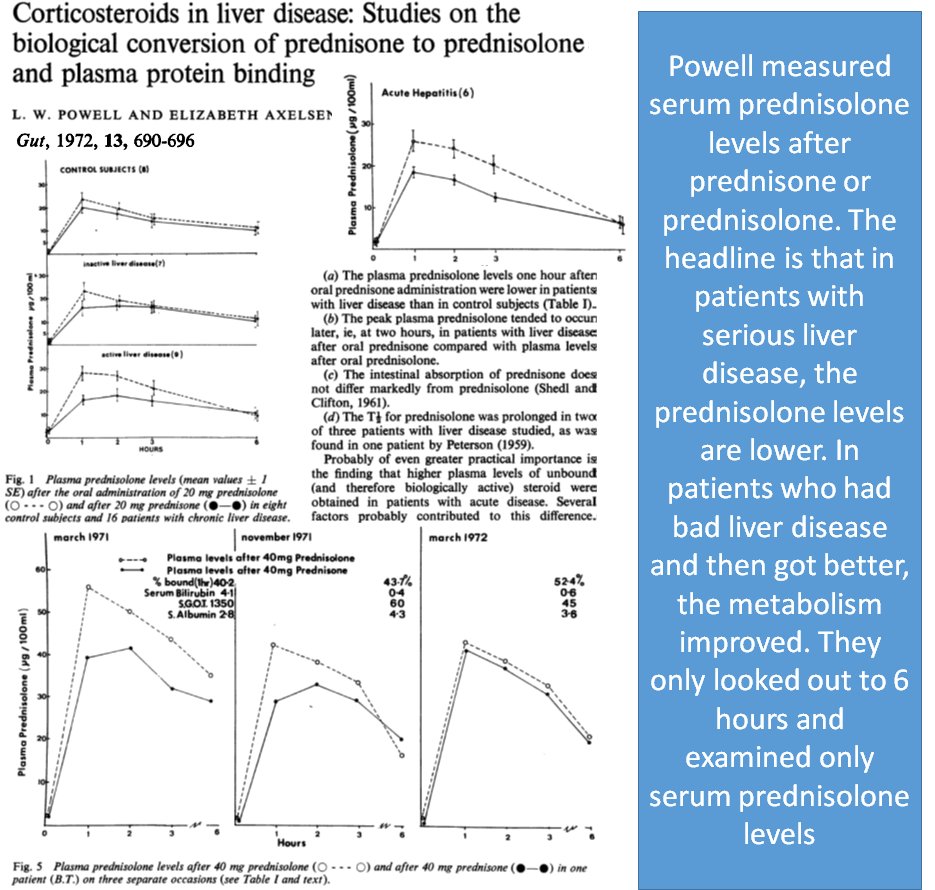
Prednisone is a prodrug converted to prednisolone by 11β-HSD1 enzyme, which is mainly in liver. Given the new interest in steroids for alc hep, Powell looked at metabolism and found conversion of prednisone to prednisolone was⬇️in liver injury
Case closed...or is it?
Prednisone is a prodrug converted to prednisolone by 11β-HSD1 enzyme, which is mainly in liver. Given the new interest in steroids for alc hep, Powell looked at metabolism and found conversion of prednisone to prednisolone was⬇️in liver injury
Case closed...or is it?
8/
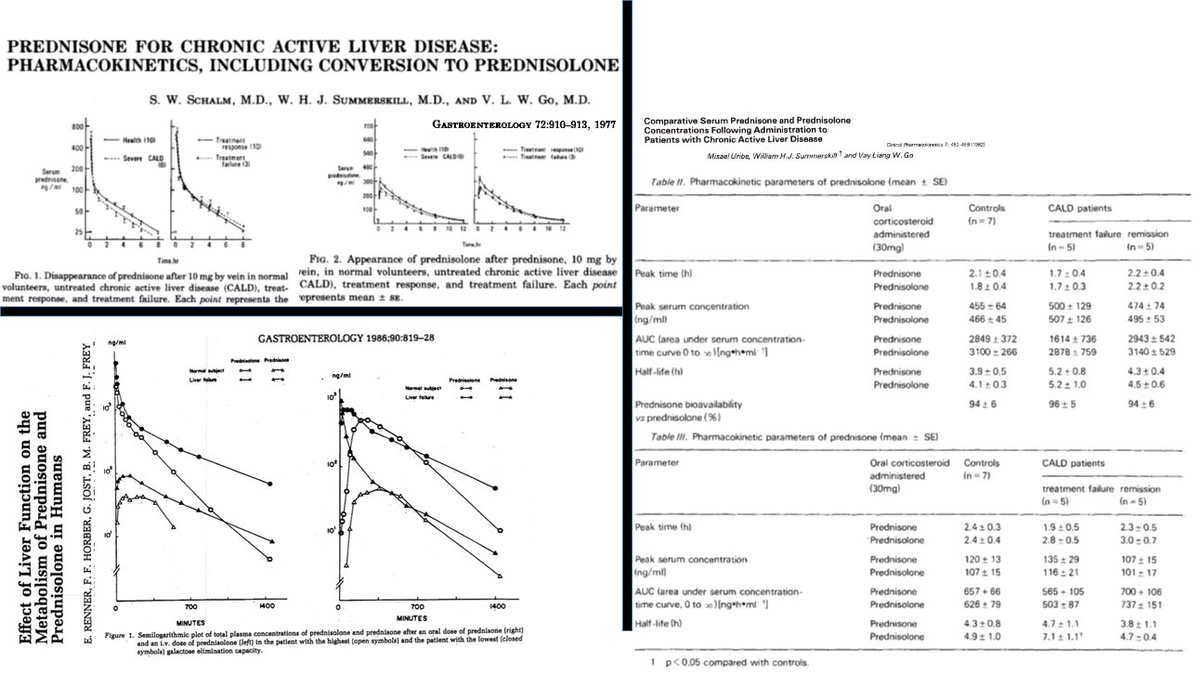
Turns out: pred=pred
1⃣Powell's findings were irreproducible
2⃣Prednisone is just converted more slowly in liver disease. Also 11β-HSD1 is in muscle, fat
3⃣Prednisone/prednisolone have equal bioavailability
4⃣Treatment failure is unrelated to pred metabolism
Turns out: pred=pred
1⃣Powell's findings were irreproducible
2⃣Prednisone is just converted more slowly in liver disease. Also 11β-HSD1 is in muscle, fat
3⃣Prednisone/prednisolone have equal bioavailability
4⃣Treatment failure is unrelated to pred metabolism
9/
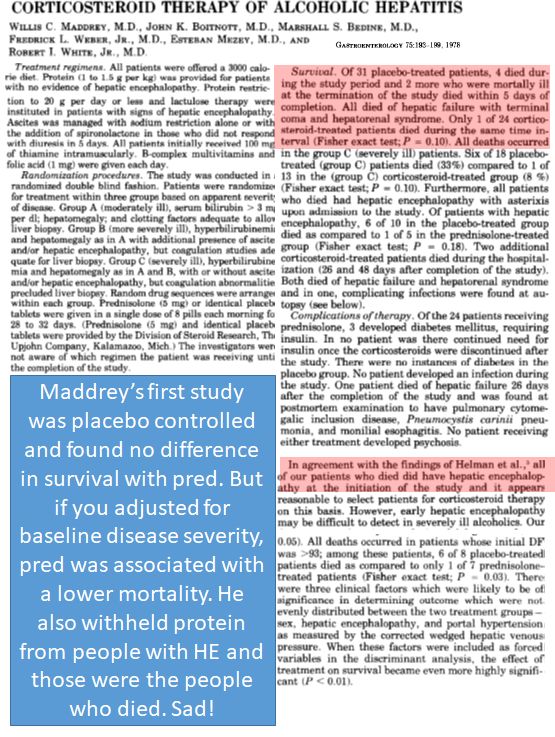
Enter Maddrey
Although we learned prednisone=prednisolone, Maddrey enrolled 55 pts in a prednisolone RCT after the Powell's 1971 study
😢No survival benefit from steroids
🧐But wait, when you adjust for disease severity, prednisolone came out on top. How? Next slide pls
Enter Maddrey
Although we learned prednisone=prednisolone, Maddrey enrolled 55 pts in a prednisolone RCT after the Powell's 1971 study
😢No survival benefit from steroids
🧐But wait, when you adjust for disease severity, prednisolone came out on top. How? Next slide pls
10/
Introducing the Discriminant Function (DF)
Using stepwise regression, Maddrey found all ppl who died had 96+ using: 4.6 x prothrombin time x bilirubin
For a multicenter trial, he updated the DF (subtracting normal PT) & only included people with DF>32 (or HE)

Introducing the Discriminant Function (DF)
Using stepwise regression, Maddrey found all ppl who died had 96+ using: 4.6 x prothrombin time x bilirubin
For a multicenter trial, he updated the DF (subtracting normal PT) & only included people with DF>32 (or HE)


11/
In a multicenter RCT with 66 patients who had DF>32 (or HE), prednisolone was associated with a major reduction in mortality. These results were confirmed in a trial of 61 patients from France
Both prednisolone and the DF were looking like they were here to stay

In a multicenter RCT with 66 patients who had DF>32 (or HE), prednisolone was associated with a major reduction in mortality. These results were confirmed in a trial of 61 patients from France
Both prednisolone and the DF were looking like they were here to stay


12/
Since those landmarks, many trials have been undertaken
1⃣Prednisolone has been mostly used; out of convention, not b/c it's >prednisone
2⃣we tried many other treatments, eg pentoxifylline, thought to⬇️tnf
3⃣All results have been conflicting
Then came STOPAH
Since those landmarks, many trials have been undertaken
1⃣Prednisolone has been mostly used; out of convention, not b/c it's >prednisone
2⃣we tried many other treatments, eg pentoxifylline, thought to⬇️tnf
3⃣All results have been conflicting
Then came STOPAH
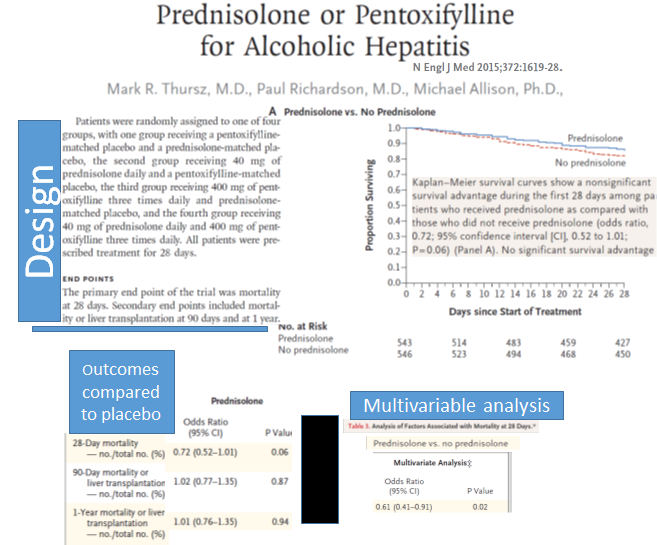
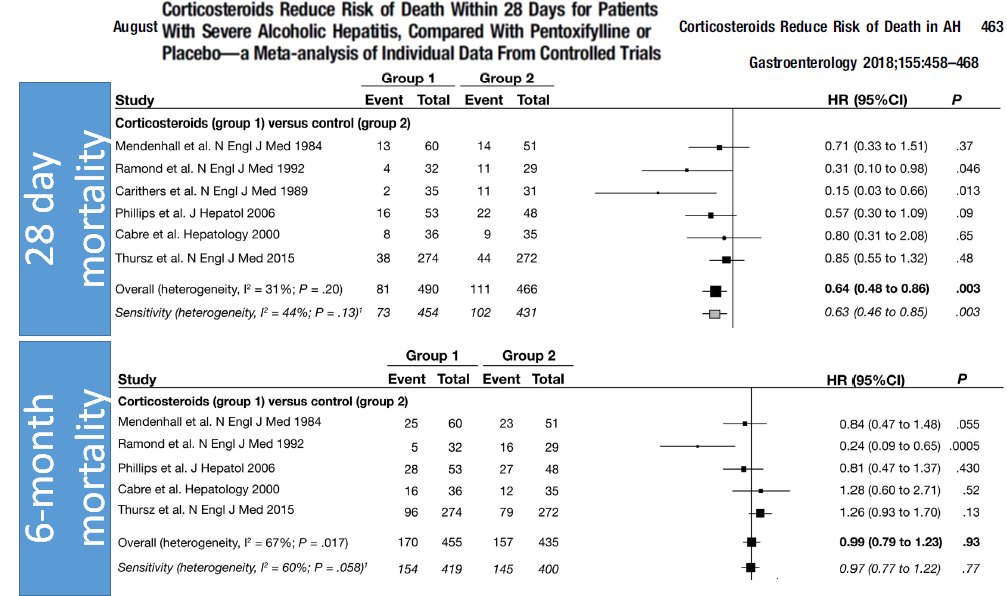
13/
STOPAH was:
1⃣The largest Alc hep RCT
2⃣2x2 factorial: pred, pentox, placebo
STOPAH found:
3⃣🚫improved survival at 90, 365 days
4⃣Possible⬆️survival at 28d for pred
Conclusion
🪦pentoxifylline
🤔use steroids carefully, if at all
(Confirmed by meta-analysis)

STOPAH was:
1⃣The largest Alc hep RCT
2⃣2x2 factorial: pred, pentox, placebo
STOPAH found:
3⃣🚫improved survival at 90, 365 days
4⃣Possible⬆️survival at 28d for pred
Conclusion
🪦pentoxifylline
🤔use steroids carefully, if at all
(Confirmed by meta-analysis)
14/
What else did STOPAH show?
28d mortality was 17% in the placebo group (13-14% in the pred groups). We have far to go but we have come a LONG way!
Why? Better supportive care, eg:
1⃣nutritional support
2⃣Screen/treat for infection
3⃣Endoscopy for bleeding

What else did STOPAH show?
28d mortality was 17% in the placebo group (13-14% in the pred groups). We have far to go but we have come a LONG way!
Why? Better supportive care, eg:
1⃣nutritional support
2⃣Screen/treat for infection
3⃣Endoscopy for bleeding


15/
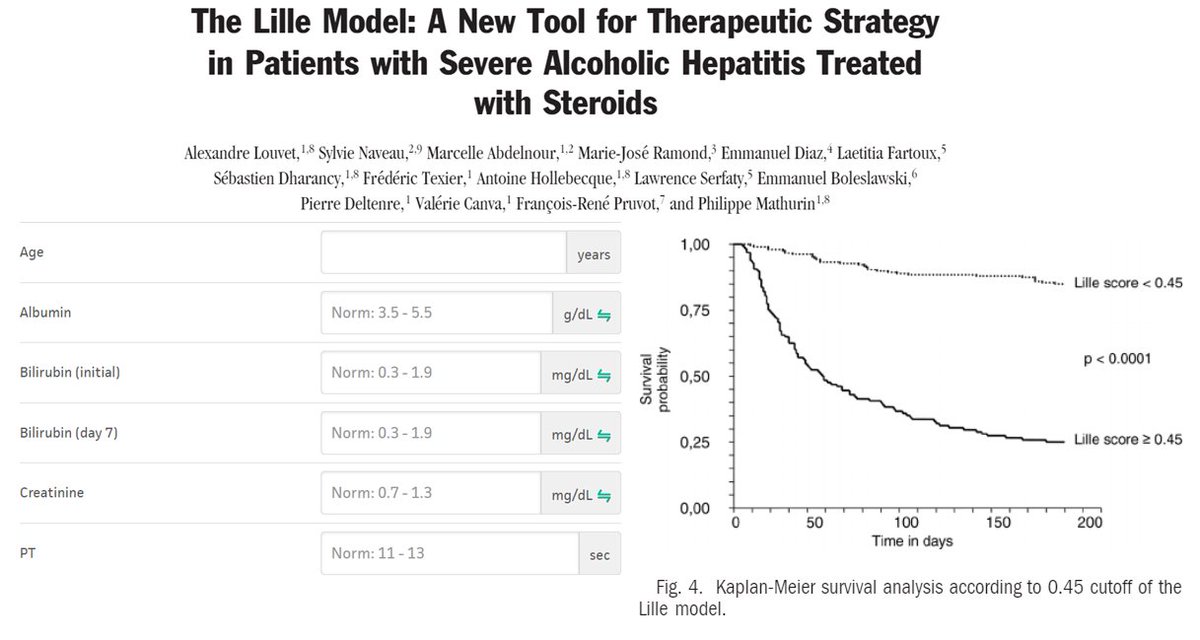
Where are we at with DF these days?
1⃣If we choose pred using DF, we only want 2 use in ppl who r benefitting by ~ day 7 (i.e. Lille score)
2⃣MELD score may be better than DF for prognosis at baseline; MELD + Lille for pred users
3⃣If pred has benefit, it's in MELD 25-39


Where are we at with DF these days?
1⃣If we choose pred using DF, we only want 2 use in ppl who r benefitting by ~ day 7 (i.e. Lille score)
2⃣MELD score may be better than DF for prognosis at baseline; MELD + Lille for pred users
3⃣If pred has benefit, it's in MELD 25-39


16/
SUMMARY
1⃣Pred was used to treat #cirrhosis but trials showed only ppl with alc hep may benefit
2⃣Prednisone➡️prednisolone. Bioavailability is the same
3⃣The DF was associated w/death & then used 2 select pts 4 trials
4⃣Pred may⬆️28-day but not longterm survival
SUMMARY
1⃣Pred was used to treat #cirrhosis but trials showed only ppl with alc hep may benefit
2⃣Prednisone➡️prednisolone. Bioavailability is the same
3⃣The DF was associated w/death & then used 2 select pts 4 trials
4⃣Pred may⬆️28-day but not longterm survival
/end
This concludes a #tweetorial on the use of steroids for patients with alcohol-associated hepatitis. I hope you enjoyed. I would like to thank @BloomPringle for peer-review and thank those whose work benefits patients with AH like J `Mellinger, @MarkThursz, and Maddrey
This concludes a #tweetorial on the use of steroids for patients with alcohol-associated hepatitis. I hope you enjoyed. I would like to thank @BloomPringle for peer-review and thank those whose work benefits patients with AH like J `Mellinger, @MarkThursz, and Maddrey
• • •
Missing some Tweet in this thread? You can try to
force a refresh













