It is often said that Marie Skłodowska-Curie died of "aplastic anemia." Try Googling it; you'll find many hits. But I am not so sure. She died on July 4th, 1934, at a sanatorium called Sancellemoz, in Passy, Haute-Savoie, France, after a long illness. #aplasticanemia #MDS /1
https://twitter.com/NobelPrize/status/1411703123501064194
The 1937 biography by her younger daughter Ève describes her final illness, including a consultation at Sancellemoz (postcard) by a "Professor Roch." That would have been Maurice Roch, Regent of @UNIGEnews & father of famous Alpinist André Roch who planned Aspen, Colorado./3 



Here is how the daughter's biography describes that consultation. Mention is made of fevers and blood tests - rapidly falling WBC & RBC counts - and that X-rays were done. (The last thing she needed: more radiation!). Diagnosis: "Pernicious anaemia in its extreme form." /3 

It is unclear if Mme. Sklodowska-Curie underwent a marrow biopsy. The @nytimes ran her obituary the following day, and stated her cause of death as "a form of pernicious anaemia". (Interesting to see @Wimbledon 🎾 scores next to the obituary - it was July 4th week after all.)/4 

Aplastic anemia was well recognized by 1934. It had first been described in 1888 at autopsy in a 21 year-old pregnant woman named Hedwig S. with “strikingly hypocellular” marrow - by Paul Ehrlich at Charite in Berlin, in this case report./5 



The term "aplastic anemia" is usually said to have been coined in 1904 by this guy: Anatole Chauffard in Paris. The key paper was "Un cas d’anémie pernicieuse aplastique" in the Bulletin Soc Med Hop Paris, 21 (1904): 303f. But... notice the "pernicious" in the paper's title./6 

Richard Clarke Cabot in Boston (depicted - he started the clinicopathological case series in @NEJM) summarized 24 cases of aplastic anemia the 1908 version of text, emphasizing hypocellularity. If Mme Curie had #aplasticanemia we might have expected Roch to give that diagnosis./6 



(BTW: back then people reported *original* research in textbooks! Osler's 1892 first edition of his Principles and Practice text is packed with his own unpublished observations. Now, of course, textbooks are so long in gestation that anyone who tried that would get 'scooped'.)/7
In contrast to aplastic anemia, myelodysplastic syndromes were not yet well described in 1934. "Refractory anemia" term dates to a 1938 paper by the notorious C.P. "Dusty" Rhoads. I summarized some of that history in a 2012 Leukemia Research paper./8 sciencedirect.com/science/articl…
Since pernicious anemia is associated with blood/marrow cell dysmorphology, as in these 2 @ASH_hematology image bank photomicrographs, and the megaloblastic changes in pernicious anemia overlap with findings in #MDS, many early MDS cases were mistaken for pernicious anemia./9 



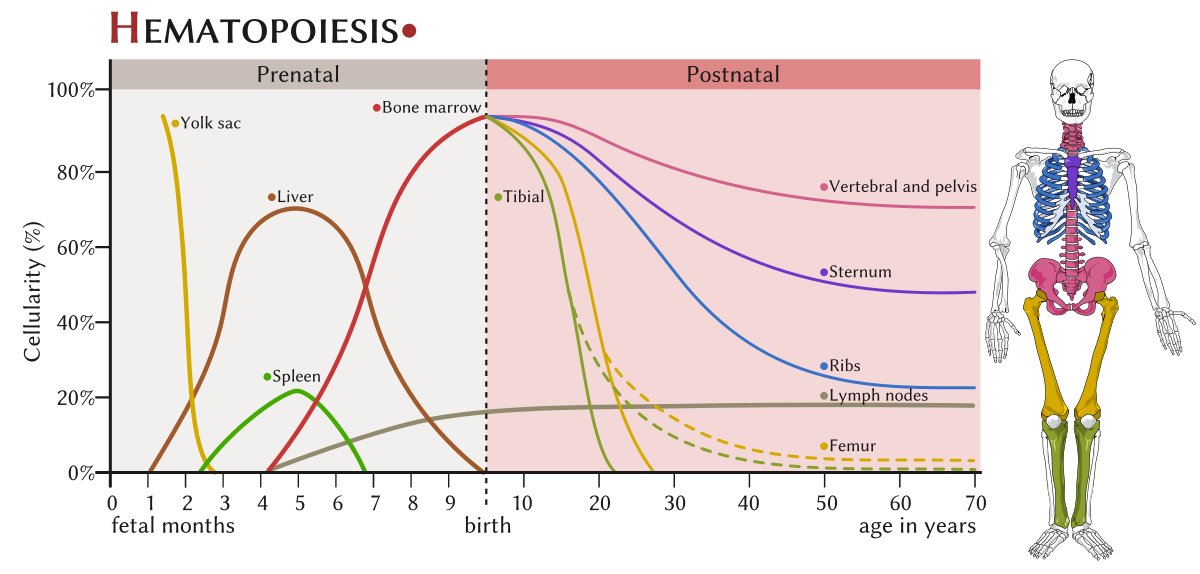
Aplastic anemia induced by ionizing radiation is often (albeit not always) the result of a single large myeloablative dose. Therapy- or exposure-related MDS, in contrast, has a different epidemiology and may result from lower dose chronic exposure./10 ashpublications.org/hematology/art…
Mme. Curie died at age 66 & had many years of lower-dose exposures to various radioisotopes./11 history.aip.org/exhibits/curie…
Already in 1920 the health effects of radium in particular were well recognized. Mme. Curie wrote to her sister Bronya in 1920, "“Perhaps radium has something to do with these troubles, but it cannot be affirmed with certainty.” "Radium Girl" lawsuits began in the 1920s./12 

So while it is not impossible for Marie Skłodowska-Curie to have died of aplastic anemia, as the Nobel Foundation tweeted yesterday, MDS, or another chronic myeloid neoplasm (MF is unlikely given lack of mention of a spleen), or even actue leukemia are more likely. /End
• • •
Missing some Tweet in this thread? You can try to
force a refresh