
We’ve seen how to measure VTI and stroke volume with #ultrasound
Our next #FUSIC haemodynamic question brought to you by @icultrasonica, @wilkinsonjonny and I is:
Q2. Does SV respond to fluid, vasopressors or inotropes?
#echofirst #POCUS #haemodynamics #foamed
Our next #FUSIC haemodynamic question brought to you by @icultrasonica, @wilkinsonjonny and I is:
Q2. Does SV respond to fluid, vasopressors or inotropes?
#echofirst #POCUS #haemodynamics #foamed

In Q1 we saw how to measure stroke volume (SV). Q2 helps us manage someone with an inappropriately low SV. Pressors, fluids and inotropes are all treatment options. If If used correctly, they will ↑SV. If not, they won’t, and they may even be harmful.
https://twitter.com/ICUltrasonica/status/1407111542814957575?s=20
Measuring VTI before and after each of these interventions will therefore easily show you if they have worked. But can we predict which one is likely to work before we give drugs or a drop of fluid? 1st, let’s go back to some physiology.
Venous return (VR) is determined by mean systemic pressure (Pms) minus right atrial pressure (Pra). Pms is dependent on the volume & compliance of the venules. The heart can only keep Pra low & accept ↑VR from ↑Pms if it not badly failing.
player.vimeo.com/video/545386872
player.vimeo.com/video/545386872
A dilated, poorly functioning LV or RV (stay tuned for Q8) or high left atrial pressure (Q7) make it unlikely pressors or fluids will increase SV. Fluid will make things worse via capillary leak & venous congestion (Q10). Pressors may over constrict & impair peripheral perfusion
Low Pms has a number of features with ultrasound. A reasonable starting point is size. A small, hyperdynamic LV (end diastolic area in PSAX of <10cm2 or kissing papillary muscles) & an IVC diameter of <1cm suggest SV will be responsive to increasing Pms.
Heart-lung interactions are also predictive. Ventilation induces cyclical changes in intrathoracic pressure which causes alterations in SV. Back to some physiology….
In mechanical ventilation, a +ve pressure breath reduces VR (↑impedance via ↑Pra) & increases RV afterload causing reduced RV SV. After the pulmonary transition time the LV receives less blood and SV falls. LV SV thus cyclically changes with ventilation. 
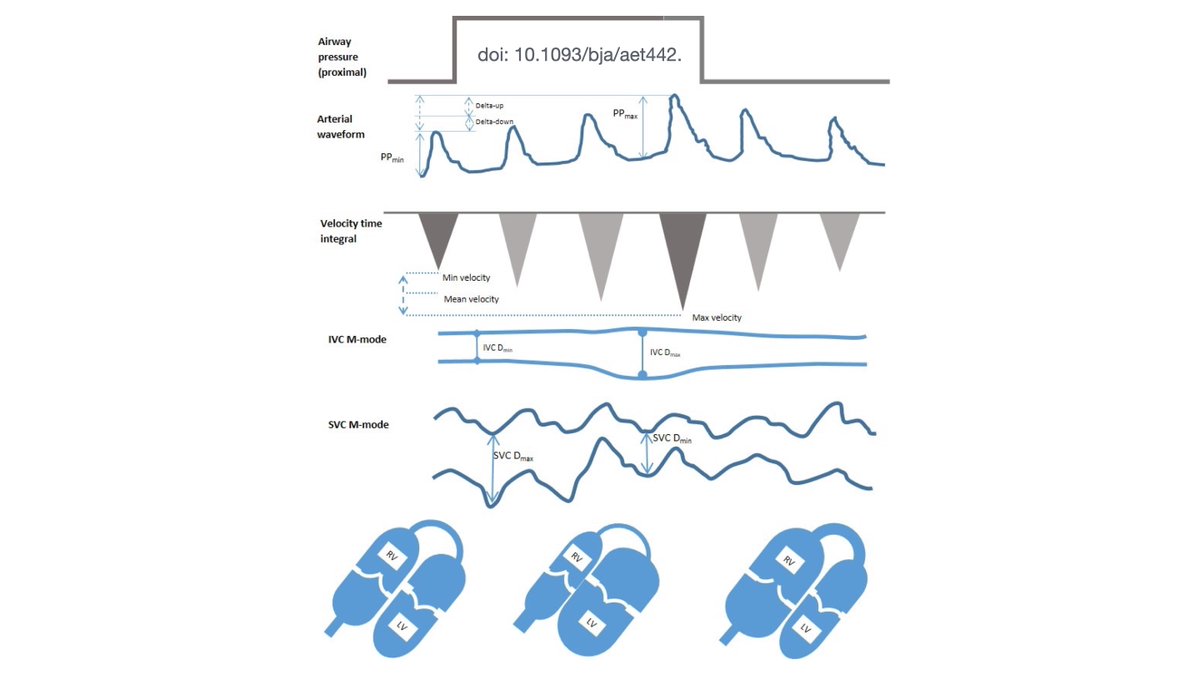
This effect is exaggerated if VR to the RV is low (↓Pms) as impedance will have a greater effect and the ventricles are on the steep part of the starling curve.
Large changes in SV with +ve pressure ventilation therefore predict preload responsiveness
Large changes in SV with +ve pressure ventilation therefore predict preload responsiveness
See how this patient’s VTI varies between 8.1 and 11.4, representing a 33% variation (using VTImean as the denominator). The sweep speed allows a whole respiratory cycle to be seen while keeping the VTI wide enough to measure accurately 

Peak velocity variation (Vmax) is easier to measure than VTI. This patient has a 21% variation in Vmax. A faster sweep speed has been used here to show >1 respiratory cycle. As we measuring Vmax it doesn’t matter that the VTI is narrow. 
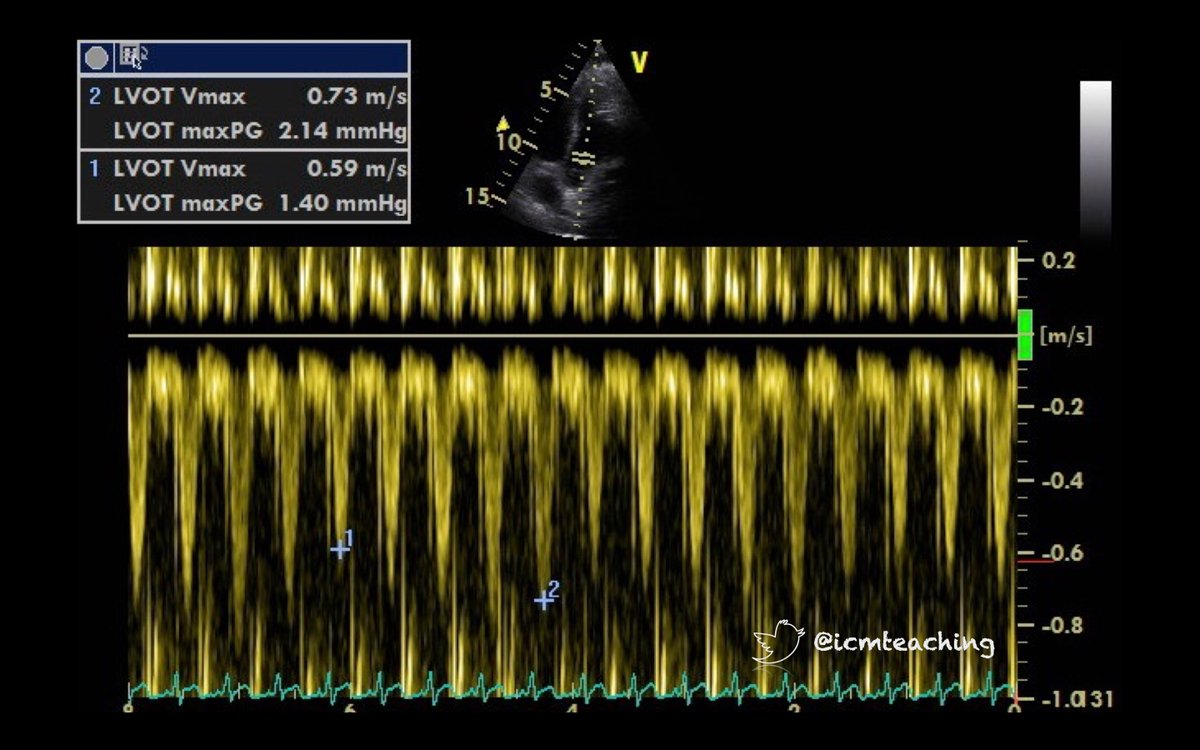
VTI and peak velocity variation of >14% have been shown to be strong predictors of preload responsiveness. However, the patient from which these images were from was not fluid responsive (the SV did not increase with a fluid challenge). So why not?
1st, there are a number of pre-conditions to assessing respiratory variation - sinus rhythm, mechanical ventilation with no spontaneous effort, tidal volumes of ≥8mls/kg, normal intra-abdominal pressure and an intact thorax are all required.
2nd, heart failure will produce false positives. In RV failure the ↓VR and ↑afterload from a positive pressure breath will be exaggerated (known as dDown). In LV failure a positive pressure breath reduces LV afterload improving its output (dUp). Echo of above patient
So, these cyclical changes will only predict preload responsiveness in a limited range of circumstances. Heart-lung interactions have in fact been shown to be of only very limited usefulness in predicting preload responsiveness in real world patients
pubmed.ncbi.nlm.nih.gov/24374504/
pubmed.ncbi.nlm.nih.gov/24374504/
The change in IVC diameter with invasive ventilation can also be used to predict preload responsiveness but has the same caveats as LVOT measurements so is equally limited in the real world. 

More information on assessing fluid responsiveness can be found in this @BSEcho article
ncbi.nlm.nih.gov/pmc/articles/P…
ncbi.nlm.nih.gov/pmc/articles/P…
Usually then we need to ‘challenge’ the patients SV. As already stated, the ultrasound signs of a low Pms do not tell you whether this if from from hypovolaemia or vasodilatation. Each require very different treatment. As with all ultrasound, clinical correlation is key…
…In a patient with sepsis or pancreatitis a rational approach would be to try a vasopressor 1st. In a patient with bleeding or GI losses a fluid challenge would be 1st line.
A passive leg raise gives a reversible fluid challenge by mobilising around 300mls of blood. An increase in VTI >15% demonstrates a +ve response. The change in position can make VTI measurement challenging. We can also give an IV fluid bolus of 100-250mls.
https://twitter.com/jackdeliuc/status/1404518089094569989?s=20
It is important to remember that a +ve response to IV fluid must be sustained for >30 mins for it to mean hypovolaemia was present (without ongoing bleeding).
A vasodilated patient will often respond transiently to fluid via increased Pms, but if there is not hypovolaemia most of the fluid will redistribute to the tissues in <60minutes and Pms, VR & SV will then fall
If there is a low Pms from vasodilatation, a vasopressor will increase Pms, VR and SV. If it does not then it suggests maximal vasoconstriction already (e.g hypovolaemia) or ventricular failure (the heart is unable to accept more VR)
In a failing heart which cannot accept any more VR, increasing Pms with pressors will not ↑ SV. This is where we can assess the VTI response to starting an inotrope. Improved efficiency will allow the heart to accept more VR and ↑ its SV. It may become vasopressor responsive
Remember - a low SV can be multifactorial (heart failure and vasodilatation). Clinical integration is KEY. Perform the most rational intervention and assess the response.
See the full #FUSIC HD article
doi.org/10.1177%2F1751…
See the full #FUSIC HD article
doi.org/10.1177%2F1751…
• • •
Missing some Tweet in this thread? You can try to
force a refresh



